Abstract
Study design
Retrospective review of data from a prospective database of a Level 1 trauma center.
Objectives
This project aims to identify factors collected during the acute and rehabilitative care following a traumatic spinal cord injury (TSCI) associated with success and failure to return home after inpatient intensive functional rehabilitation (IFR).
Setting
Level 1 trauma center specialized in TSCI care in Montreal, Canada.
Methods
All eligible patients from our prospective database were separated into two groups according to discharge destination following IFR. Clinical variables collected during the acute and rehabilitative care as well as demographic variables were compared between patients who managed to return home (Group 1) and those who were discharged elsewhere (Group 2). Multivariable regression analyses were conducted with variables that were significant at the univariate level.
Results
Out of the 193 patients included, 22 (11%) failed to return home following IFR. Six variables were associated with failure to return home at the univariate level: longer acute length of stay (LOS), longer rehabilitation LOS, living alone, higher neurological level of injury, having comorbidities, and having a pressure injury (PI) during acute care. Three variables remained significant at the multivariate level: living alone, increasing acute LOS and presenting a high cervical (C1-C4) neurological level of injury.
Conclusions
It is important that acute care clinicians recognize the aforementioned factors early after TSCI in order to optimize patients for community reintegration.
Similar content being viewed by others
Introduction
Following a traumatic spinal cord injury (TSCI), discharge destination is a major determinant of post-injury quality of life (QoL) and social reintegration [1,2,3,4]. In fact, compelling evidence clearly indicates that when possible, ensuring patients be discharged home from the inpatient setting is critical to avoid the hindering obstacles to satisfactory QoL that are associated with daily living in long-term care facilities [2, 3]. Since patients who reintegrate the community and their significant others also perceive higher levels of QoL and social participation as compared with their institutionalized counterparts [1], it is clear that maximizing the number of home discharges after TSCI is both a clinical and research objective of paramount importance. Often in hopes of doing so, patients are usually transferred from acute care to specialized inpatient functional rehabilitation (IFR) facilities—which have been shown to increase odds of successful home discharge up to sixfold compared to standard unspecialized rehabilitation facilities [5]. However, despite these IFR programs and the important associated investments [6], around 10% of patients are still discharged to locations other than home [5, 7], where previously cited data clearly demonstrate they enjoy reduced QoL.
Beyond the important role of subsequent IFR to improve the discharge outcomes, the impact of the acute care for facilitating return home after TSCI has never been studied thoroughly [7, 8]. By studying the outcomes of rehabilitation care, Whiteneck et al. [7] identified different factors associated with better odds of being discharged home following IFR, including younger age, being married, improved functional status upon IFR admission, improved IFR care, and lesser severity of illness. However, Whiteneck et al. [7] only investigated rehabilitation care, such that there was no analysis of variables from the acute care. A study from Anzai et al. [9] also reported factors associated with discharge destination following IFR, without considering variables characterizing the acute care.
In view of the paucity of data concerning the potential role of the acute care on discharge destination after TSCI, the objective of this study was to identify factors collected during the acute and rehabilitative care associated with success and failure to return home after IFR. This study will thus allow early identification of important variables during the acute care to eventually increase the number of successful home discharges.
Methods
Patients
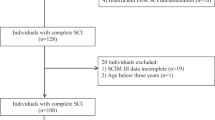
A prospective cohort of patients who were admitted to a level 1 SCI-specialized trauma facility for a TSCI between April 2010 and January 2019 was considered. Included patients were TSCI patients over 17 years of age who had been transferred to a specialized IFR facility on discharge from the acute care setting and for whom complete datasets were available (n = 209). The main exclusion criteria were: (1) living in an institutional setting (i.e., not in a private residence) prior to the injury, (2) presenting an outlying dataset, (3) having been readmitted in acute care during the first year following final discharge if destination was home (as this was considered to be a distinct subgroup of patients (n = 9) for whom complete success in reintegrating their prior residence could be controversial), and (4) penetrating injury as mechanism of TSCI. A total of 193 patients were therefore eligible for final analysis and included in this study. All patients were recruited prospectively on a voluntary basis in the acute care setting and proper consent was always obtained shortly after admission to acute care. The consent rate to participate in the prospective database fluctuated around 75% between 2010 and 2019. All patients were treated surgically based on the clinical needs determined by the attending spine surgeon. Despite variations in techniques and approaches, all surgical interventions consisted in spinal decompression, instrumentation, and fusion. Following acute hospitalization, all patients were transferred from the acute care institution to the same rehabilitative institution specialized in SCI for inpatient IFR. To be eligible for this transfer, patients had to meet several criteria after multiple assessments by the attending team consisting of a spine surgeon, physiatrist, physical therapist, occupational therapist, and liaison nurse. To be transferred to IFR, patients had to (1) be medically stable (which encompasses stable vital signs, medical condition and comorbidities) and present no impending risk of deterioration, (2) show no need for additional investigations, (3) have an established follow-up plan, (4) present no new and/or emergent treatment planned for the next 7 days, (5) display the physical and cognitive capability to undergo 60 min of rehabilitative therapy daily, and (6) require no parenteral nutrition. To meet these criteria in a timely manner, in our institution, patients participate in rehabilitation-oriented therapies during their acute hospitalization. These aim mostly at preventing complications and conditioning their body for subsequent IFR with regular physiotherapy aimed at increasing strength, joint mobility, endurance, and postural control [10]. Upon arrival to the IFR facility, patients are initially assessed by a multidisciplinary team consisting of a physiatrist, a physical therapist, an occupational therapist, a social worker, a psychologist, and a nurse to determine their personalized objectives. While these can vary from patient to patient, the focus is always on maximizing functional recovery and managing successful community reintegration through and intensive rehabilitation protocol specifically tailored to the patient’s needs and abilities. It is only when the patient has reached all said goals or when the patient shows inability to pursue treatments, changes their objectives or withdraws consent that IFR rehabilitation is ceased and patients are discharged [11].
Another important specification is that for all patients who remained for analysis, if a tracheotomy was performed during the acute hospitalization (n = 8; 6 who were discharged home, 2 who were not discharged home), they were weaned from it before discharge from IFR.
This study was approved by our institutional ethics committee.
Dependent variable
Two groups were defined based on the destination upon discharge from IFR collected prospectively by the rehabilitative institution. Group 1 consisted in patients who were discharged home following IFR and group 2 included those who were not discharged home following IFR. Patients who were not discharged home were either directly transferred to a nursing home or long-term care facility, or they were sent to an inpatient transition care institution with the intention of imminent placement in a nursing home or long-term care facility once administrative obstacles would be cleared. The decision to opt for transfer to a long-term care facility or a nursing home was made by a multidisciplinary team following weeks of observation of the patient’s evolution throughout the rehabilitation process.
Independent variables
Sociodemographic and acute clinical information were collected prospectively during the acute care. The clinical data of rehabilitation care were similarly collected by the rehabilitation institution. The selection of potential predictors was based on their clinical significance, the availability of data and on the literature [5, 7, 9]. Clinical significance was determined by the authors with relevant clinical expertize: a spine surgeon (JMMT) and a physiatrist specialized in TSCI patients (ARD). Ultimately, the variables studied were: sex (male or female), body mass index at admission (BMI; <30 or ≥30), pre-injury living arrangement (living with someone—including living with a spouse, family member, non-family—or living alone), surgical delay (<24 or ≥24 h following the TSCI), injury severity score (ISS) [12], pre-injury Charlson Comorbidity Index (of 0 or 1+) [13], acute length of stay (acute LOS), rehabilitation length of stay (rehabilitation LOS), occurrence (yes or no) of complications (subcategorized as urinary tract infections, pneumonia, pressure injury, and other complications) during acute care, and age at injury (<65years or ≥65years). The latter was dichotomized to study the subpopulation of elderly patients as they are defined by the World Health Organization [14]. The neurological level of injury and the Asia Impairment Scale grade (dichotomized as motor-complete AIS grades A-B or motor-incomplete AIS grades C–D) were assessed within 72 h of the injury by a single physiatrist using the International Standards for the Neurological Classification of Spinal Cord Injury [15]. Neurological levels of injuries were grouped in five categories: C1-C4, C5-C8, T1-T8, T9-L1, and L2-S2.
For all continuous independent variables (ISS, acute LOS, and rehabilitation LOS), outliers were defined as individuals presenting values outside of three standard-deviations from average. As specified earlier, all identified outliers were excluded.
Statistical analyses
Analyzes of the independent variables were conducted to compare the characteristics of patients who succeeded in returning home (Group 1) to those of patients who failed to do so (Group 2). Descriptive statistics were first obtained to characterize the two groups. Continuous variables (ISS, acute LOS, and rehabilitation LOS) were reported as means and standard deviations while categorical variables were reported as proportions expressed in percentage. Univariate analysis (bilateral Student t tests for continuous variables and Chi-square tests for categorical variables) allowed to identify significant differences between variables in the two study groups. A backward stepwise linear regression was finally conducted with variables that were significant at the univariate level. Categorical variables with more than 2 levels were appropriately dummy coded before they were input in the multivariate analyses. All statistical testing was performed on IBM SPSS Statistics v.25 (Chicago, IL). The level of significance was set at 0.05 for all tests.
Results
From 209 patients included in this study, 9 were excluded because they were re-hospitalized within the first year following the TSCI and an additional 7 were excluded because they presented an outlying dataset. The final cohort thus comprised a total of 193 patients. The group of patients who were discharged home following rehabilitation (Group 1) included 171 patients (89%) while the remaining 22 (11%) constituted the group of patients who were not discharged home (Group 2). Among these 22 patients, 10 were directly transferred to a nursing home, 4 were sent to long-term care and 8 were sent to a transitional inpatient setting before final discharge to either a nursing home or a long-term care facility. As shown in Table 1, patients who were not discharged home following IFR presented significantly longer acute LOS (mean (SD) difference of 22 (4.3); P < 0.01) and rehabilitation LOS (mean (SD) difference of 19 (8.1); P = 0.02) than patients who were discharged home. In addition, patients who were not discharged home were more likely (1) to live alone prior to the accident (50% vs 19%; P ≤ 0.01), (2) to have a neurological level of injury between C1 and C4 (73% vs 30%, P < 0.01), (3) to present at least one pre-existing comorbidity upon admission to acute care (77% vs 50%; P = 0.02), and (4) to have developed a pressure injury during acute care (45% vs 16%; P < 0.01). Finally, patients who were not discharged home tended to be more likely to be aged 65 years and older, to be female, to present an A or B AIS grade (as opposed to C or D) and to have developed any other type of complications than patients who were discharged home, but these differences were not statistically significant. Moreover, the groups were similar in terms of BMI at admission, surgical delay and ISS. All the results of the univariate analyses are more extensively presented in Table 1.
Of the six significant variables at the univariate level, three remained significant at the multivariate level. Results of the linear regression analysis are reported in Table 2. Living alone prior to the accident (ß = 0.15, 95% CI 0.02–0.28), presenting a neurological level of injury between C1 and C4 (ß = 0.16, 95% CI 0.02–0.29), and having a longer acute LOS (ß = 0.31, 95% CI 0.18–0.44) were all significantly associated with failure to discharge home. We also report an association – albeit not statistically significant—between having developed a pressure injury during acute care (ß = 0.12, 95% CI −0.02–0.25, P = 0.09) and not being discharged home after IFR.
Discussion
This work provides important insight on the factors associated with discharge destination and community reintegration following specialized inpatient rehabilitation in patients who sustained a TSCI. Out of the 193 patients studied, 11% (n = 22) failed to return home following IFR—a highly similar proportion to reported figures in the literature [5, 7]. More specifically, we report that having a high cervical injury (C1–C4), living alone prior to the accident, and having a longer acute LOS are all factors associated with a decreased likelihood of returning home.
Our findings regarding living arrangement are in line with previous literature and further confirm that enhanced social support could be instrumental in facilitating community living for TSCI patients living alone prior to the injury. As previously hypothesized by Anzai et al. [9], the explanation behind this result most probably resides in the fact that when available, close ones take on a role of day-to-day caregiver, allowing otherwise dependant patients to enjoy a higher autonomy from the resources provided by the health care system. When patients live alone, the likelihood that there are relatives to take on this responsibility decreases. It is also of notable importance to consider that individuals who live alone depend on a single-source household income and could suffer from severe financial difficulties (and only limited help for that issue) as a result of the accident. Literature has also demonstrated that as compared with unlicensed assistive personnel, family caregivers can also lower the prevalence of depression in patients after TSCI [16]. Accounting for the living arrangement of patients early during the acute phase could thus prove impactful in two ways. First of all, it is possible that by addressing patients’ social difficulties early during acute care with targeted and specialized resources in the form of social work, psychological support, and financial planning consultations, it could be easier to set realistic goals and plan early to adapt living arrangements to the functional limitations. Second of all, this early identification of at-risk patients could also create the opportunity for proper counseling and participation of family caregivers to facilitate return home.
Acute LOS was significantly longer in the group of patients who did not return home and we report a significant association between acute LOS and this undesired outcome. This finding suggests that taking action towards reducing acute LOS (thereby reaching our criteria for discharge from the acute care earlier) and accelerating exposure to IFR could potentially facilitate return home. This result is in line with previous research conducted in Canada on discharge destination in TSCI patients [5] and might be explained by the fact that shorter LOS in acute care and early transfer to IFR have been shown to be strong predictors of functional recovery after TSCI [17]. According to Gour-Provencal et al. [10], modifying treatment regimens in the early acute setting by increasing daily-therapy time in the form of physical therapy and occupational therapy could be one of two key elements to reduce acute LOS. On that matter, Gour-Provencal et al. [10] further suggest that much of this acute therapy should aim at providing adequate prerequisites for IFR and working on abilities such as balance training and endurance—which were listed as main criteria for determining readiness for discharge to IFR. Reducing acute LOS might also be achieved by finding ways to diminish the occurrence of secondary complications, such as pressure injuries, which have also been found to cause longer acute LOS [10, 17] and were correlated in this paper with discharge location.
On the matter of pressure injuries, despite the fact that our results cannot support a statistically significant association between the occurrence of pressure injuries during acute hospitalization and discharge destination following IFR, we still have to report a trend to that effect (ß = 0.12, 95% CI −0.02 to 0.25, P = 0.09). While the intricacies of the relationship between pressure injuries and rehabilitation outcomes have not been thoroughly examined, it is suggested that developing a pressure injury during the acute care could be detrimental to the rehabilitation process by hindering the course of therapy sessions in IFR. The implementation of aggressive preventative strategies to reduce the occurrence of pressure injuries during the acute care, such as frequent repositioning and early mobilization of patients might help potentiate the impact of rehabilitative care on discharge outcomes [10].
Finally, we report a significant association between presenting a neurological level of injury between C1 and C4 and being discharged somewhere other than home. This finding is in accordance with the figures reported by Anzai et al. [9] on discharge destination in high cervical TSCI patients, which revealed a much lower proportion of home discharges in this specific population compared to the figures reported in studies which included all neurological levels of injuries [5, 7, 8]. Since higher neurological levels of injuries have been repeatedly associated with poorer functional outcomes [17] this finding is probably explained by the fact that high cervical patients can be less apt to manage self-care and activities of daily living without the continuous assistance that is provided in nursing homes or long-term care facilities.
Surprisingly, the proportion of elderly patients (≥65 years of age) was not significantly higher in the group of patients who failed to return home. These results contrast deeply with some data reported in the literature. Age has indeed been identified as a strong predictor of discharge to a long-term care facility following SCI [5, 7, 9], especially for patients above 65 years of age [18]. Anzai et al. also described “older age” as a significant variable for discharge to a nursing home after IFR in high cervical SCI patients in British Columbia [9]. In view of this contrast with previous literature, additional analyses (not shown) were conducted with age as a continuous variable but no association between age and discharge destination further emerged. Two explanations for this discrepancy are possible. First, it is possible that the relatively small group size of patients not returning home (n = 22) was not sufficient to reach significance. More likely, the second possible explanation is the presence of a period effect since previous studies [7, 9, 18] were done on cohorts from a different time period; and that nowadays chronological age is not a predictor of returning home anymore, and should not be an important factor for determining final discharge destination.
The first limitation of our study is related to the relatively small number of patients who were not discharged home following IFR. This could explain the absence of statistical significance that we observed in our analyzes for the association between the occurrence of pressure injuries during acute hospitalization and discharge destination following IFR. Another possible limitation of our study is that due to the particular public healthcare system prevailing in Quebec, Canada, differences could exist with other countries (and provinces within Canada) with respect to the course of events during the acute and subacute phases after the injury. In some countries, patients’ acute LOS can be much shorter than what is reported herein. For example, in the United States, acute LOS have oscillated between 6.5 and 7.5 days on average since 1993 [19]. As a result, it is possible that our findings regarding this variable and its predictive value of discharge destination might not be easily reproducible in other settings. This discrepancy regarding acute LOS might also affect the comparativeness of our results in terms of the rates of acute complications we report and their association with the dependant variable. However, despite these differences, our findings remain applicable to all contexts because early consideration of all predictors identified in this study would still be important, whether the patient is still in an acute care institution or already in an IFR setting. For example, although we report longer mean acute LOS than what may be observed in the US, for example, our finding pointing towards better odds of home discharge in patients who present shorter acute LOS refers not to the duration of acute LOS per se, but rather to the delay between the time of injury and the moment at which the patient is medically, physically and mentally ready to undergo intensive rehabilitation therapy.
Finally, a last possible limitation of our study was that we only included complete cases in our analyzes, which did result in a drop of the number of patients available for analysis and could cast some doubt as to the generalizability of our findings. However, additional analyzes (not shown) demonstrated that patients that were not included because they presented incomplete datasets were not statistically different to our final cohort in terms of acute LOS, rehab LOS, age, sex, living arrangement, CCI, NLI, and AIS grade. Differences were observed solely for BMI and surgical delay. However, since neither of these variables emerged as significant predictors of discharge destination after IFR, it is highly unlikely that these differences would have altered our findings in any way.
In brief, this study identifies several variables associated with discharge destination following IFR in TSCI patients. Our findings point towards the conclusion that taking certain actions early in the acute phase could help maximize the likelihood of returning home. In particular, returning home would be more likely with early identification and planning for supporting patients who live alone, along with the implementation of timely measures for reaching transfer criteria for IFR as early as possible (e.g., specific therapy for improving balance and endurance during the acute care, early mobilization after surgery, etc.), and overall increased resources for high cervical patients. Prospective evaluations of paramedical interventions on discharge outcomes from IFR remain required. The validity of age as a variable of clinical importance for post-injury autonomy should also be re-examined and additional work remains needed to clarify the relationship between the occurrence of pressure injuries and discharge destination following specialized inpatient rehabilitation.
Data archiving
The datasets generated during and/or analyzed during the current study are not publicly available due to the regulations defined by the ethics committee of the CIUSS Nord-de-l’Île-de-Montréal but are available from the corresponding author on reasonable request.
References
DeVivo MJ, Richards JS. Community reintegration and quality of life following spinal cord injury. Paraplegia. 1992;30:108–12.
Putzke JD, Richards JS. Nursing home residence: quality of life among individuals with spinal cord injury. Am J Phys Med Rehabil. 2001;80:404–9.
Silver J, Ljungberg I, Libin A, Groah S. Barriers for individuals with spinal cord injury returning to the community: a preliminary classification. Disabil Health J. 2012;5:190–6.
Smith B, Caddick N. The impact of living in a care home on the health and wellbeing of spinal cord injured people. Int J Environ Res Public Health. 2015;12:4185–202.
Cheng CL, Plashkes T, Shen T, Fallah N, Humphreys S, O’Connell C, et al. Does specialized inpatient rehabilitation affect whether or not people with traumatic spinal cord injury return home? J Neurotrauma. 2017;34:2867–76.
Munce SE, Wodchis WP, Guilcher SJ, Couris CM, Verrier M, Fung K, et al. Direct costs of adult traumatic spinal cord injury in Ontario. Spinal Cord. 2013;51:64–9.
Whiteneck G, Gassaway J, Dijkers MP, Heinemann AW, Kreider SE. Relationship of patient characteristics and rehabilitation services to outcomes following spinal cord injury: the SCIRehab project. J Spinal Cord Med. 2012;35:484–502.
DeVivo MJ. Discharge disposition from model spinal cord injury care system rehabilitation programs. Arch Phys Med Rehabil. 1999;80:785–90.
Anzai K, Young J, McCallum J, Miller B, Jongbloed L. Factors influencing discharge location following high lesion spinal cord injury rehabilitation in British Columbia, Canada. Spinal Cord. 2006;44:11–8.
Gour-Provencal G, Mac-Thiong JM, Feldman DE, Begin J, Richard-Denis A. Decreasing pressure injuries and acute care length of stay in patients with acute traumatic spinal cord injury. J Spinal Cord Med. 2020 [Published online ahead of print].
Membres de la Table de réadaptation fonctionnelle intensive de Montréal et du sous-comité sur les soins postaigus de la Table SAPA de Montréal. Programme de soins postaigus et services de rédaptation fonctionnelle intensive pour la clientèle montréalaise. 2017. p. 40.
Baker SP, O’Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96.
Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173:676–82.
WHO. US National Institute of Aging. Global health and aging. 2011.
Kirshblum S, Waring W 3rd. Updates for the International Standards for Neurological Classification of Spinal Cord Injury. Phys Med Rehabil Clin N Am. 2014;25:505–17.
Kang MG, Kim CH, Park E, Huh JW, Yang WJ, Nam TW, et al. Effect of family caregiving on depression in the first 3 months after spinal cord injury. Ann Rehabil Med. 2018;42:130–6.
Richard-Denis A, Beausejour M, Thompson C, Nguyen BH, Mac-Thiong JM. Early predictors of global functional outcome after traumatic spinal cord injury: a systematic review. J Neurotrauma. 2018;35:1705–25.
Gulati A, Yeo CJ, Cooney AD, McLean AN, Fraser MH, Allan DB. Functional outcome and discharge destination in elderly patients with spinal cord injuries. Spinal Cord. 2011;49:215–8.
Jain NB, Ayers GD, Peterson EN, Harris MB, Morse L, O’Connor KC, et al. Traumatic spinal cord injury in the United States, 1993-2012. JAMA. 2015;313:2236–43.
Acknowledgements
We acknowledge the contribution of all team members at the Orthopedics—Spine Research Unit of the Hôpital du Sacré-Coeur de Montréal. We thank Louis-Félix Gravel (medical student at the University of Montreal) and Ms. Geneviève Leblanc who both assisted in the task of data extraction. We also recognize the important guidance of Dr. Jean Bégin, who provided us with crucial insight for the design of all statistical analyses. Finally, we thank the patients for their essential participation in all our research initiatives.
Funding
This research was funded by the Programme d’Excellence en Médecine pour l’Initiation En Recherche, the Fonds de recherche du Québec – Santé, the Praxis Spinal Cord Institute and the Medtronic Research Chair in Spinal Trauma at Université de Montréal.
Author information
Authors and Affiliations
Contributions
AD was responsible for designing the protocol, conducting the search, screening for potentially eligible patients, extracting and analyzing data, interpreting results, creating findings tables and figures, and writing the report. AR-D was responsible for designing the protocol and reviewing the manuscript. VL was responsible for extracting and analyzing data. J-MM-T was the senior author for this study. As such, he was responsible for designing the research protocol, interpreting the results, reviewing the manuscript and securing funding.
Corresponding author
Ethics declarations
Conflict of interest
AR-D has received a scholarship and research grants from the Fonds de recherche du Québec – Santé, an investigator-initiated research grant from Medline Industries, and a research grant from Praxis Spinal Cord Institute. J-MM-T is chairholder of the Medtronic research chair in spinal trauma at Université de Montréal, owns stocks and is a board member in Spinologics, and has received a scholarship and research grants from the Fonds de recherche du Québec – Santé, an investigator-initiated research grant from Medline Industries, educational grants from Medtronic and Depuy-Synthes, as well as research grants from the U.S. Department of Defense—Congressionally directed medical research programs, Craig H. Neilsen Foundation, from Social Sciences and Humanities Research Council, Canadian Institutes of Health Research, Natural Sciences and Engineering Research Council, Praxis Spinal Cord Institute, and Vertex Pharmaceutical. AD and VL have nothing to disclose.
Ethical approval
This study was approved by the “Comité d’éthique de la recherche du CIUSSS du Nord-de-l’Île-de-Montréal” at Hôpital Sacré-Cœur de Montréal. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dionne, A., Richard-Denis, A., Lim, V. et al. Factors associated with discharge destination following inpatient functional rehabilitation in patients with traumatic spinal cord injury. Spinal Cord 59, 642–648 (2021). https://doi.org/10.1038/s41393-020-00542-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-00542-z