Abstract
Rheumatoid arthritis (RA) is an aggressive autoimmune arthritis, and current therapies remain unsatisfactory due to low remission rate and substantially adverse effects. Low-dose interleukin-2 (Ld-IL2) is potentially a therapeutic approach to further improve the disease. This randomized, double-blind, placebo-controlled trial was undertaken to evaluate the efficacy and safety of Ld-IL2 in patients with active RA. Patients were randomly assigned (1:1) to receive Ld-IL2, defined as a dose of 1 million IU, or placebo in a 12-week trial with a 12-week follow-up. Three cycles of Ld-IL2 or placebo were administered subcutaneously every other day for 2 weeks (a total of 7 doses), followed by a 2-week break. All patients received a stable dose of methotrexate (MTX). The primary outcomes were the proportion of patients achieving the ACR20, DAS28-ESR <2.6, and the change from baseline in CDAI or SDAI at week 24. Secondary endpoints included other clinical responses and safety. The primary outcomes were achieved in the per-protocol population. The improvements from baseline in CDAI and SDAI were significantly greater across time points for the Ld-IL2 + MTX group (n = 17) than for the placebo+MTX group (n = 23) (P = 0.018 and P = 0.015, respectively). More patients achieved ACR20 response in the Ld-IL2 + MTX group than those in the placebo+MTX group at week 12 (70.6% vs 43.5%) and at week 24 (76.5% vs 56.5%) (P = 0.014). In addition, low Treg and high IL-21 were associated with good responses to Ld-IL2. Ld-IL-2 treatment was well-tolerated in this study. These results suggested that Ld-IL2 was effective and safe in RA. ClinicalTrials.gov number: NCT 02467504.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a prevalent autoimmune disease characterized by progressive articular destruction and is notoriously difficult to treat with poor remission.1,2 Basic studies have shown that impaired immunological homeostasis plays a critical role in the development of RA.3 The distribution of regulatory T cells (Tregs) contributes to the disease activity of RA;4 effector T cells (Teff) are involved in the pathogenesis of RA, particularly impacting joint erosion.5,6,7 Clinically, methotrexate (MTX) is the first-line anchor drug for RA, but it is efficacious in only 19.8–25.4% of RA patients.1 It was also shown that 30–50% of patients need additional treatment.8,9,10 The ceiling phenomenon of low efficacy of MTX in RA is at least partially related to its interrupting effect on Tregs.11 A novel strategy to overcome the dilemma phenomenon of MTX is expected clinically.
The cytokine interleukin-2 (IL-2) is essential for the biogenesis and function of Tregs. The deficiency of Tregs can be promoted by low-dose interleukin-2 (Ld-IL2).12,13 A study showed that defects of Tregs from patients with RA were reversed by exogenous IL-2 in vitro.14 On the other hand, Ld-IL2 can inhibit Th17 cell proliferation, which is associated with the development of RA.15 Ld-IL2 treatment may be beneficial in RA.
We evaluated the potential effects and safety of Ld-IL2 along with MTX on RA in a randomized, double-blind, placebo-controlled trial for the first time. Furthermore, we identified factors in predicting potential responses to the treatment of Ld-IL2.
Result
Study population
Of the 52 patients screened, 47 patients were randomly assigned to the Ld-IL2 + MTX group (n = 23) or the placebo+MTX (n = 24) (Supplementary Table 1). Flow diagram of participants at each stage of the trial was shown in Fig. 1. In total, 40 (85.1%) patients completed the 24-week trial. Through week 24, 7 patients discontinued the study; the reasons included withdrawal by patients (n = 5) and lost to follow-up (n = 2).
Baseline demographics and disease characteristics were comparable in the two groups (Table 1), with the following exception: compared with the placebo + MTX group, patients in the Ld-IL2 + MTX group have more swollen joint counts (4.5 versus 2.9).
Efficacy
The primary outcomes were achieved in a per-protocol (PP) analysis set. More patients achieved American College of Rheumatology (ACR)20 response in the Ld-IL2 + MTX group (n = 17) than those in the MTX + placebo group (n = 23) at week 12 (70.6% vs 43.5%, P = 0.081) and at week 24 (76.5% vs 56.5%, P = 0.080). There were significant treatment differences across time points (P = 0.014). At week 12, the rate of ACR50 response in the Ld-IL2 + MTX group was significantly higher than that in the MTX + placebo group (P = 0.026). Compared to the placebo + MTX group, a higher percentage of patients with Ld-IL2 + MTX achieved ACR50 response (58.8% vs 34.8%) and ACR70 response (23.5% vs 8.8%) at week 24 (Fig. 2a, Supplementary Table 2), even though there were no statistically significant differences. The improvements from baseline in Clinical Disease Activity Index (CDAI) and Simplified Disease Activity Index (SDAI) were significantly greater across time points for the Ld-IL2 + MTX group than for the placebo+MTX group (P = 0.018 and P = 0.015, respectively, Fig. 2b, c, Supplementary Table 2). The change from baseline in CDAI score at week 24 was −16.6 in the Ld-IL2 + MTX group, as compared with −12.5 in the placebo+MTX group (P = 0.047). The changes from baseline in SDAI score at week 24 were −17.5 and −13.0 in the two groups, respectively (P = 0.062). At week 24, disease activity score (28 joint) calculated using erythrocyte sedimentation rate formula (DAS28-ESR) < 2.6 was achieved by 35.3% (6/17) of the patients in the Ld-IL2 + MTX group and 26.1% (6/23) of patients in the placebo+MTX group. Even though there was a higher percentage of patients achieving DAS28 remission in the Ld-IL2 group, statistically significant improvement was not observed.
Clinical responses to Ld-IL2 combined with MTX therapy. The data were presented in a per-protocol (PP) analysis set. The proportion of patients achieving an ACR20/50/70 response by at week 12 and 24 (a). The mean changes from baseline for CDAI and SDAI (b, c). The mean changes from baseline for pain, PtGA and PhGA of disease activity (d). Data in graphs were mean ± SE. *P < 0.05, with analyses with a logistic regression model or a covariance (ANCOVA) model at week 12 or 24. #P-value, presenting treatment differences across time points with a mixed model for repeated-measures analysis or Generalized Estimation Equations (GEE) method. ACR20/50/70 the American College of Rheumatology for 20%/50%/70% improvement, CDAI Clinical Disease Activity Index, SDAI Simplified Disease Activity Index, Ld-IL2 low-dose interleukin-2, MTX methotrexate, PtGA patient’s global assessment, PhGA physician’s global assessment
Compared with the placebo group, benefits with Ld-IL2 were observed in pain assessment, physician’s and patient’s global assessment of disease activity at week 12 (P = 0.009, P = 0.033, and P = 0.006, respectively, Fig. 2d, Supplementary Table 2). No significant differences were found when comparing the decreases of tender joint count (TJC) and swollen joint count (SJC) between the two groups. Similar clinical improvements in acute phase reactants, Short Form-36 (SF-36) score, and health assessment questionnaire disability index (HAQ-DI) were shown for both Ld-IL2 and placebo groups. No significant decrease in rheumatoid factor (RF) and anti-cyclic citrullinated peptide (CCP) antibody was observed (Supplementary Table 2).
Intention-to-treat (ITT) analyses for clinical outcomes were also performed (Supplementary Table 3). Although some numerical trends towards improvement were observed in primary and secondary outcomes, the marginal changes were relatively small.
Safety
Ld-IL2 was well-tolerated during the trial. Through week 24, the proportion of patients with at least one adverse event (AE) in the Ld-IL2 group was 47.8% (11/23) and in the placebo group was 37.5% (9/24) (Table 2). No drug-related serious adverse events (SAEs) occurred in both groups. Transient fever was observed in the Ld-IL2 + MTX group (n = 2), and there were injection-site reactions (3 in Ld-IL2 + MTX and 2 in placebo + MTX groups, respectively). No intervention was needed to resolve these events.
The incidence of patients with SAEs through week 24 was low and similar between the two groups. There were two SAEs reported in the Ld-IL2 group, including surgery for osteochondroma not related to the study and worsening of RA. The patient with worsening of RA had severe disease activity (DAS28-ESR 6.6) at baseline and was admitted to the hospital 4 weeks after the participation in the study. One patient with SAE in the placebo group was admitted to the hospital because of hypertension. All SAEs were singular events, and no specific association between SAEs and treatment was identified.
Factors predicting potential response to Ld-IL2
To identify factors predicting potential response to Ld-IL2 in RA, we separated Ld-IL2 + MTX group (n = 23) into responders (n = 11) and non-responders (n = 10), according to the decrease of DAS28-ESR more than 1.2. Two patients who discontinued prior to receiving 1 cycle of Ld-IL2 were not involved. Improved response to the Ld-IL2 therapy was clearly correlated with a lower frequency of baseline Tregs and higher serum levels of IL-21 (P = 0.036 and P = 0.012, respectively, Fig. 3a, b, Supplementary Table 4). The percentage of Tregs was associated with the level of IL-2 (Fig. 3c). The detailed differences between the two groups were shown in Fig. 3d, e.
Predictive biomarkers for potential response to Ld-IL2 treatment in RA. The percentage of regulatory T cells (Tregs) in CD4+ T cells and serum level of IL-21 in responders and non-responders (a, b). The correlation between percentage of Tregs and serum level of IL-2 (c). Heatmap showed a classification of the two groups (d). Each column represented an individual. Colors in the horizontal bar denoted the non-responder group (red) and the responder group (green). Tiles were colored based on clinical features, Tregs and serum cytokine levels, red and blue indicating high and low levels, respectively. Primary composition analysis (e). The non-responder group was shown in red, and the responder group was shown in green. PC1 and PC2 account for 39.8% and 14%, respectively, of the total variance. Panels d and e were performed by R 4.1.0 and R-packages (mixOmics and pheatmap) (http://www.metaboanalyst.ca). Data in graphs were mean ± SE. *P < 0.05
Immunological analysis
We evaluated the changes of Treg cells in patients during the trial. Consistent with clinical improvement, the proportion of Treg cells in CD4+ T cells were significantly increased in association with the Ld-IL2 administration, at week 2, 6, and 10 (P = 0.001, 0.019, and 0.001, respectively, Fig. 4a). It was shown that MTX caused a significant decrease in Tregs (P = 0.029), while the addition of Ld-IL2 reversely expanded Tregs (P = 0.034) (Fig. 4b). The proportion of Th17 cells decreased significantly with MTX therapy (P = 0.001, Fig. 4c). There was a decline of Th17 cells in the Ld-IL2 + MTX arm, but it was not statistically significant (P = 0.078, Fig. 4c). The ratio of Treg/Th17 increased signifsignificantly with Ld-IL2 + MTX (P = 0.016), while it decreased with placebo+MTX (P < 0.001) (Fig. 4d). These data were consistent with the notion that Ld-IL2 counteracted the impairment of Tregs caused by MTX.
Ld-IL2 therapy synergized with MTX to expand the population of Tregs and ameliorate inflammation of RA. The proportion of Tregs in CD4+ T cells. Grey areas indicated the periods on Ld-IL2 or placebo therapy (a). The changes of the proportion of Tregs or Th17 in Ld-IL2 combined with MTX group and MTX alone group (b, c). The ratio of Tregs/Th17 (d). The serum levels of IL-17A, IFN-γ, TNF-α, and IL-12 were decreased significantly at week 12 (e). Data in bar graphs were mean ± SE. Ld-IL2 low-dose interleukin-2, MTX methotrexate, Treg regulatory T cell. *P < 0.05
Notably, we also found that the therapy comprising Ld-IL2 and MTX caused significant reductions of inflammatory cytokines, including IL-17A, IFN-γ, TNF-α, and IL-12 levels, at week 12 (P = 0.004, 0.028, 0.020, and 0.015, respectively, Fig. 4e, Supplementary Table 5).
Discussion
This randomized, double-blind, placebo-controlled clinical study provided the first evidence that Ld-IL2 further increased the efficacy of MTX. The treatment was well-tolerated, and was accompanied by a significant clinical improvement of CDAI, SDAI, and ACR response.
Tregs could be an ideal target for therapies to induce remission of autoimmune disorders.16 IL-2 has been reported to exert beneficial effects for the treatment.12,17,18,19 Recently, Klatzmann et al. reported the safety, biological and clinical effects of Ld-IL2 in a basket of 11 individual diseases, including RA.20 In the present study, we conducted a randomized, double-blind, placebo-controlled study. The results demonstrated that Ld-IL2 in combination with MTX outperformed the placebo+MTX for clinical outcomes including CDAI, SDAI, and ACR response.
The improvements of patient’s assessment of pain, patient’s global assessment (PtGA), and physician’s global assessment (PhGA) of disease activity were observed in the Ld-IL2 group, without significant reductions in TJC and SJC compared to the placebo group. TJC and SJC were important because articular involvement was the main feature of RA. However, systemic clinical manifestations, like fatigue and morning stiffness, were not involved. SDAI and CDAI incorporate the systemic features and are able to express the response of the study drug objectively. Our study demonstrated that Ld-IL2 treatment achieved a significant clinical improvement in response to SDAI, CDAI, and ACR response.
In agreement with improvements in clinical features, inflammatory cytokines were dampened with Ld-IL2 treatment. The dose and schedule of IL-2 administration varied in different studies and further clinical trials would be required to decipher the dose-response relationship.21 We defined three cycles of Ld-IL2 administration subcutaneously every other day for 2 weeks (a dose of 1 million IU, a total of 7 doses), followed by a 2-week break. We found an increase in the number of Tregs at the end of the treatment cycle, followed by a decrease until the next cycle. This treatment regimen was effective and tolerate in systemic lupus erythematosus (SLE).22
Given that the proportion of Tregs was known to be reduced in the peripheral blood of RA patients,23 promoting the Treg population could facilitate the development of novel immunotherapies for treating RA. The results of this study supported that MTX actually caused a significant decrease in Tregs, while administration of Ld-IL2 with MTX increased the percentage of Tregs. Data of in vitro assays supported that MTX decreased the proportion of Tregs, while administration of IL-2 with MTX increased Tregs. Furthermore, the level of Foxp3 and IL-10 mRNA expression decreased with MTX, and increased with IL-2, consistently with the change of Treg cell population (Supplementary Fig. 1). We assumed that the Treg-disrupting effect by MTX was at least partially the explanation for MTX resistance and the poor responding in patients with RA. There were inconsistent results of MTX effect on Tregs population and function.24,25,26 Many factors, such as background therapy, duration of MTX treatment, disease activity, and disease duration varied in previous studies, which could influence the results of MTX effect on the Treg frequency and function. As we know, one of the mechanisms of MTX efficacy is folate antagonism. Previous studies demonstrated that the Treg population was suppressed due to folate deficiency.11,27 We suggest that MTX impairs the Treg population by inhibiting the folate pathway. Further studies to define the mechanism of MTX to target Tregs are needed.
In addition, both MTX alone and Ld-IL2 + MTX treatment attenuated the percentage of Th17 cells. However, the ratio of Treg/Th17 significantly increased after the combination of Ld-IL2 and MTX treatment. The therapeutic effectiveness of MTX could be related to the decrease in circulating Th17 cell frequencies, while Ld-IL2 could counteract rebalance the immune homeostasis, suggesting a potential therapeutic strategy.
As a pleiotropic cytokine, high-dose IL-2, produced primarily by CD4 + T cells, can promote autoimmune responses, while low-dose IL-2 restores immune tolerance. Our study showed a decline in serum IL-2 level after Ld-IL2 treatment (Supplementary Table 5). This result suggested that Ld-IL2 might downregulate endogenous IL-2 and drive immune tolerance without increasing serum IL-2. A decrease in IL-2 concentration might result from the efficacy of the treatment, which needs to be further studied in a larger trial.
We observed that although Ld-IL2 synergized with MTX in improving the clinical and immunological outcomes of RA, in some patients Ld-IL2 failed to achieve adequate suppression of disease activity. We determined Ld-IL2 response in patients who had completed at least 1 cycle of Ld-IL2. In order to address this apparently differential response to the treatment, our results indicated that response to Ld-IL2 was probably correlated with a lower proportion of Treg cells and higher serum IL-21 levels. IL-21 plays a critical role in the activation and proliferation of Th17 cells and follicular helper T (Tfh) cells and further mediates several inflammatory processes in RA pathogenesis and progression.28 IL-21 could inhibit IL-2 production and impair Treg homeostasis,29 while IL-2 could improve these effects. Thus, optimizing the stratification will help to understand the conditions in which patients can benefit from Ld-IL2 therapy.
Current treatment regimens mainly rely on conventional synthetic disease-modifying anti-rheumatic drugs (csDMARDs) and biologic agents, which are associated with substantial adverse effects including liver damage, cytopenia, nausea, and various infections.1,30 MTX is the most widely accepted initial therapy, but it is not efficacious in a large proportion of patients. The potential adverse effects limit the use of MTX. In this study, gastrointestinal disorders and hepatic enzyme increase were associated with the side effects of MTX. A drug-related side effect was barely observed in Ld-IL2, which was consisted with previous studies.12,22 Particularly, Ld-IL2 could be beneficial for leukopenia and infection. In SLE study, we observed the significant increase of natural killer (NK) cells in response to Ld-IL2 treatment, which implicated potential augmentation of anti-infection cellular immunity.22 We also found that CD56bri NK cells were increased in association with Ld-IL2 administration (Supplementary Fig. 2). Injection-site reactions and transient fever were the most common AE, while no event was severe or resulted in the discontinuation of the study agent. Vascular leak syndrome, one of the main complications of high-dose IL-2 administration, did not occur. Overall, no safety risk or a particular pattern of association between AEs and Ld-IL2 treatment was observed.
Six patients in the Ld-IL2 + MTX group and 1 patient in the placebo+MTX group discontinued the trial prematurely. The withdrawal might result from the protocol-mandated requirement for frequent visits. None of the patients reported premature discontinuation associated with the study drug.
Our study has some limitations. Enrollment was not stratified due to the small sample size in the study. In addition, the bias was possible because of the higher withdrawal rate in Ld-IL2 + MTX group. The background DMARD therapy varied among patients and was not further analyzed because of the inefficient number of patients. In a further study, optimizing the stratification would help to understand the clinical conditions that are likely to benefit from the Ld-IL2 therapy.
Taken together, this study provides the first clinical evidence that Ld-IL2 combined with MTX results in improvements in clinical and immunological responses of RA. The results demonstrate that Ld-IL2 is a novel and practical therapeutic approach in RA.
Methods
Study design
This study was a 6-month, pilot, randomized, double-blind, placebo-controlled trial to verify the clinical response and safety of Ld-IL2 for the treatment of moderate to severely active RA (ClinicalTrials.gov number, NCT02467504). This study was performed in accordance with the Declaration of Helsinki and Good Clinical Practice principles, and was approved by Peking University People’s Hospital Ethics Committee. All patients provided written informed consent. This study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline.31
Participants
Methotrexate (MTX)-naïve patients with moderate to severely active RA were recruited from Department of Rheumatology and Immunology of Peking University People’s Hospital from July 2015 to August 2017. All patients (18–70 years) with RA fulfilled the revised 1987 ACR criteria,32 and were eligible if they had moderate to severely active disease, defined as DAS28-ESR > 3.2.33 Patients could continue treatments with oral non-steroidal anti-inflammatory drugs or oral corticosteroids (≤10 mg/day) and/or csDMARDs except MTX, provided that the doses had been stable for at least 3 months before baseline and remained stable throughout the trial. Patients previously given biologic DMARDs or MTX were excluded from the study. Patients were also excluded if they had an autoimmune disease other than RA, an active infection, recurrent bacterial infections, severe hepatic and renal dysfunction, or malignant tumor (Supplementary Table 6). Patients could withdraw from the study at any time for any reason.
Randomization
Patients who underwent screening procedures and met the inclusion criteria were enrolled in the study. Stratified randomization was performed using computer-generated block randomization (block size of 4), by an independent third party (Beijing Stemexcel Technology Co. Ltd, China). Patients were randomly assigned (1:1) to Ld-IL2 + MTX or placebo+MTX. Patients, investigators, study coordinators, and monitors were masked to treatment assignment during subcutaneous administration of the drug and assessment of the patients during the 24-week trial.
Interventions
Ld-IL2 (recombinant human IL-2Ser125) and placebo were sponsored by Beijing SL PHARM. None of the sponsors were involved in the design and conduction of this study, or the preparation of this manuscript. The data of this study would be unavailable to the sponsors until the study was published.
Ld-IL2 was administered as a dose of 1 million IU. Three cycles of Ld-IL2 or placebo were administered subcutaneously every other day for 2 weeks (a total of 7 doses), followed by a 2-week break. The dosing schedule was used in earlier studies22,34. MTX was initiated at 7.5 mg per week, and was increased to a maximum of 15 mg per week by week 4. MTX 7.5–15 mg per week was permitted for patients intolerant to higher doses. Patients received folic acid supplements of 10 mg per week. The study design was shown in Supplementary Fig. 3. Patients were assessed at a 2-week interval during the first 12 weeks and at a 4-week interval thereafter until week 24. Physical examination included SJC and TJC with 28 joints. The patient’s assessment of pain, PtGA, and PhGA of disease activity were evaluated using visual analog scales (VAS) of 0–10 cm. Physical function was assessed by HAQ-DI. Health-related quality of life, assessed at baseline and week 24, was evaluated using the SF-36, which assessed eight domains scored from 0 to 100 that could be aggregated into physical and mental component sores (PCS and MCS).35 Laboratory monitoring included measurement of inflammatory markers, blood counts, and routine biochemistry.
Outcome measures
The primary outcomes were the proportion of patients achieving ACR20 response and DAS28 remission, the change from baseline in the CDAI and SDAI at week 24. Secondary outcomes included improvement of physical examination, the change of disease activity assessment using VAS, the change from baseline of DAS28-ESR, the change of physical function assessment by HAQ-DI score, and the improvement of quality of life using the SF-36.
ACR20/50/70 assessments were based on a 20%/50%/70% or greater improvement from baseline in the number of tender joints, a 20%/50%/70%, or more improvement in the number of swollen joints, and a 20%/50%/70% or greater improvement in 3 of the 5 remaining core set measures: patient’s assessment of pain, PtGA, PhGA, HAQ-DI, and CRP.
Flow cytometry and ELISA assays
Peripheral blood mononuclear cells (PBMCs) were resuspended in Cell Staining Buffer at 5–10 × 106 cells/ml and distributed 100 µl/tube of cell suspension (5–10 × 105 cells/tube) into 12 × 75 mm plastic tubes. Cells were pre-incubated with 5 µl of Human TruStain FcX™ (BioLegend) per 100 µl of cell suspension for 5–10 min at room temperature. After washing one time, fluorescence conjugated antibodies were added at predetermined optimum concentrations and incubated on ice for 20 min in the dark. Cells were then washed two times with at least 2 ml of Cell Staining Buffer by centrifugation at 400 × g for 5 min. Cell pellets were resuspended in 0.5 ml of Cell Staining Buffer and 5 µl (0.25 µg)/million cells of 7-AAD solution was added to exclude dead cells. Incubate on ice for 3–5 min in the dark. Proportions of T cell subsets were analyzed by flow cytometry using a FACSAria II (BD) instrument and FlowJo software (TreeStar). The fluorescence conjugated antibodies for flow cytometry were listed in Supplementary Table 7. Tregs were defined as CD3+CD4+CD25highCD127low and Th17 cells were defined as CD3+CD4+CD45RA-CXCR3-CCR6+ (Supplementary Fig. 4).36,37 Inflammation associated cytokines or other soluble factors in patient serum, including IL-2, IL-6, IL-17A, IL-21 TNF-α, IFN-γ, sCD25, IL-4, IL-12, TGF-β, and CXCL13, were determined by ELISA kits (MultiSciences, Hangzhou, China), following instructions from the manufacturer.
Adverse events
Safety was evaluated by the frequency and severity of AEs through 24 weeks. Patients were monitored at each visit for vital signs, clinical and laboratory abnormalities, AEs, and SAEs.
Statistical analysis
The sample size and power of the study were calculated based on the proportion of patients achieving ACR20 response in either group. Assuming that the proportion of patients receiving placebo + MTX group at week 24 would be 40% and the proportion of patients in Ld-IL2 + MTX group would be 75%, 22 patients were required for each group to have 70% or higher power to detect the difference between the two groups, with a significance level of 0.05.
Analysis of efficacy was performed on PP and ITT populations. The PP population was defined as the patients who completed the entire 24-week trial. The ITT population consisted of patients who were randomized and took at least one dose of treatment. If a patient had data for at least one ACR component at week 24, missing component data were imputed with the last observation carried forward if baseline data were available; otherwise, missing components were considered to worse than ACR20 response. The safety population included all patients who received at least one Ld-IL2 or placebo infusion.
Statistical analyses for baseline demographic and disease characteristics were done using student t-tests, Mann-Whitney U for comparisons of continuous variables, and Chi-square test for comparison of categorical variables. Binary efficacy variables were analyzed with a logistic regression model, adjusting age, gender, and baseline DAS28-ESR score. Continuous variables were assessed with an analysis of covariance (ANCOVA) model, including treatment group and baseline score. For continuous variables, treatment differences across time points were evaluated using a mixed model for repeated-measures analysis, with a visit, treatment group, treatment-by-visit interactions included in the model. The generalized Estimation Equations (GEE) method in a logistic repeated-measures model was used for categorical variables, controlling for confounder variables. Principal component analysis (PCA) and cluster analysis were used to analyze the variance between response and non-response groups to Ld-IL2 + MTX treatment. Cluster analysis by heatmap and PCA was performed by R 4.1.0 and R-packages (mixOmics and pheatmap) (http://www.metaboanalyst.ca).
A nominal significance level of 0.05 (two-sided) was applied to all the analyses. All statistical analyses were carried out by SPSS (version 23, IBM) and Graph Pad Prism (Version 5.0, Graph Pad Software).
Data availability
The data supporting the findings in this study will be available from the corresponding author on request.
References
Smolen, J. S. et al. Rheumatoid arthritis. Nat. Rev. Dis. Prim. 4, 18001–18023 (2018).
Zhu, H. et al. Remission assessment of rheumatoid arthritis in daily practice in China: a cross-sectional observational study. Clin. Rheumatol. 37, 597–605 (2018).
McInnes, I. B. & Schett, G. Pathogenetic insights from the treatment of rheumatoid arthritis. Lancet 389, 2328–2337 (2017).
Kawashiri, S. Y. et al. CD4+CD25(high)CD127(low/-) Treg cell frequency from peripheral blood correlates with disease activity in patients with rheumatoid arthritis. J. Rheumatol. 38, 2517–2521 (2011).
Chemin, K., Gerstner, C. & Malmstrom, V. Effector functions of CD4+ T cells at the site of local autoimmune inflammation-lessons from rheumatoid arthritis. Front. Immunol. 10, 353–368 (2019).
Kim, K. W., Kim, H. R., Kim, B. M., Cho, M. L. & Lee, S. H. Th17 cytokines regulate osteoclastogenesis in rheumatoid arthritis. Am. J. Pathol. 185, 3011–3024 (2015).
Sato, K. et al. Th17 functions as an osteoclastogenic helper T cell subset that links T cell activation and bone destruction. J. Exp. Med. 203, 2673–2682 (2006).
van der Heijde, D. et al. Comparison of etanercept and methotrexate, alone and combined, in the treatment of rheumatoid arthritis: two-year clinical and radiographic results from the TEMPO study, a double-blind, randomized trial. Arthritis Rheum. 54, 1063–1074 (2006).
de Jong, P. H. et al. Induction therapy with a combination of DMARDs is better than methotrexate monotherapy: first results of the tREACH trial. Ann. Rheum. Dis. 72, 72–78 (2013).
Bakker, M. F. et al. Low-dose prednisone inclusion in a methotrexate-based, tight control strategy for early rheumatoid arthritis: a randomized trial. Ann. Intern. Med. 156, 329–339 (2012).
Kinoshita, M. et al. Dietary folic acid promotes survival of Foxp3+ regulatory T cells in the colon. J. Immunol. 189, 2869–2878 (2012).
He, J. et al. Low-dose interleukin-2 treatment selectively modulates CD4(+) T cell subsets in patients with systemic lupus erythematosus. Nat. Med. 22, 991–993 (2016).
Knoechel, B., Lohr, J., Kahn, E., Bluestone, J. A. & Abbas, A. K. Sequential development of interleukin 2-dependent effector and regulatory T cells in response to endogenous systemic antigen. J. Exp. Med. 202, 1375–1386 (2005).
Kosmaczewska, A. et al. Exogenous IL-2 controls the balance in Th1, Th17, and Treg cell distribution in patients with progressive rheumatoid arthritis treated with TNF-alpha inhibitors. Inflammation 38, 765–774 (2015).
Spolski, R., Li, P. & Leonard, W. J. Biology and regulation of IL-2: from molecular mechanisms to human therapy. Nat. Rev. Immunol. 18, 648–659 (2018).
Esensten, J. H., Wofsy, D. & Bluestone, J. A. Regulatory T cells as therapeutic targets in rheumatoid arthritis. Nat. Rev. Rheumatol. 5, 560–565 (2009).
Koreth, J. et al. Interleukin-2 and regulatory T cells in graft-versus-host disease. N. Engl. J. Med. 365, 2055–2066 (2011).
Lim, J. A. et al. New feasible treatment for refractory autoimmune encephalitis: Low-dose interleukin-2. J. Neuroimmunol. 299, 107–111 (2016).
Hartemann, A. et al. Low-dose interleukin 2 in patients with type 1 diabetes: a phase 1/2 randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 1, 295–305 (2013).
Rosenzwajg, M. et al. Immunological and clinical effects of low-dose interleukin-2 across 11 autoimmune diseases in a single, open clinical trial. Ann. Rheum. Dis. 78, 209–217 (2019).
Klatzmann, D. & Abbas, A. K. The promise of low-dose interleukin-2 therapy for autoimmune and inflammatory diseases. Nat. Rev. Immunol. 15, 283–294 (2015).
He, J. et al. Efficacy and safety of low-dose IL-2 in the treatment of systemic lupus erythematosus: a randomised, double-blind, placebo-controlled trial. Ann. Rheum. Dis. 79, 141–149 (2020).
Morita, T. et al. The proportion of regulatory T cells in patients with rheumatoid arthritis: a meta-analysis. PLoS ONE 11, e0162306–e0162323 (2016).
Guggino, G. et al. The in vitro addition of methotrexate and/or methylprednisolone determines peripheral reduction in Th17 and expansion of conventional Treg and of IL-10 producing Th17 lymphocytes in patients with early rheumatoid arthritis. Rheumatol. Int. 35, 171–175 (2015).
Bulatovic Calasan, M. et al. Methotrexate treatment affects effector but not regulatory T cells in juvenile idiopathic arthritis. Rheumatology 54, 1724–1734 (2015).
Porter, S. B. et al. Suppressor function of umbilical cord blood-derived CD4+CD25+ T-regulatory cells exposed to graft-versus-host disease drugs. Transplantation 82, 23–29 (2006).
Wu, C. H., Huang, T. C. & Lin, B. F. Folate deficiency affects dendritic cell function and subsequent T helper cell differentiation. J. Nutr. Biochem. 41, 65–72 (2017).
Spolski, R. & Leonard, W. J. Interleukin-21: a double-edged sword with therapeutic potential. Nat. Rev. Drug Discov. 13, 379–395 (2014).
Attridge, K. et al. IL-21 inhibits T cell IL-2 production and impairs Treg homeostasis. Blood 119, 4656–4664 (2012).
Li, R. et al. High remission and low relapse with prolonged intensive DMARD therapy in rheumatoid arthritis (PRINT): a multicenter randomized clinical trial. Medicine 95, e3968–e3975 (2016).
Schulz, K. F., Altman, D. G., Moher, D. & Group, C. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med. 7, e1000251 (2010).
Arnett, F. C. et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 31, 315–324 (1988).
Wells, G. et al. Validation of the 28-joint Disease Activity Score (DAS28) and European League Against Rheumatism response criteria based on C-reactive protein against disease progression in patients with rheumatoid arthritis, and comparison with the DAS28 based on erythrocyte sedimentation rate. Ann. Rheum. Dis. 68, 954–960 (2009).
He, J. et al. Circulating precursor CCR7(lo)PD-1(hi) CXCR5(+) CD4(+) T cells indicate Tfh cell activity and promote antibody responses upon antigen reexposure. Immunity 39, 770–781 (2013).
Ware, J. E. Jr & Sherbourne, C. D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 30, 473–483 (1992).
Todd, J. A. et al. Regulatory T cell responses in participants with type 1 diabetes after a single dose of interleukin-2: a non-randomised, open label, adaptive dose-finding trial. PLoS Med. 13, e1002139 (2016).
Hu, D. et al. Aberrant expression of USF2 in refractory rheumatoid arthritis and its regulation of proinflammatory cytokines in Th17 cells. Proc. Natl Acad. Sci. USA 117, 30639–30648 (2020).
Acknowledgements
We thank all the participants in this study. National Natural Science Foundation of China (U1903210, 31530020, 81701598, 31570880, 81471601, 81801617), Beijing Sci-Tech Program (Z171100000417007, Z191100006619114), and Macao Science and Technology Fund (0094/2018/A3).
Author information
Authors and Affiliations
Contributions
X.Z., J.H., and Z.L. contributed to the design of the study and analysis and interpretation of the data. X.Z., X.S., J.C., and H.L. contributed to the analysis and interpretation of the data. X.L., T.L., X.Z., J.H., M.S., X.Z., and Y.J. contribute to the conduct of the study and recruitment of patients. Y.Z., Y.Y., R.L., H.Y., Y.L., C.L., Y.L., L.R., and Y.S. contributed to data collection and recruitment of patients. M.S., M.M., Y.L., and R.Z. contributed to experiments. X.Z. and J.H. wrote the initial manuscript draft, and Z.L. critically revised the manuscript. All authors contributed to drafting the manuscript or revising it critically for important intellectual content, provided final approval of the final manuscript, and agreed to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
We have no conflicts of interest. The sponsor was not involved with the collection, management, analysis, interpretation of the data, or preparation of the manuscript. The corresponding authors had full access to all the data in the study and had the final responsibility for the decision to submit the paper.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, X., Miao, M., Zhang, R. et al. Efficacy and safety of low-dose interleukin-2 in combination with methotrexate in patients with active rheumatoid arthritis: a randomized, double-blind, placebo-controlled phase 2 trial. Sig Transduct Target Ther 7, 67 (2022). https://doi.org/10.1038/s41392-022-00887-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41392-022-00887-2
This article is cited by
-
The effects of low-dose IL-2 on Th17/Treg cell imbalance in primary biliary cholangitis mouse models
BMC Gastroenterology (2024)
-
Molecular Engineering of Interleukin-2 for Enhanced Therapeutic Activity in Autoimmune Diseases
BioDrugs (2024)
-
Inflammation across tissues: can shared cell biology help design smarter trials?
Nature Reviews Rheumatology (2023)
-
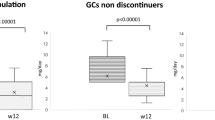
Low-dose IL-2 mitigates glucocorticoid-induced Treg impairment and promotes improvement of SLE
Signal Transduction and Targeted Therapy (2023)
-
Low-dose Interleukin-2 For Psoriasis Therapy Based on the Regulation of Th17/Treg Cell Balance in Peripheral Blood
Inflammation (2023)