Abstract
Background
Darolutamide is an androgen receptor pathway inhibitor (ARPI) used in patients with prostate cancer (PC). In pivotal trials, it has demonstrated a favorable toxicity profile. There are no head-to-head comparison studies between the different ARPIs, but the efficacy of these drugs seems to be similar making the toxicity profile a key element for treatment selection.
Methods
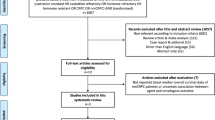
We conducted a systematic review of all clinical trials assessing treatment with darolutamide for patients with PC using placebo as the control using the PubMed/Medline and Cochrane library databases. We also performed a meta-analysis to compare the safety of darolutamide versus placebo evaluating adverse events (AE) leading to treatment discontinuation and the rate of the AE reported as “AE of interest” in the ARAMIS trial. The comparison among darolutamide and the placebo group in terms of safety and tolerability was performed using odds ratio (OR) as meta-analytic outcome.
Results
We identified three articles comprising 2902 patients for the systematic review and meta-analysis (1652 treated with darolutamide and 1250 with placebo). Darolutamide did not increase AE leading to treatment discontinuation compared to placebo (pooled OR: 1.176, 95% CI 0.918–1.507, p = 0.633). Regarding the “AE of interest” there was no difference between darolutamide and placebo in terms of asthenia, cardiac arrhythmia, cardiac disorder, coronary artery disorder, depression mood disorder, falls, fatigue, heart failure, hot flushes, hypertension, mental-impairment disorder, rash, seizure and weight loss. The only “AE of interest” with a statistically significant difference in favor of placebo was bone fractures (pooled OR: 1.523, 95% CI 1.081–2.146).
Conclusions
In our systematic review and meta-analysis, darolutamide showed a toxicity profile comparable to placebo with the exception of bone fractures. In the absence of head-to-head comparison studies between the different ARPIs, the results of our research suggest a preferred use of darolutamide in the approved settings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Baumgart SJ, Nevedomskaya E, Lesche R, Newman R, Mumberg D, Haendler B. Darolutamide antagonizes androgen signaling by blocking enhancer and super-enhancer activation. Mol Oncol. 2020;14:2022–39.
Fizazi K, Massard C, Bono P, Jones R, Kataja V, James N, et al. Activity and safety of ODM-201 in patients with progressive metastatic castration-resistant prostate cancer (ARADES): an open-label phase 1 dose-escalation and randomised phase 2 dose expansion trial. Lancet Oncol. 2014;15:975–85.
Massard C, Penttinen HM, Vjaters E, Bono P, Lietuvietis V, Tammela TL, et al. Pharmacokinetics, antitumor activity, and safety of ODM-201 in patients with chemotherapy-naive metastatic castration-resistant prostate cancer: an open-label phase 1 study. Eur Urol. 2016;69:834–40.
Fizazi K, Shore N, Tammela TL, Ulys A, Vjaters E, Polyakov S, et al. Nonmetastatic, castration-resistant prostate cancer and survival with darolutamide. N Engl J Med. 2020;383:1040–9.
Smith MR, Hussain M, Saad F, Fizazi K, Sternberg CN, Crawford ED, et al. Darolutamide and survival in metastatic, hormone-sensitive prostate cancer. N Engl J Med. 2022;386:1132–42.
Gillessen S, Procopio G, Hayoz S, Kremer E, Schwitter M, Caffo O, et al. Darolutamide maintenance in patients with metastatic castration-resistant prostate cancer with nonprogressive disease after taxane treatment (SAKK 08/16). J Clin Oncol. 2023;41:3608–15.
Mori K, Mostafaei H, Pradere B, Motlagh RS, Quhal F, Laukhtina E, et al. Apalutamide, enzalutamide, and darolutamide for non-metastatic castration-resistant prostate cancer: a systematic review and network meta-analysis. Int J Clin Oncol. 2020;25:1892–1900.
Wenzel M, Nocera L, Colla Ruvolo C, Wurnschimmel C, Tian Z, Shariat SF, et al. Overall survival and adverse events after treatment with darolutamide vs. apalutamide vs. enzalutamide for high-risk non-metastatic castration-resistant prostate cancer: a systematic review and network meta-analysis. Prostate Cancer Prostatic Dis. 2022;25:139–48.
Halabi S, Jiang S, Terasawa E, Garcia-Horton V, Ayyagari R, Waldeck AR, et al. Indirect comparison of darolutamide versus apalutamide and enzalutamide for nonmetastatic castration-resistant prostate cancer. J Urol. 2021;206:298–307.
Wang L, Paller C, Hong H, Rosman L, De Felice A, Brawley O, et al. Comparison of treatments for nonmetastatic castration-resistant prostate cancer: matching-adjusted indirect comparison and network meta-analysis. J Natl Cancer Inst. 2022;114:191–202.
Yanagisawa T, Rajwa P, Thibault C, Gandaglia G, Mori K, Kawada T, et al. Androgen receptor signaling inhibitors in addition to docetaxel with androgen deprivation therapy for metastatic hormone-sensitive prostate cancer: a systematic review and meta-analysis. Eur Urol. 2022;82:584–98.
Altavilla A, Di Maio M, Tucci M, Lolli C, Schepisi G, Buttigliero C, et al. Safety of new androgen receptor inhibitors (ARi) in patients with nonmetastatic castration-resistant prostate cancer (nmCRPC): a network meta-analysis of randomized controlled trials (RCT). Ann Oncol. 2019;30:v325–v355.
Colomba E, Jonas SF, Eymard JC, Delva R, Brachet PE, Neuzillet Y, et al. A randomized, open-label, cross-over phase 2 trial of darolutamide and enzalutamide in men with asymptomatic or mildly symptomatic metastatic castrate-resistant prostate cancer: patient preference and cognitive function in ODENZA. Eur Urol. 2023.
Borgmann H, Lallous N, Ozistanbullu D, Beraldi E, Paul N, Dalal K, et al. Moving towards precision urologic oncology: targeting enzalutamide-resistant prostate cancer and mutated forms of the androgen receptor using the novel inhibitor darolutamide (ODM-201). Eur Urol. 2018;73:4–8.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Langston B, Armes J, Levy A, Tidey E, Ream E. The prevalence and severity of fatigue in men with prostate cancer: a systematic review of the literature. Support Care Cancer. 2013;21:1761–71.
Ryan C, Wefel JS, Morgans AK. A review of prostate cancer treatment impact on the CNS and cognitive function. Prostate Cancer Prostatic Dis. 2020;23:207–19.
Wang X, Hui Y, Wang S, Hu X, Yu X, Wang W, et al. Comparison of effectiveness and safety outcomes of abiraterone versus enzalutamide in patients with metastatic castration-resistant prostate cancer: a systematic review and meta-analysis. J Pharm Pharm Sci. 2020;23:451–61.
Nowakowska MK, Ortega RM, Wehner MR, Nead KT. Association of second-generation antiandrogens with cognitive and functional toxic effects in randomized clinical trials: a systematic review and meta-analysis. JAMA Oncol. 2023;9:930–7.
Myint ZW, Momo HD, Otto DE, Yan D, Wang P, Kolesar JM. Evaluation of fall and fracture risk among men with prostate cancer treated with androgen receptor inhibitors: a systematic review and meta-analysis. JAMA Netw Open. 2020;3:e2025826.
Golshayan AR, Antonarakis ES. Enzalutamide: an evidence-based review of its use in the treatment of prostate cancer. Core Evid. 2013;8:27–35.
Morgans AK, Shore N, Cope D, McNatty A, Moslehi J, Gomella L, et al. Androgen receptor inhibitor treatments: cardiovascular adverse events and comorbidity considerations in patients with non-metastatic prostate cancer. Urol Oncol. 2021;39:52–62.
Hussain M, Fizazi K, Saad F, Rathenborg P, Shore N, Ferreira U, et al. Enzalutamide in men with nonmetastatic, castration-resistant prostate cancer. N Engl J Med. 2018;378:2465–74.
Armstrong AJ, Szmulewitz RZ, Petrylak DP, Holzbeierlein J, Villers A, Azad A, et al. ARCHES: a randomized, phase III study of androgen deprivation therapy with enzalutamide or placebo in men with metastatic hormone-sensitive prostate cancer. J Clin Oncol. 2019;37:2974–86.
Davis ID, Martin AJ, Stockler MR, Begbie S, Chi KN, Chowdhury S, et al. Enzalutamide with standard first-line therapy in metastatic prostate cancer. N Engl J Med. 2019;381:121–31.
Smith MR, Yu MK, Small EJ. Apalutamide and metastasis-free survival in prostate cancer. N Engl J Med. 2018;378:2542.
Chi KN, Agarwal N, Bjartell A, Chung BH, Pereira de Santana Gomes AJ, Given R, et al. Apalutamide for metastatic, castration-sensitive prostate cancer. N Engl J Med. 2019;381:13–24.
Turco F, Gillessen S, Cathomas R, Buttigliero C, Vogl UM. Treatment landscape for patients with castration-resistant prostate cancer: patient selection and unmet clinical needs. Res Rep Urol. 2022;14:339–50.
Bargiota A, Oeconomou A, Zachos I, Samarinas M, Pisters LL, Tzortzis V. Adverse effects of androgen deprivation therapy in patients with prostate cancer: Focus on muscle and bone health. J BUON. 2020;25:1286–94.
Taylor LG, Canfield SE, Du XL. Review of major adverse effects of androgen-deprivation therapy in men with prostate cancer. Cancer. 2009;115:2388–99.
Cornford P, van den Bergh RCN, Briers E, Van den Broeck T, Cumberbatch MG, De Santis M, et al. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer. Part II-2020 update: treatment of relapsing and metastatic prostate cancer. Eur Urol. 2021;79:263–82.
Coleman R, Hadji P, Body JJ, Santini D, Chow E, Terpos E, et al. Bone health in cancer: ESMO Clinical Practice Guidelines. Ann Oncol. 2020;31:1650–63.
Greenspan SL, Wagner J, Nelson JB, Perera S, Britton C, Resnick NM. Vertebral fractures and trabecular microstructure in men with prostate cancer on androgen deprivation therapy. J Bone Min Res. 2013;28:325–32.
Santini D, Berruti A, Di Maio M, Procopio G, Bracarda S, Ibrahim T, et al. Bone health management in the continuum of prostate cancer disease: a review of the evidence with an expert panel opinion. ESMO Open. 2020;5:e000652.
Roubaud G, Kostine M, McDermott RS, Bernard-Tessier A, Maldonado X, Silva M, et al. Bone mineral density in men with de novo metastatic castration-sensitive prostate cancer treated with or without abiraterone plus prednisone in the PEACE-1 phase 3 trial. J Clin Oncol. 2022;40:19–19.
Del Re M, Fogli S, Derosa L, Massari F, De Souza P, Crucitta S, et al. The role of drug-drug interactions in prostate cancer treatment: focus on abiraterone acetate/prednisone and enzalutamide. Cancer Treat Rev. 2017;55:71–82.
Duran I, Carles J, Bulat I, Hellemans P, Mitselos A, Ward P, et al. Pharmacokinetic drug-drug interaction of apalutamide, Part 1: clinical studies in healthy men and patients with castration-resistant prostate cancer. Clin Pharmacokinet. 2020;59:1135–48.
Zurth C, Koskinen M, Fricke R, Prien O, Korjamo T, Graudenz K, et al. Drug-drug interaction potential of darolutamide: in vitro and clinical studies. Eur J Drug Metab Pharmacokinet. 2019;44:747–59.
Shore N, Zurth C, Fricke R, Gieschen H, Graudenz K, Koskinen M, et al. Evaluation of clinically relevant drug-drug interactions and population pharmacokinetics of darolutamide in patients with nonmetastatic castration-resistant prostate cancer: results of pre-specified and post hoc analyses of the phase III ARAMIS trial. Target Oncol. 2019;14:527–39.
Boyle HJ, Alibhai S, Decoster L, Efstathiou E, Fizazi K, Mottet N, et al. Updated recommendations of the International Society of Geriatric Oncology on prostate cancer management in older patients. Eur J Cancer. 2019;116:116–36.
Author information
Authors and Affiliations
Contributions
FT: conception and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, statistical analysis, supervision. SG: conception and design, acquisition of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, supervision. GT: conception and design, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, statistical analysis, supervision. KF: critical revision of the manuscript for important intellectual content. MRS: critical revision of the manuscript for important intellectual content. BT: critical revision of the manuscript for important intellectual content. RC: critical revision of the manuscript for important intellectual content. CB: critical revision of the manuscript for important intellectual content. MDM: critical revision of the manuscript for important intellectual content. MT: critical revision of the manuscript for important intellectual content. UV: conception and design, acquisition of data, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, statistical analysis, supervision.
Corresponding author
Ethics declarations
Competing interests
FT: travel grant: Bayer. SG: (last 3 years) personal honoraria advisory boards from Amgen, MSD; invited speaker ESMO, Swiss group for Clinical Cancer Research (SAKK), German-speaking European School of Oncology (DESO), Swiss Academy of Multidisciplinary oncology (SAMO); travel grant from AstraZeneca, Bayer. Institutional honoraria advisory boards or in Independent Data Monitoring-/Steering Committees from AAA International, Amgen, AstraZeneca, Astellas Pharma, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, DAIICHI Sankyo, Innomedia, Ipsen, Modra Pharmaceuticals, MSD, Myriad Genetic, Novartis, Orion, Pfizer, Roche, Telixpharma; invited speaker SAKK, ASCO GU, ESMO, PeerVoice, Silvio Grasso Consulting, WebMD-Medscape. Patent for a research method for biomarker WO2009138392. GT: no conflicts of interest. KF: participation in advisory boards and talks for Amgen, Astellas, AstraZeneca, Bayer, Clovis, Daiichi Sankyo, Janssen, MSD, Novartis/AAA, Pfizer, Sanofi Honoraria go to Gustave Roussy, my institution. Participation to advisory boards with personal honorarium for Arvinas, CureVac, Macrogenics and Orion. MRS: consultant to Ambrx, Astellas, Bayer, Pfizer, Janssen, Lilly. BT: consultant and advisor for Amgen, Astellas, AstraZeneca, Bayer, Ferring, Janssen, Myovant, Novartis, Pfizer. RC: consultation or participation at advisory boards (institutional): AstraZeneca, Astellas, Bayer, Janssen, Roche, Pfizer, Novartis, MSD, BMS, Ipsen, Debiopharm, Accord, Merck; honoraria (institutional): Ipsen, Astellas, Janssen, Merck Travel support (institutional): Ipsen. CB: no conflicts of interest. MDM: honoraria from AstraZeneca, Boehringer Ingelheim, Janssen, Merck Sharp & Dohme (MSD), Novartis, Pfizer, Roche, GlaxoSmithKline, Amgen, Merck, Takeda for consultancy or participation to advisory boards; institutional research funding from Tesaro/GlaxoSmithKline; institutional funding for work in clinical trials/contracted research from Beigene, Exelixis, MSD, Pfizer and Roche. MT: no conflicts of interest. UV: grant: Fond’Action; Institutional: Pfizer, Astellas, Janssen, Sanofi, Merck, MSD, BMS, Ipsen, Health Book, Novartis, Bayer Private: Health Book, SAMO, Inselspital Bern, Kantonsspital Chur, Kantonsspital Baden, Ipsen; Travel Grant: AstraZeneca, Janssen.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Turco, F., Gillessen, S., Treglia, G. et al. Safety profile of darolutamide versus placebo: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis (2023). https://doi.org/10.1038/s41391-023-00775-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-023-00775-y