Abstract
Background
The prognostic nutritional index (PNI) integrates both nutritional and immune indicators and provides promising prognostic value for various malignancies. However, there is still no specific consensus relating to the precise relationship between the pretreatment PNI and the survival outcome of patients with prostate cancer (PCa). Here, we performed a meta-analysis to determine the prognostic significance of PNI for patients with PCa.
Methods
We used the PubMed, EMBASE, Web of Science, Cochrane Library (CENTRAL), and CNKI databases to identify and retrieve eligible articles that were published in any language up to the 1st March 2023. Our analysis considered hazard ratios (HRs) and 95% confidence intervals (CIs) published in the included studies. Data synthesis and analysis were conducted using Stata 15.1 software.
Results
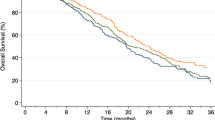
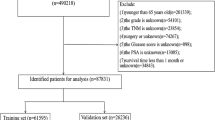
A total of ten studies featuring 1631 cases were included in our quantitative analysis. Analysis showed that a low PNI at baseline was significantly associated with poor overall survival (OS) (HR: 2.16; 95% CI: 1.40–3.34; p = 0.01), progression-free survival (PFS) (HR: 2.17; 95% CI 1.63–2.89; p < 0.001). Owing to high levels of heterogeneity, we performed subgroup analysis based on disease staging, sample size, and cutoff value; we found that disease staging may have been the source of the heterogeneity. A low pretreatment PNI was associated with poor survival outcomes for both metastatic castration-resistant prostate cancer (mCRPC) patients and nonmetastatic castration-resistant prostate cancer (nmCRPC) patients.
Conclusions
A low pretreatment PNI was significantly correlated with a worse OS and PFS in patients with PCa. A low pretreatment PNI may act as a reliable and effective predictor for the prognosis of patients with PCa. Further well-designed studies should be performed to fully evaluate the prognostic performance of this novel indicator for PCa.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Schaeffer E, Srinivas S, Antonarakis ES, Armstrong AJ, Bekelman JE, Cheng H, et al. NCCN guidelines insights: prostate cancer, version 1.2021. J Natl Compr Cancer Netw. 2021;19:134–43.
Shore ND, Laliberté F, Ionescu-Ittu R, Yang L, Mahendran M, Lejeune D, et al. Real-world treatment patterns and overall survival of patients with metastatic castration-resistant prostate cancer in the US prior to PARP inhibitors. Adv Ther. 2021;38:4520–40.
Parker C, Castro E, Fizazi K, Heidenreich A, Ost P, Procopio G, et al. Prostate cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31:1119–34.
Humphrey PA. Histopathology of prostate cancer. Cold Spring Harb Perspect Med. 2017;7:a030411.
Srigley JR, Delahunt B, Samaratunga H, Billis A, Cheng L, Clouston D, et al. Controversial issues in Gleason and International Society of Urological Pathology (ISUP) prostate cancer grading: proposed recommendations for international implementation. Pathology. 2019;51:463–73.
Huszno J, Kołosza Z, Mrochem-Kwarciak J, Telka E, Jochymek B, Miszczyk L. Role of neutrophil-lymphocyte ratio, platelet-lymphocyte ratio, lymphocyte-monocyte ratio and platelets in prognosis of patients with prostate cancer. Oncol Lett. 2022;24:305.
Yin X, Xiao Y, Li F, Qi S, Yin Z, Gao J. Prognostic role of neutrophil-to-lymphocyte ratio in prostate cancer: a systematic review and meta-analysis. Medicine. 2016;95:e2544.
Sejima T, Iwamoto H, Masago T, Morizane S, Yao A, Isoyama T, et al. Low pre-operative levels of serum albumin predict lymph node metastases and ultimately correlate with a biochemical recurrence of prostate cancer in radical prostatectomy patients. Cent Eur J Urol. 2013;66:126–32.
Okamoto T, Hatakeyama S, Narita S, Takahashi M, Sakurai T, Kawamura S, et al. Impact of nutritional status on the prognosis of patients with metastatic hormone-naive prostate cancer: a multicenter retrospective cohort study in Japan. World J Urol. 2019;37:1827–35.
Chang L-W, Hung S-C, Li J-R, Chiu K-Y, Yang C-K, Chen C-S, et al. Geriatric nutritional risk index as a prognostic marker for patients with metastatic castration-resistant prostate cancer receiving docetaxel. Front Pharmacol. 2021;11:601513.
Buzby GP, Mullen JL, Matthews DC, Hobbs CL, Rosato EF. Prognostic nutritional index in gastrointestinal surgery. Am J Surg. 1980;139:160–7.
Sun K, Chen S, Xu J, Li G, He Y. The prognostic significance of the prognostic nutritional index in cancer: a systematic review and meta-analysis. J Cancer Res Clin Oncol. 2014;140:1537–49.
Wang Z, Wang Y, Zhang X, Zhang T. Pretreatment prognostic nutritional index as a prognostic factor in lung cancer: review and meta-analysis. Clin Chim Acta Int J Clin Chem. 2018;486:303–10.
Fan L, Wang X, Chi C, Wang Y, Cai W, Shao X, et al. Prognostic nutritional index predicts initial response to treatment and prognosis in metastatic castration-resistant prostate cancer patients treated with abiraterone. Prostate. 2017;77:1233–41.
Küçükarda A, Gökyer A, Gökmen I, Özcan E, Hacıoğlu MB, Erdoğan B, et al. Prognostic nutritional index is an independent prognostic factor for treatment response, survival and drug choice in metastatic castration-resistant prostate cancer treated with abiraterone acetate or enzalutamide. Actas Urol Esp. 2022;46:301–9.
Ma Y, Yang D, Tian P, Zhao P, Feng C. Prognostic factors in patients with high-volume disease metastatic hormone-sensitive prostate cancer. Chin J Exp Surg. 2022;39:741–4.
Guo Y, Wang R, Zhang W, Mao S, Wu Y, Liu J, et al. Preoperative nutritional risk index predicts recurrence of oligometastatic prostate cancer in patients undergoing cytoreductive radical prostatectomy. Nutr Cancer Int J. 2021;73:1440–7.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14:45.
Shu K, Zhao J, Chen J, Zhang X, Zhang H, Dai J, et al. Evaluation of the prognostic nutritional index for the prognosis of patients with high/extremely high-risk prostate cancer after radical prostatectomy. J Sichuan Univ. 2019;50:99–101.
Li B, Lu Z, Wang S, Hou J, Xia G, Li H, et al. Pretreatment elevated prognostic nutritional index predicts a favorable prognosis in patients with prostate cancer. BMC Cancer. 2020;20:361.
Li N, Song W-J, Gao J, Xu Z-P, Long Z, Liu J-Y, et al. The prognostic nutritional index predicts the biochemical recurrence of patients treated with robot-assisted laparoscopic radical prostatectomy. Prostate. 2022;82:221–6.
Liang Y, Zhang Y, Chen M, Guan H, Li W, Liu B, et al. Predictive value of the pre-operative prognostic nutrition index for the survival of patients undergoing radical prostatectomy. Chin J Gen Pract. 2022;20:224–7.
Sun F, Li H, Tao T, Zhu T, Li Y, Ge L, et al. Significance of PNI and NLR for predicting initial efficacy and prognosis in the metastatic castration-resistant prostate cancer patients treated with abiraterone acetate and prednisone. J Benbu Med Coll. 2022;47:856–61.
Wang X, Mei G. Prognostic nutrition index as a predictive tool to evaluate the prognosis of pre-treatment prostate cancer patients. Electron J Metab Nutr Cancer. 2022;9:70–3.
Yang F, Pan M, Nie J, Xiao F, Zhang Y. Evaluation of the prognostic nutritional index for the prognosis of Chinese patients with high/extremely high-risk prostate cancer after radical prostatectomy. World J Clin Cases. 2022;10:8863–71.
George DJ, Sartor O, Miller K, Saad F, Tombal B, Kalinovský J, et al. Treatment patterns and outcomes in patients with metastatic castration-resistant prostate cancer in a real-world clinical practice setting in the United States. Clin Genitourin Cancer. 2020;18:284–94.
Higano CS, Sternberg CN, Saad F, Tombal BF, Miller K, Kalinovsky J, et al. Treatment patterns and outcomes for metastatic castration-resistant prostate cancer (mCRPC) in a real-world setting: a retrospective study of greater than 2500 patients. J Clin Oncol. 2019;37:256.
Clarke N, Wiechno P, Alekseev B, Sala N, Jones R, Kocak I, et al. Olaparib combined with abiraterone in patients with metastatic castration-resistant prostate cancer: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Oncol. 2018;19:975–86.
Clarke NW, Armstrong AJ, Thiery-Vuillemin A, Oya M, Shore N, Loredo E, et al. Abiraterone and olaparib for metastatic castration-resistant prostate cancer. NEJM Evid. 2022;1:1–16.
Chandra RK. Nutrition and the immune system: an introduction. Am J Clin Nutr. 1997;66:460s–3s.
Castillo-Martínez L, Castro-Eguiluz D, Copca-Mendoza ET, Pérez-Camargo DA, Reyes-Torres CA, Ávila EA, et al. Nutritional assessment tools for the identification of malnutrition and nutritional risk associated with cancer treatment. Rev Invest Clin. 2018;70:121–5.
Gupta D, Lis CG. Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J. 2010;9:69.
Liu X, Meng QH, Ye Y, Hildebrandt MA, Gu J, Wu X. Prognostic significance of pretreatment serum levels of albumin, LDH and total bilirubin in patients with non-metastatic breast cancer. Carcinogenesis. 2015;36:243–8.
Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent JP, Nicolis I, et al. Geriatric nutritional risk index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. 2005;82:777–83.
Lv GY, An L, Sun DW. Geriatric nutritional risk index predicts adverse outcomes in human malignancy: a meta-analysis. Dis Markers. 2019;2019:4796598.
Wang S, Wu T, Hu C, Fan J, Liu Y, Xu Y, et al. Preoperative nutritional evaluation of prostate cancer patients undergoing laparoscopic radical prostatectomy. PLoS ONE. 2022;17:e0262630.
Grisaru-Tal S, Dulberg S, Beck L, Zhang C, Itan M, Hediyeh-Zadeh S, et al. Metastasis-entrained eosinophils enhance lymphocyte-mediated antitumor immunity. Cancer Res. 2021;81:5555–71.
Dunn GP, Old LJ, Schreiber RD. The immunobiology of cancer immunosurveillance and immunoediting. Immunity. 2004;21:137–48.
Huang SH, Waldron JN, Milosevic M, Shen X, Ringash J, Su J, et al. Prognostic value of pretreatment circulating neutrophils, monocytes, and lymphocytes in oropharyngeal cancer stratified by human papillomavirus status. Cancer. 2015;121:545–55.
Gooden MJ, de Bock GH, Leffers N, Daemen T, Nijman HW. The prognostic influence of tumour-infiltrating lymphocytes in cancer: a systematic review with meta-analysis. Br J Cancer. 2011;105:93–103.
Ferro M, Musi G, Serino A, Cozzi G, Mistretta FA, Costa B, et al. Neutrophil, platelets, and eosinophil to lymphocyte ratios predict Gleason score upgrading in low-risk prostate cancer patients. Urol Int. 2019;102:43–50.
Lopez P, Newton RU, Taaffe DR, Singh F, Buffart LM, Spry N, et al. Associations of fat and muscle mass with overall survival in men with prostate cancer: a systematic review with meta-analysis. Prostate Cancer Prostatic Dis. 2022;25:615–26.
Funding
This study was supported by the Key Research and Development Projects of Sichuan Science and Technology Department (References: 23ZDYF2070, 2022YFS0135) and the Popular Application Reference: SCR2023-210).
Author information
Authors and Affiliations
Contributions
YZ, KW and SR: study conception and design, acquisition of data, analysis and interpretation of data and manuscript drafting. YO, YZ and ZW: acquisition of data, analysis, and interpretation of data. XH: acquisition of data, manuscript drafting and critical revision. YZ and SR: study conception and design, manuscript drafting and critical revision. DW, XL and YZ: study conception and design, manuscript drafting and critical revision. YZ and SR: study conception and design, acquisition of data, manuscript drafting and critical revision.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zheng, Y., Wang, K., Ou, Y. et al. Prognostic value of a baseline prognostic nutritional index for patients with prostate cancer: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis (2023). https://doi.org/10.1038/s41391-023-00689-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-023-00689-9