Abstract
Introduction
Benign prostatic hyperplasia (BPH) is one of the most common diseases affecting men and can present with bothersome lower urinary tract symptoms (LUTS). Historically, transurethral resection of the prostate (TURP) has been considered the gold standard in the treatment of LUTS due to BPH. However, TURP and other traditional options for the surgical management of LUTS secondary to BPH are associated with high rates of sexual dysfunction. In the past decade, several novel technologies, including Aquablation therapy, convective water vapor therapy (Rezum), and transperineal prostate laser ablation (TPLA), have demonstrated promising evidence to be safe and effective while preserving sexual function.
Methods
In this review, we discuss three ablative minimally invasive surgeries: Aquablation, Rezum, and TPLA. We review their techniques, safety, as well as perioperative and functional outcomes. We go into further detail regarding sexual function after these ablative minimally invasive surgical therapies.
Results
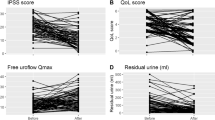
Aquablation is a surgeon-guided, robot-executed, heat-free ablative waterjet procedure with sustained functional outcomes at 5 years while having no effect on sexual activity. Rezum is an innovative office-based, minimally invasive surgical option for BPH that delivers convective water vapor energy into prostate adenoma to ablate obstructing tissue. Rezum leads to significant improvements in Qmax, IPSS while preserving sexual function. TPLA is another office-based technology which uses a diode laser source to produce thermoablation. It leads to improvement in Qmax, IPSS, and QoL while preserving ejaculatory function.
Conclusions
Overall, ablative minimally invasive surgical therapies have demonstrated excellent safety and efficacy profiles while preserving sexual function. These modalities should be discussed with patients to ensure informed and shared decision-making. Ablative minimally invasive surgical therapies may be particularly interesting to patients who value the preservation of their sexual function.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Zhang S-J, Qian H-N, Zhao Y, Sun K, Wang H-Q, Liang G-Q, et al. Relationship between age and prostate size. Asian J Androl 2013;15:116–20.
Rosen R, Altwein J, Boyle P, Kirby RS, Lukacs B, Meuleman E. et al. Lower urinary tract symptoms and male sexual dysfunction: The multinational survey of the aging.male (MSAM-7). Prog Urol. 2004;14:332–44.
Egan KB, Burnett AL, McVary KT, Ni X, Suh M, Wong DG, et al. The Co-occurring Syndrome—Coexisting Erectile Dysfunction and Benign Prostatic Hyperplasia and Their Clinical Correlates in Aging Men: Results From the National Health and Nutrition Examination Survey. Urology 2015;86:570–80.
Lusty A, Siemens DR, Tohidi M, Whitehead M, Tranmer J, Nickel JC. Cardiac Failure Associated with Medical Therapy of Benign Prostatic Hyperplasia: A Population Based Study. J Urol. 2021;205:1430–7.
Nguyen D-D, Herzog P, Cone EB, Labban M, Zorn KC, Chughtai B, et al. Disproportional signal of sexual dysfunction reports associated with finasteride use in young men with androgenetic alopecia: A pharmacovigilance analysis of VigiBase. J Am Acad Dermatol. 2023;88:179–81.
Nguyen D-D, Marchese M, Cone EB, Paciotti M, Basaria S, Bhojani N, et al. Investigation of Suicidality and Psychological Adverse Events in Patients Treated With Finasteride. JAMA Dermatol. 2021;157:35–42.
Cindolo L, Fanizza C, Romero M, Pirozzi L, Autorino R, Berardinelli F, et al. The effects of dutasteride and finasteride on BPH-related hospitalization, surgery and prostate cancer diagnosis: a record-linkage analysis. World J Urol. 2013;31:665–71.
Sugianto R, Tirtayasa PMW, Duarsa GWK. A comprehensive review of medical therapy on benign prostatic hyperplasia. Sexologies 2022;31:52–60.
Ahyai SA, Gilling P, Kaplan SA, Kuntz RM, Madersbacher S, Montorsi F, et al. Meta-analysis of Functional Outcomes and Complications Following Transurethral Procedures for Lower Urinary Tract Symptoms Resulting from Benign Prostatic Enlargement. Eur Urol 2010;58:384–97.
Bouhadana D, Nguyen D-D, Raizenne B, Schwarcz J, Gordon H, Chughtai B, et al. Evaluating the acceptability of an online patient decision aid for the surgical management of lower urinary tract symptoms secondary to benign prostatic hyperplasia. Can Urol Assoc J. 2021;15:247–54.
Malde S, Umbach R, Wheeler JR, Lytvyn L, Cornu J-N, Gacci M, et al. A Systematic Review of Patients’ Values, Preferences, and Expectations for the Diagnosis and Treatment of Male Lower Urinary Tract Symptoms. Eur Urol. 2021;79:796–809.
Bouhadana D, Nguyen D-D, Zorn KC, Elterman DS, Bhojani N. Patient perspectives on benign prostatic hyperplasia surgery: A focus on sexual health. J Sex Med. 2020;17:2108–12.
Sadri I, Arezki A, Couture F, Nguyen D-D, Schwartz R, Zakaria AS, et al. Reasons to overthrow TURP: Bring on Aquablation. World J Urol. 2021;39:2291–9.
Gilling P, Barber N, Bidair M, Anderson P, Sutton M, Aho T, et al. WATER: A Double-Blind, Randomized, Controlled Trial of Aquablation vs Transurethral Resection of the Prostate in Benign Prostatic Hyperplasia. J Urol. 2018;199:1252–61.
Desai M, Bidair M, Bhojani N, Trainer A, Arther A, Kramolowsky E, et al. WATER II (80-150 mL) procedural outcomes. BJU Int. 2019;123:106–12.
Lerner LB, McVary KT, Barry MJ, Bixler BR, Dahm P, Das AK, et al. Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia: AUA GUIDELINE PART II-Surgical Evaluation and Treatment. J Urol. 2021;206:818–26.
Elterman D, Aubé-Peterkin M, Evans H, Elmansy H, Meskawi M, Zorn KC, et al. UPDATE – 2022 Canadian Urological Association guideline on male lower urinary tract symptoms/benign prostatic hyperplasia (MLUTS/BPH). Canadian Urol Assoc J. 2022;16. https://doi.org/10.5489/cuaj.7906.
Management of Non-neurogenic Male LUTS. Uroweb - European Association of Urology. https://uroweb.org/guidelines/management-of-non-neurogenic-male-luts/chapter/disease-management (accessed 3 Jan 2023).
Nguyen D-D, Barber N, Bidair M, Gilling P, Anderson P, Zorn KC, et al. Waterjet Ablation Therapy for Endoscopic Resection of prostate tissue trial (WATER) vs WATER II: comparing Aquablation therapy for benign prostatic hyperplasia in 30-80 and 80-150 mL prostates. BJU Int. 2020;125:112–22.
Bhojani N, Nguyen D-D, Kaufman RP Jr., Elterman D, Zorn KC. Comparison of 100 cc prostates undergoing aquablation for benign prostatic hyperplasia. World J Urol. 2019;37:1361–8.
Nguyen D-D, Mantri SS, Zorn KC, Misraï V, Elterman D, Bhojani N. Which anatomic structures should be preserved during aquablation contour planning to optimize ejaculatory function? A case-control study using ultrasound video recordings to identify surgical predictors of postoperative anejaculation. Urology. 2021;153:250–5.
Elterman D, Bach T, Rijo E, Misrai V, Anderson P, Zorn KC, et al. Transfusion rates after 800 Aquablation procedures using various haemostasis methods. BJU Int. 2020;125:568–72.
MacRae C, Gilling P. How I do it: Aquablation of the prostate using the AQUABEAM system. Can J Urol. 2016;23:8590–3.
El Hajj A, Misrai V, Nasrallah AA, Labban ML, Najdi JA, Rijo E. Learning curve in aquablation: an international multicenter study. World J Urol. 2022;40:773–9.
Nguyen D-D, Misraï V, Bach T, Bhojani N, Lingeman JE, Elterman DS, et al. Operative time comparison of aquablation, greenlight PVP, ThuLEP, GreenLEP, and HoLEP. World J Urol. 2020;38:3227–33.
Bach T, Giannakis I, Bachmann A, Fiori C, Gomez-Sancha F, Herrmann TRW, et al. Aquablation of the prostate: single-center results of a non-selected, consecutive patient cohort. World J Urol. 2019;37:1369–75.
Bach T, Gilling P, El Hajj A, Anderson P, Barber N. First Multi-Center All-Comers Study for the Aquablation Procedure. J Clin Med Res. 2020;9. https://doi.org/10.3390/jcm9020603.
Elterman D, Gilling P, Roehrborn C, Barber N, Misrai V, Zorn KC, et al. Meta-analysis with individual data of functional outcomes following Aquablation for lower urinary tract symptoms due to BPH in various prostate anatomies. BMJ Surg Inter Health Technol. 2021;3:e000090.
Assad A, Nguyen D-D, Barber N, Bidair M, Gilling P, Anderson P, et al. WATER vs WATER II 3-Year Update: Comparing Aquablation Therapy for Benign Prostatic Hyperplasia in 30-80 cc and 80-150 cc Prostates. Urology. 2022;165:268–74.
Nguyen D-D, Barber N, Bidair M, Gilling P, Anderson P, Zorn KC, et al. WATER versus WATER II 2-Year Update: Comparing Aquablation Therapy for Benign Prostatic Hyperplasia in 30-80-cm and 80-150-cm Prostates. Eur Urol Open Sci. 2021;25:21–28.
Gilling PJ, Barber N, Bidair M, Anderson P, Sutton M, Aho T, et al. Five-year outcomes for Aquablation therapy compared to TURP: results from a double-blind, randomized trial in men with LUTS due to BPH. Can J Urol. 2022;29:10960–8.
Bhojani N. Aquablation for benign prostatic hyperplasia in large prostates (80-150cc): 4-year results. Eur Urol. 2022;81:S1313–S1314.
Bhojani N, Yafi FA, Misrai V, Rijo E, Chughtai B, Zorn KC, et al. Review of Sexual Preservation After Novel Benign Prostatic Hyperplasia Surgical Treatment Modalities From Food and Drug Administration Clinical Trials. Sex Med Rev. 2021;9:169–73.
Zorn KC, Bidair M, Trainer A, Arther A, Kramolowsky E, Desai M, et al. Aquablation therapy in large prostates (80-150 cc) for lower urinary tract symptoms due to benign prostatic hyperplasia: WATER II 3-year trial results. BJUI Compass. 2022;3:130–8.
McVary KT, Gittelman MC, Goldberg KA, Patel K, Shore ND, Levin RM, et al. Final 5-Year Outcomes of the Multicenter Randomized Sham-Controlled Trial of a Water Vapor Thermal Therapy for Treatment of Moderate to Severe Lower Urinary Tract Symptoms Secondary to Benign Prostatic Hyperplasia. J Urol. 2021;206:715–24.
McVary KT, El-Arabi A, Roehrborn C. Preservation of sexual function 5 years after water vapor thermal therapy for benign prostatic hyperplasia. Sex Med. 2021;9:100454.
Dixon CM, Rijo Cedano E, Mynderse LA, Larson TR. Transurethral convective water vapor as a treatment for lower urinary tract symptomatology due to benign prostatic hyperplasia using the Rezūm(®) system: evaluation of acute ablative capabilities in the human prostate. Res Rep Urol. 2015;7:13–18.
Arezki A, Sadri I, Couture F, Schwartz R, Nguyen D-D, Zakaria AS, et al. Reasons to go for Rezūm steam therapy: an effective and durable outpatient minimally invasive procedure. World J Urol. 2021;39:2307–13.
Woo HH, Gonzalez RR. Perspective on the Rezūm System: A minimally invasive treatment strategy for benign prostatic hyperplasia using convective radiofrequency water vapor thermal therapy. Med Devices. 2017;10:71–80.
Gauhar V, Lim EJ, Khan TY, Law YXT, Choo ZW, Castellani D, et al. Rezum to the rescue: Early outcomes of Rezum on patients with recurrent lower urinary tract symptoms after surgical interventions for benign prostatic enlargement. Andrologia. 2022; 54. https://doi.org/10.1111/and.14450.
Elterman D, Bhojani N, Vannabouathong C, Chughtai B, Zorn KC. Rezūm therapy for ≥ 80‐ mL benign prostatic enlargement: a large, multicentre cohort study. BJU Int. 2022;130:522–7.
Elterman D, Bhojani N, Vannabouathong C, Chughtai B, Zorn KC. Large, multi-center, prospective registry of rezūm water vapor therapy for benign prostatic hyperplasia. Urology. 2022;165:261–7.
Dixon C, Cedano ER, Pacik D, Vit V, Varga G, Wagrell L, et al. Two-year results after convective radiofrequency water vapor thermal therapy of symptomatic benign prostatic hyperplasia. Res Rep Urol. 2016;8:207–16.
Cindolo L, Campobasso D, Conti E, Uricchio F, Franzoso F, Maruzzi D, et al. Do Patients Treated with Water Vapor Therapy and Meeting Randomized Clinical Trial Criteria Have Better Urinary and Sexual Outcomes Than an Unselected Cohort. J Endourol. 2022. https://doi.org/10.1089/end.2022.0637.
Eredics K, Wehrberger C, Henning A, Sevcenco S, Marszalek M, Rauchenwald M, et al. Rezūm water vapor therapy in multimorbid patients with urinary retention and catheter dependency. Prostate Cancer Prostatic Dis. 2022;25:302–5.
Campobasso D, Siena G, Chiodini P, Conti E, Franzoso F, Maruzzi D, et al. Composite urinary and sexual outcomes after Rezum: an analysis of predictive factors from an Italian multi-centric study. Prostate Cancer Prostatic Dis. 2022. https://doi.org/10.1038/s41391-022-00587-6.
Frego N, Saita A, Casale P, Diana P, Contieri R, Avolio PP, et al. Feasibility, safety, and efficacy of ultrasound-guided transperineal laser ablation for the treatment of benign prostatic hyperplasia: a single institutional experience. World J Urol. 2021;39:3867–73.
Devices@FDA. https://www.accessdata.fda.gov/scripts/cdrh/devicesatfda/index.cfm?db=pmn&id=K213594 (accessed 30 Dec 2022).
Sessa F, Bisegna C, Polverino P, Gacci M, Siena G, Cocci A, et al. Transperineal laser ablation of the prostate (TPLA) for selected patients with lower urinary tract symptoms due to benign prostatic obstruction: A step-by-step guide. Urol Video J. 2022;15:100167.
Cai H-J, Fang J-H, Kong F-L, Xu C-K, Chen C-H, Wang W, et al. Ultrasound-guided transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: a new minimally invasive interventional therapy. Acta Radio. 2022;63:553–8.
Sessa F, Polverino P, Bisegna C, Siena G, Lo Re M, Spatafora P, et al. Transperineal laser ablation of the prostate with EchoLaserTM system: perioperative and short-term functional and sexual outcomes. Front Urol. 2022; 2. https://doi.org/10.3389/fruro.2022.969208.
de Rienzo G, Lorusso A, Minafra P, Zingarelli M, Papapicco G, Lucarelli G, et al. Transperineal interstitial laser ablation of the prostate, a novel option for minimally invasive treatment of benign prostatic obstruction. Eur Urol. 2021;80:95–103.
Patelli G, Ranieri A, Paganelli A, Mauri G, Pacella CM. Transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: A feasibility study. Cardiovasc Interv Radio. 2017;40:1440–6.
Manenti G, Perretta T, Calcagni A, Ferrari D, Ryan CP, Fraioli F, et al. 3-T MRI and clinical validation of ultrasound-guided transperineal laser ablation of benign prostatic hyperplasia. Eur Radio Exp. 2021;5:41.
Pacella CM, Patelli G, Iapicca G, Manenti G, Perretta T, Ryan CP, et al. Transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: a feasibility study. Results at 6 and 12 months from a retrospective multi-centric study. Prostate Cancer Prostic Dis. 2020;23:356–63.
Boeri L, Silvani C, Turetti M, Bebi C, Malfatto M, Longo F, et al. Clinical and functional outcomes of transperineal interstitial laser ablation of the prostate at medium term follow up: A single center experience. European Urology Open. Science 2022;39:S161.
McNicholas TA, Woo HH, Chin PT, Bolton D, Fernández Arjona M, Sievert K-D, et al. Minimally invasive prostatic urethral lift: surgical technique and multinational experience. Eur Urol. 2013;64:292–9.
Diaz SM, Bhojani N, Elterman D, Zorn K, Kaplan SA, Kohler TS, et al. Development of a North American coordinated registry network for surgical treatment of benign prostatic hyperplasia. World J Urol. 2022;40:2991–9.
Kaplan-Marans E, Martinez M, Wood A, Cochran J, Dubowitch E, Schulman A. Aquablation, prostatic urethral lift, and transurethral water vapor therapy: A comparison of device-related adverse events in a national registry. J Endourol. 2022;36:231–5.
Bouhadana D, Nguyen D, Schwarcz J, Gordon H, Elterman DS, Lavallée LT, et al. Development of a patient decision aid for the surgical management of lower urinary tract symptoms secondary to benign prostatic hyperplasia. BJU Int. 2021;127:131–5.
Bouhadana D, Nguyen D-D, Raizenne B, Vangala SK, Sadri I, Chughtai B, et al. Assessing the accuracy, quality, and readability of information related to the surgical management of benign prostatic hyperplasia. J Endourol. 2022;36:528–34.
Author information
Authors and Affiliations
Contributions
DDN: Project development, Data collection, Manuscript writing. TL: Project development, Data collection, Manuscript writing. RF: Data collection, Manuscript writing. MBB: Manuscript writing. AVN: Manuscript writing. BC: Project development, Manuscript editing, Supervision. KCZ: Project development, Manuscript editing, Supervision. NB: Project development, Manuscript editing, Supervision. DE: Project development, Manuscript editing, Supervision.
Corresponding author
Ethics declarations
Competing interests
Dr. Elterman is a consultant/investigator for Boston Scientific, Procept Biorobotics, Olympus, Urotronic, Prodeon, and Zenflow. Dr. Chughtai is a consultant for Boston Scientific, Olympus, Procept, and Prodeon. Dr. Zorn is a consultant/investigator for Boston Scientific and Procept BioRobotics. Dr. Bhojani is a consultant/investigator for Boston Scientific, Procept BioRobotics, and Olympus. All other authors report no relevant competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nguyen, DD., Li, T., Ferreira, R. et al. Ablative minimally invasive surgical therapies for benign prostatic hyperplasia: A review of Aquablation, Rezum, and transperineal laser prostate ablation. Prostate Cancer Prostatic Dis 27, 22–28 (2024). https://doi.org/10.1038/s41391-023-00669-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-023-00669-z
This article is cited by
-
Ejaculation sparing of classic and minimally invasive surgical treatments of LUTS/BPH
Prostate Cancer and Prostatic Diseases (2024)
-
The times have changed. Let the urologists change!
Prostate Cancer and Prostatic Diseases (2024)
-
Rezŭm water vaporization therapy versus transurethral resection of the prostate in the management of refractory urine retention: matched pair comparative multicenter experience
World Journal of Urology (2024)
-
Trans - Perineal laser ablation of the prostate in high surgical risk patients affected by severe lower urinary tract symptoms related to benign prostatic obstruction
Prostate Cancer and Prostatic Diseases (2023)