Abstract
Purpose
To investigate the effectiveness and safety of SoracteLite™—transperineal percutaneous laser ablation (TPLA) in the treatment of patients with symptomatic benign prostatic hyperplasia (BPH) at 6 and 12 months follow-up.
Methods
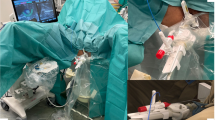
Patients with urinary symptoms secondary to BPH underwent TPLA under local anesthesia in four centers. Under US guidance, up to four 21G applicators were inserted in the prostatic tissue. Each treatment was performed with diode laser operating at 1064 nm changing the illumination time according to prostate size. The primary end-points of this study were change in IPSS, PVR, Qmax, QoL, and prostatic volume at 6 an 12 months from SoracteLiteTM TPLA treatment. Secondary end-point was the assessment of complications.
Results
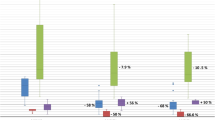
Analysis was performed on data 160 patients (mean age 69.8 ± 9.6 years) with at least 6 months follow and of 83 patients (mean age 67.9 ± 8.7 years) with at least 12 months follow-up. At 6 months, IPSS improved from 22.5 ± 5.1 to 7.7 ± 3.3 (P < 0.001), PVR from 89.5 ± 84.6 to 27.2 ± 44.5 ml (P < 0.001), Qmax from 8.0 ± 3.8 to 14.3 ± 3.9 ml/s (P < 0.001), QoL from 4.5 ± 1.1 to 1.8 ± 1.0 (P < 0.001), volume from 75.0 ± 32.4 to 60.3 ± 24.5 ml (P < 0.001). At 12 months, IPSS improved from 22.5 ± 4.5 to 7.0 ± 2.9 (P < 0.001), PVR from 71.7 ± 93.9 to 17.8 ± 51.0 ml (P < 0.001), Qmax from 8.6 ± 5.2 to 15.0 ± 4.0 ml/s (P < 0.001), QoL from 4.2 ± 0.6 to 1.6 ± 0.9 (P < 0.001), volume from 87.9 ± 31.6 to 58.8 ± 22.9 ml (P < 0.001). 7/160 (4.3%) grade I and 1/160 (0.6%) grade III complication occurred.
Conclusions
SoracteLite™ TPLA allows significant improvement of IPSS, Qol, Qmax, PVR, and reduction of prostatic volume at 6 and 12 months.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Parsons JK. Benign prostatic hyperplasia and male lower urinary tract symptoms: epidemiology and risk factors. Curr Bladder Dysfunct Rep. 2010;5:212–8.
Rosen RC, Wei JT, Althof SE, Seftel AD, Miner M, Perelman MA, et al. Association of sexual dysfunction with lower urinary tract symptoms of BPH and BPH medical therapies: results from the BPH Registry. Urology. 2009;73:562–6.
Roehrborn CG. Current medical therapies for men with lower urinary tract symptoms and benign prostatic hyperplasia: achievements and limitations. Rev Urol. 2008;10:14–25.
Cornu JN, Ahyai S, Bachmann A, de la Rosette J, Gilling P, Gratzke C, et al. A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol. 2015;67:1066–96.
Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)–incidence, management, and prevention. Eur Urol. 2006;50:969–79. discussion 980
Bouza C, Lopez T, Magro A, Navalpotro L, Amate JM. Systematic review and meta-analysis of transurethral needle ablation in symptomatic benign prostatic hyperplasia. BMC Urol. 2006;6:14.
Malaeb BS, Yu X, McBean AM, Elliott SP. National trends in surgical therapy for benign prostatic hyperplasia in the United States (2000-2008). Urology. 2012;79:1111–6.
Perera M, Roberts MJ, Doi SA, Bolton D. Prostatic urethral lift improves urinary symptoms and flow while preserving sexual function for men with benign prostatic hyperplasia: a systematic review and meta-analysis. Eur Urol. 2015;67:704–13.
Roehrborn CG, Rukstalis DB, Barkin J, Gange SN, Shore ND, Giddens JL, et al. Three year results of the prostatic urethral L.I.F.T. study. Can J Urol. 2015;22:7772–82.
Yildiz G, Bahouth Z, Halachmi S, Meyer G, Nativ O, Moskovitz B. Allium TPS–a new prostatic stent for the treatment of patients with benign prostatic obstruction: the first report. J Endourol. 2016;30:319–22.
El-Husseiny T, Buchholz N. Transurethral ethanol ablation of the prostate for symptomatic benign prostatic hyperplasia: long-term follow-up. J Endourol. 2011;25:477–80.
Shore N, Cowan B. The potential for NX-1207 in benign prostatic hyperplasia: an update for clinicians. Ther Adv Chronic Dis. 2011;2:377–83.
Elhilali MM, Pommerville P, Yocum RC, Merchant R, Roehrborn CG, Denmeade SR. Prospective, randomized, double-blind, vehicle controlled, multicenter phase IIb clinical trial of the pore forming protein PRX302 for targeted treatment of symptomatic benign prostatic hyperplasia. J Urol. 2013;189:1421–6.
Marberger M, Chartier-Kastler E, Egerdie B, Lee KS, Grosse J, Bugarin D, et al. A randomized double-blind placebo-controlled phase 2 dose-ranging study of onabotulinumtoxinA in men with benign prostatic hyperplasia. Eur Urol. 2013;63:496–503.
McVary KT, Roehrborn CG. Three-year outcomes of the prospective, randomized controlled rezum system study: convective radiofrequency thermal therapy for treatment of lower urinary tract symptoms due to benign prostatic hyperplasia. Urology. 2018;111:1–9.
Schreuder SM, Scholtens AE, Reekers JA, Bipat S. The role of prostatic arterial embolization in patients with benign prostatic hyperplasia: a systematic review. Cardiovasc Interventional Radiol. 2014;37:1198–1219.
Pisco J, Bilhim T, Costa NV, Ribeiro MP, Fernandes L, Oliveira AG. Safety and efficacy of prostatic artery chemoembolization for prostate cancer-initial experience. J Vasc Inter Radio. 2018;29:298–305.
Yassaie O, Silverman JA, Gilling PJ. Aquablation of the prostate for symptomatic benign prostatic hyperplasia: early results. Curr Urol Rep. 2017;18:91.
Gilling P, Reuther R, Kahokehr A, Fraundorfer M. Aquablation - image-guided robot-assisted waterjet ablation of the prostate: initial clinical experience. BJU Int. 2016;117:923–9.
Roberts WW. Development and translation of histotripsy: current status and future directions. Curr Opin Urol. 2014;24:104–10.
McCulloch P, Cook JA, Altman DG, Heneghan C, Diener MK, Group I. IDEAL framework for surgical innovation 1: the idea and development stages. Brit Med J. 2013;346:f3012.
Patelli G, Ranieri A, Paganelli A, Mauri G, Pacella CM. Transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: a feasibility study. Cardiovasc Interventional Radiol. 2017;40:1440–6.
Pacella CM, Francica G, Di Lascio FM, Arienti V, Antico E, Caspani B, et al. Long-term outcome of cirrhotic patients with early hepatocellular carcinoma treated with ultrasound-guided percutaneous laser ablation: a retrospective analysis. J Clin Oncol. 2009;27:2615–21.
Pacella CM, Mauri G, Achille G, Barbaro D, Bizzarri G, De Feo P, et al. Outcomes and risk factors for complications of laser ablation for thyroid nodules: a multicenter study on 1531 patients. J Clin Endocrinol Metab. 2015;100:3903–10.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Mamoulakis C, Efthimiou I, Kazoulis S, Christoulakis I, Sofras F. The modified Clavien classification system: a standardized platform for reporting complications in transurethral resection of the prostate. World J Urol. 2011;29:205–10.
Gilling P, Barber N, Bidair M, Anderson P, Sutton M, Aho T, et al. WATER: a double-blind, randomized, controlled trial of aquablation((R)) vs transurethral resection of the prostate in benign prostatic hyperplasia. J Urol. 2018;199:1252–61.
Krambeck AE, Handa SE, Lingeman JE. Experience with more than 1,000 holmium laser prostate enucleations for benign prostatic hyperplasia. J Urol. 2013;189:S141–5.
Tan AHH, Gilling PJ, Kennett KM, Frampton C, Westemberg AM, Fraundorfer MR. A randomized trial comparing holmium laser enucleation ot the prostatewith transurethral resection of the perostate for the treatment of bladder outlet obstruction secondary to benign prostatic hyperplasia in large glands (40 to 200 grams). J Urol. 2003;170:1270–4.
Kim KS, Choi JB, Bae WJ, Kim SJ, Cho HJ, Hong SH, et al. Comparison of photoselective vaporization versus Holmium laser enucleation for treatment of benign prostate hyperplasia in a small prostate volume. PLoS ONE. 2016;11:e0156133.
Jones P, Rai BP, Somani BK, Aboumarzouk OM. A review of thulium laser vapo-enucleation of the prostate: A novel laser-based strategy for benign prostate enlargement. Arab J Urol. 2015;13:209–11.
Roberts WW. New technologies in benign prostatic hyperplasia management. Curr Opin Urol. 2016;26:254–8.
Whelan JP, Bowen JM, Burke N, Woods EA, McIssac GP, Hopkins RB, et al. A prospective trial of GreenLight PVP (HPS120) versus transurethral resection of the prostate in the treatment of lower urinary tract symptoms in Ontario, Canada. Can Urol Assoc J. 2013;7:335–41.
Yu H, Isaacson AJ, Burke CT. Review of current literature for prostatic artery embolization. Semin Interv Radiol. 2016;33:231–5.
Gao YA, Huang Y, Zhang R, Yang YD, Zhang Q, Hou M, et al. Benign prostatic hyperplasia: prostatic arterial embolization versus transurethral resection of the prostate–a prospective, randomized, and controlled clinical trial. Radiology. 2014;270:920–8.
Carnevale FC, Iscaife A, Yoshinaga EM, Moreira AM, Antunes AA, Srougi M. Transurethral resection of the prostate (TURP) versus original and PErFecTED prostate artery embolization (PAE) due to benign prostatic hyperplasia (BPH): preliminary results of a single center, prospective, urodynamic-controlled analysis. Cardiovascular interventional Radiol. 2016;39:44–52.
Reich O, Gratzke C, Bachmann A, Seitz M, Schlenker B, Hermanek P, et al. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol. 2008;180:246–9.
Ruszat R, Seitz M, Wyler SF, Abe C, Rieken M, Reich O, et al. GreenLight laser vaporization of the prostate: single-center experience and long-term results after 500 procedures. Eur Urol. 2008;54:893–901.
Gilling P, Anderson P, Tan A. Aquablation of the prostate for symptomatic benign prostatic hyperplasia: 1-Year Results. J Urol. 2017;197:1565–72.
Yafi FA, Tallman CT, Seard ML, Jordan ML Aquablation outcomes for the U.S. cohort of men with LUTS due to BPH in large prostates (80–150 cc). Int J Impot Res. 2018;30:209–14.
Rassweiler MC, Mamoulakis C, Kenngott HG, Rassweiler J, de la Rosette J, Laguna MP. Classification and detection of errors in minimally invasive surgery. J Endourol. 2011;25:1713–21.
Montorsi F, Naspro R, Salonia A, Suardi N, Briganti A, Zanoni M, et al. Holmium laser enucleation versus transurethral resection of the prostate: results from a 2-center, prospective, randomized trial in patients with obstructive benign prostatic hyperplasia. J Urol. 2004;172:1926–9.
Ahyai SA, Gilling P, Kaplan SA, Kuntz RM, Madersbacher S, Montorsi F, et al. Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. Eur Urol. 2010;58:384–97.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
GM, CMP and CR: consultant for Elesta SrL. All other authors have nothing to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pacella, C.M., Patelli, G., Iapicca, G. et al. Transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: a feasibility study. Results at 6 and 12 months from a retrospective multi-centric study. Prostate Cancer Prostatic Dis 23, 356–363 (2020). https://doi.org/10.1038/s41391-019-0196-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-019-0196-4
This article is cited by
-
Ejaculation sparing of classic and minimally invasive surgical treatments of LUTS/BPH
Prostate Cancer and Prostatic Diseases (2024)
-
Ablative minimally invasive surgical therapies for benign prostatic hyperplasia: A review of Aquablation, Rezum, and transperineal laser prostate ablation
Prostate Cancer and Prostatic Diseases (2024)
-
Trans - Perineal laser ablation of the prostate in high surgical risk patients affected by severe lower urinary tract symptoms related to benign prostatic obstruction
Prostate Cancer and Prostatic Diseases (2023)
-
Ultrasound-guided SoracteLite™ transperineal laser ablation (TPLA) of the prostate for the treatment of symptomatic benign prostatic hyperplasia (BPH): a prospective single-center experience
World Journal of Urology (2023)
-
Transurethral resection of the prostate (TURP) versus transperineal laser ablation (TPLA) due to benign prostatic hyperplasia (BPH): prospective and comparative study
International Urology and Nephrology (2023)