Abstract
Background
Lymph node invasion (LNI) is a strong adverse prognostic factor in prostate cancer (PCa). The purpose of this study was to evaluate the role of Prostate Imaging Reporting and Data System version 2 (PI-RADSv2) scores for estimating the risk of LN metastasis. The study also aimed to investigate the additional value of PI-RADSv2 scores when used in combination with clinical nomograms for the prediction of LNI in patients with PCa.
Methods
We retrospectively identified 308 patients who underwent multiparametric magnetic resonance imaging (mpMRI) and RP with pelvic lymph node dissection (PLND). Clinicopathological parameters and PI-RADSv2 scores were assessed. Univariate and multivariate logistic analyses were performed. The area under the receiver operating characteristic curves (AUCs) and decision curve analysis (DCA) were generated for assessing the incremental value of PI-RADSv2 scores combined with the Briganti and Memorial Sloan Kettering Cancer Center (MSKCC) nomograms.
Results
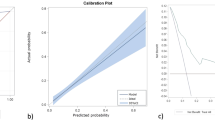
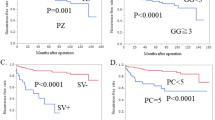
Overall, 20 (6.5%) patients had LNI. At univariate analysis, all clinicopathological characteristics and PI-RADSv2 scores were significantly associated to LNI (p < 0.04). However, multivariate analysis revealed that only PI-RADSv2 scores and percentage of positive cores were independently significant (p ≤ 0.006). The PI-RADSv2 score was the most accurate predictor (AUC, 80.2%). The threshold of PI-RADSv2 score was 5, which provided high sensitivity (18/20, 90.0%) and negative predictive value (203/205, 99.0%). When PI-RADSv2 scores were combined with Briganti and MSKCC nomograms, the AUC value increased from 75.1 to 86.3% and from 79.2 to 87.9%, respectively (p ≤ 0.001). The DCA also demonstrated that the two nomograms plus PI-RADSv2 scores improved clinical risk prediction of LNI.
Conclusions
The patients with a PI-RADSv2 score <5 were associated with a very low risk of LNI in PCa. Preoperative PI-RADSv2 scores could help improve the accuracy of clinical nomograms for predicting pelvic LN metastasis at radical prostatectomy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Schumacher MC, Burkhard FC, Thalmann GN, Fleischmann A, Studer UE. Good outcome for patients with few lymph node metastases after radical retropubic prostatectomy. Eur Urol. 2008;54:344–52.
Touijer KA, Mazzola CR, Sjoberg DD, Scardino PT, Eastham JA. Long-term outcomes of patients with lymph node metastasis treated with radical prostatectomy without adjuvant androgen-deprivation therapy. Eur Urol. 2014;65:20–5.
Boorjian SA, Thompson RH, Siddiqui S, Bagniewski S, Bergstralh EJ, Karnes RJ, et al. Long-term outcome after radical prostatectomy for patients with lymph node positive prostate cancer in the prostate specific antigen era. J Urol. 2007;178(3 Part 1):864–70. discussion 870–861.
Masterson TA, Bianco FJ Jr., Vickers AJ, DiBlasio CJ, Fearn PA, Rabbani F, et al. The association between total and positive lymph node counts, and disease progression in clinically localized prostate cancer. J Urol. 2006;175:1320–4. discussion 1324-1325.
Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M, et al. EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part 1: Screening, diagnosis, and local treatment with curative intent. Eur Urol. 2017;71:618–29.
Van Huele A, Poelaert F, Fonteyne V, Decaestecker K, Ost P, Lumen N. Pelvic lymph node dissection in prostate cancer staging: evaluation of morbidity and oncological outcomes. Acta Chir Belg. 2019;119:103–9.
Briganti A, Blute ML, Eastham JH, Graefen M, Heidenreich A, Karnes JR, et al. Pelvic lymph node dissection in prostate cancer. Eur Urol. 2009;55:1251–65.
Abdollah F, Karnes RJ, Suardi N, Cozzarini C, Gandaglia G, Fossati N, et al. Predicting survival of patients with node-positive prostate cancer following multimodal treatment. Eur Urol. 2014;65:554–62.
Briganti A, Larcher A, Abdollah F, Capitanio U, Gallina A, Suardi N, et al. Updated nomogram predicting lymph node invasion in patients with prostate cancer undergoing extended pelvic lymph node dissection: the essential importance of percentage of positive cores. Eur Urol. 2012;61:480–7.
Memorial Sloan Kettering Cancer Center Dynamic Prostate Cancer Nomogram: Coefficients. https://www.mskcc.org/nomograms/prostate/pre-op/coefficients.
Roach M 3rd, Marquez C, Yuo HS, Narayan P, Coleman L, et al. Predicting the risk of lymph node involvement using the pre-treatment prostate specific antigen and Gleason score in men with clinically localized prostate cancer. Int J Radiat Oncol Biol Phys. 1994;28:33–7.
Godoy G, Chong KT, Cronin A, Vickers A, Laudone V, Touijer K, et al. Extent of pelvic lymph node dissection and the impact of standard template dissection on nomogram prediction of lymph node involvement. Eur Urol. 2011;60:195–201.
Futterer JJ, Briganti A, De Visschere P, Emberton M, Giannarini G, Kirkham A, et al. Can clinically significant prostate cancer be detected with multiparametric magnetic resonance imaging? A systematic review of the literature. Eur Urol. 2015;68:1045–53.
Weinreb JC, Barentsz JO, Choyke PL, Cornud F, Haider MA, Macura KJ, et al. PI-RADS prostate imaging—Reporting and Data System: 2015, Version 2. Eur Urol. 2016;69:16–40.
Vargas HA, Hotker AM, Goldman DA, Moskowitz CS, Gondo T, Matsumoto K, et al. Updated prostate imaging reporting and data system (PIRADSv2) recommendations for the detection of clinically significant prostate cancer using multiparametric MRI: critical evaluation using whole-mount pathology as standard of reference. Eur Radiol. 2016;26:1606–12.
Kayat Bittencourt L, Litjens G, Hulsbergen-van de Kaa CA, Turkbey B, Gasparetto EL, Barentsz JO. Prostate Cancer: The European Society of Urogenital Radiology Prostate Imaging Reporting and Data System Criteria for Predicting Extraprostatic Extension by Using 3-T Multiparametric MR Imaging. Radiology. 2015;276:479–89.
Park SY, Oh YT, Jung DC, Cho NH, Choi YD, Rha KH, et al. Prediction of biochemical recurrence after radical prostatectomy with PI-RADS version 2 in prostate cancers: initial results. Eur Radiol. 2016;26:2502–9.
Sanda MG, Cadeddu JA, Kirkby E, Chen RC, Crispino T, Fontanarosa J, et al. Clinically localized prostate cancer: AUA/ASTRO/SUO Guideline. Part I: Risk stratification, shared decision making, and care options. J Urol. 2018;199:683–90.
Mohler JL, Antonarakis ES, Armstrong AJ, D’Amico AV, Davis BJ, Dorff T, et al. Prostate Cancer, Version 2.2019, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2019;17:479–505.
Rouviere O, Schoots IG, Mottet N. Panel E-E-E-E-SPCG. Multiparametric magnetic resonance imaging before prostate biopsy: a chain is only as strong as its weakest link. Eur Urol. 2019;75:889–90.
Park SY, Cho NH, Jung DC, Oh YT. Prostate Imaging-Reporting and Data System Version 2: beyond prostate cancer detection. Korean J Radiol. 2018;19:193–200.
Brembilla G, Dell’Oglio P, Stabile A, Ambrosi A, Cristel G, Brunetti L, et al. Preoperative multiparametric MRI of the prostate for the prediction of lymph node metastases in prostate cancer patients treated with extended pelvic lymph node dissection. Eur Radiol. 2018;28:1969–76.
Park SY, Oh YT, Jung DC, Cho NH, Choi YD, Rha KH. Prediction of micrometastasis (<1 cm) to pelvic lymph nodes in prostate cancer: role of preoperative MRI. Am J Roentgenol. 2015;205:W328–34.
Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA, et al. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: Definition of Grading Patterns and Proposal for a New Grading System. Am J Surg Pathol. 2016;40:244–52.
Bochner BH, Cho D, Herr HW, Donat M, Kattan MW, Dalbagni G. Prospectively packaged lymph node dissections with radical cystectomy: evaluation of node count variability and node mapping. J Urol. 2004;172(4 Part 1):1286–90.
Hovels AM, Heesakkers RA, Adang EM, Jager GJ, Strum S, Hoogeveen YL, et al. The diagnostic accuracy of CT and MRI in the staging of pelvic lymph nodes in patients with prostate cancer: a meta-analysis. Clin Radiol. 2008;63:387–95.
Budaus L, Leyh-Bannurah SR, Salomon G, Michl U, Heinzer H, Huland H, et al. Initial experience of (68)Ga-PSMA PET/CT imaging in high-risk prostate cancer patients prior to radical prostatectomy. Eur Urol. 2016;69:393–6.
Tay KJ, Gupta RT, Brown AF, Silverman RK, Polascik TJ. Defining the incremental utility of prostate multiparametric magnetic resonance imaging at standard and specialized read in predicting extracapsular extension of prostate cancer. Eur Urol. 2016;70:211–3.
Rayn KN, Bloom JB, Gold SA, Hale GR, Baiocco JA, Mehralivand S, et al. Added value of multiparametric magnetic resonance imaging to clinical nomograms in predicting adverse pathology in prostate cancer. J Urol. 2018;200:1041–7.
Tonttila PP, Kuisma M, Paakko E, Hirvikoski P, Vaarala MH. Lesion size on prostate magnetic resonance imaging predicts adverse radical prostatectomy pathology. Scand J Urol. 2018;52:111–5.
Hambrock T, Hoeks C, Hulsbergen-van de Kaa C, Scheenen T, Futterer J, Bouwense S, et al. Prospective assessment of prostate cancer aggressiveness using 3-T diffusion-weighted magnetic resonance imaging-guided biopsies versus a systematic 10-core transrectal ultrasound prostate biopsy cohort. Eur Urol. 2012;61:177–84.
Bittencourt LK, Barentsz JO, de Miranda LC, Gasparetto EL. Prostate MRI diffusion-weighted imaging at 1.5T correlates better with prostatectomy Gleason grades than TRUS-guided biopsies in peripheral zone tumours. Eur Radiol. 2012;22:468–75.
Liu X, Peng W, Zhou L, Wang H. Biexponential apparent diffusion coefficients values in the prostate: comparison among normal tissue, prostate cancer, benign prostatic hyperplasia and prostatitis. Korean J Radiol. 2013;14:222–32.
Zhang P, Min X, Wang L, Feng Z, Ke Z, You H, et al. Bi-exponential versus mono-exponential diffusion-weighted imaging for evaluating prostate cancer aggressiveness after radical prostatectomy: a whole-tumor histogram analysis. Acta Radiol. 2019. https://doi.org/10.1177/0284185119837932.
Jung SI, Donati OF, Vargas HA, Goldman D, Hricak H, Akin O. Transition zone prostate cancer: incremental value of diffusion-weighted endorectal MR imaging in tumor detection and assessment of aggressiveness. Radiology. 2013;269:493–503.
Le JD, Tan N, Shkolyar E, Lu DY, Kwan L, Marks LS, et al. Multifocality and prostate cancer detection by multiparametric magnetic resonance imaging: correlation with whole-mount histopathology. Eur Urol. 2015;67:569–76.
Briganti A, Chun FK, Salonia A, Zanni G, Scattoni V, Valiquette L. et al. Validation of a nomogram predicting the probability of lymph node invasion among patients undergoing radical prostatectomy and an extended pelvic lymphadenectomy. Eur Urol. 2006;49:1019–26. discussion 1026–1017.
Perry-Keene J, Ferguson P, Samaratunga H, Nacey JN, Delahunt B. Total submission of pelvic lymphadenectomy tissues removed during radical prostatectomy for prostate cancer increases lymph node yield and detection of micrometastases. Histopathology. 2014;64:399–404.
Radtke JP, Hadaschik BA, Wolf MB, Freitag MT, Schwab C, Alt C, et al. The Impact of magnetic resonance imaging on prediction of extraprostatic extension and prostatectomy outcome in patients with low-, intermediate- and high-risk prostate cancer: try to find a standard. J Endourol. 2015;29:1396–405.
Park SY, Shin SJ, Jung DC, Cho NH, Choi YD, Rha KH, et al. PI-RADS version 2: preoperative role in the detection of normal-sized pelvic lymph node metastasis in prostate cancer. Eur J Radiol. 2017;91:22–8.
Weaver JK, Kim EH, Vetter JM, Shetty A, Grubb RL 3rd, Strope SA, et al. Prostate magnetic resonance imaging provides limited incremental value over the Memorial Sloan Kettering Cancer Center preradical prostatectomy nomogram. Urology. 2018;113:119–28.
Hruby S, Englberger C, Lusuardi L, Schatz T, Kunit T, Abdel-Aal AM, et al. Fluorescence guided targeted pelvic lymph node dissection for intermediate and high risk prostate cancer. J Urol. 2015;194:357–63.
Acknowledgements
This study was funded by the National Natural Science Foundation of China (Grant Numbers: 81672546, 81602253, and 81872083) and Joint Fund of Peking University First Hospital. We thank the entire staff of the Department of Urology, Peking University First Hospital.
Author information
Authors and Affiliations
Contributions
CH and GS contributed equally to this work. GS, XYW, and LQZ conceived and designed the study. CH, HHW, ZYL, GJJ, SYZ, YSG, JL, ZQB, PH, and YCD collected the data. HHW and ZYL analyzed mpMRI results. CH, PL, QH, SMH, and YQG analyzed and interpreted the data. CH and GS drafted the manuscript. GS revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Huang, C., Song, G., Wang, H. et al. Preoperative PI-RADS Version 2 scores helps improve accuracy of clinical nomograms for predicting pelvic lymph node metastasis at radical prostatectomy. Prostate Cancer Prostatic Dis 23, 116–126 (2020). https://doi.org/10.1038/s41391-019-0164-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-019-0164-z
This article is cited by
-
The role and controversy of pelvic lymph node dissection in prostate cancer treatment: a focused review
World Journal of Surgical Oncology (2024)
-
The predictive value of machine learning and nomograms for lymph node metastasis of prostate cancer: a systematic review and meta-analysis
Prostate Cancer and Prostatic Diseases (2023)
-
A Nomogram Predicting Lymph Node Metastasis in Patients with Prostate Cancer Undergoing Ultrasound-Guided Transrectal Prostate Biopsy
Indian Journal of Surgery (2022)
-
Multiparametric MRI-based radiomics model to predict pelvic lymph node invasion for patients with prostate cancer
European Radiology (2022)
-
Prostate Cancer and Prostatic Diseases Best of Asia, 2019: challenges and opportunities
Prostate Cancer and Prostatic Diseases (2020)