Abstract
Background
Men with elevated prostate-specific antigen (PSA) and initial negative prostate biopsy may have risk of prostate cancer (PCa) in the future. The role of Prostate Health Index (phi) in determining future PCa risk has not been studied before. This study aims to investigate the role of initial phi and phi density in predicting future PCa risk in men with initial negative biopsy.
Methods
Five hundred sixty nine men with PSA 4–10 ng/mL were recruited between 2008 and 2015 for prostate biopsy with prior phi. Electronic clinical record of men with initial negative biopsy was reviewed. Patients and follow-up doctors were blinded to phi. Kaplan–Meier curves were used to analyze the PCa-free survival in different baseline phi and phi density groups.
Results
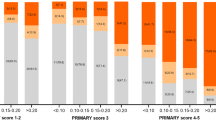
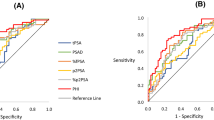
Four hundred sixty-one men with complete follow-up data were included. Median follow-up is 77 months. PCa and HGPCa was diagnosed in 8.2% (38/461) and 4.8% (22/461) of cohort respectively. A higher baseline phi value was associated with PCa (p = 0.003) and HGPCa (p < 0.001). HGPCa was diagnosed in 0.6% (1/163) of phi < 25, 4.6% (9/195) of phi 25–34.9, and 11.7% (12/103) of phi ≥ 35 (p < 0.001). HGPCa was diagnosed in 0% (0/109) and 21.0% (13/62) with phi density of <0.4 and ≥1.2, respectively, (p < 0.001). Kaplan–Meier curves showed phi and phi density predicted PCa and HGPCa diagnoses (log-rank test, all p ≤ 0.002).
Conclusions
Initial phi or phi density predicted 6-year risk of PCa in men with initial negative prostate biopsy. Men with higher phi (≥35) or phi density (≥1.2) need closer follow-up and repeated investigation, while men with lower phi (<25) or phi density (<0.4) could have less frequent follow-up.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Stamey TA, Yang N, Hay AR, McNeal JE, Freiha FS, Redwine E. Prostate-specific antigen as a serum marker for adenocarcinoma of the prostate. N Engl J Med. 1987;317:909–16.
Hugosson J, Roobol MJ, Månsson M, Tammela TLJ, Zappa M, Nelen V, et al. A 16-yr follow-up of the european randomized study of screening for prostate cancer. Eur Urol. 2019;76:43–51.
Mikolajczyk SD, Millar LS, Wang TJ, Rittenhouse HG, Marks LS, Song W, et al. A precursor form of prostate-specific antigen is more highly elevated in prostate cancer compared with benign transition zone prostate tissue. Cancer Res. 2000;60:756–9.
Filella X, Giménez N. Evaluation of [− 2] proPSA and prostate health index (phi) for the detection of prostate cancer: a systematic review and meta-analysis. Clin Chem Lab Med. 2013;51:729–39.
Catalona WJ, Partin AW, Sanda MG, Wei JT, Klee GG, Bangma CH, et al. A multicenter study of [−2]pro-prostate specific antigen combined with prostate specific antigen and free prostate specific antigen for prostate cancer detection in the 2.0 to 10.0 ng/ml prostate specific antigen range. J Urol. 2011;185:1650–5.
Chiu PK, Ng CF, Semjonow A, Zhu Y, Vincendeau S, Houlgatte A, et al. A multicentre evaluation of the role of the Prostate Health Index (phi) in regions with differing prevalence of prostate cancer: adjustment of phi reference ranges is needed for European and Asian settings. Eur Urol. 2019;75:558–61.
Ploussard G, Nicolaiew N, Marchand C, Terry S, Allory Y, Vacherot F, et al. Risk of repeat biopsy and prostate cancer detection after an initial extended negative biopsy: Longitudinal follow-up from a prospective trial. BJU Int. 2013;111:988–96.
Loeb S, Vellekoop A, Ahmed HU, Catto J, Emberton M, Nam R, et al. Systematic review of complications of prostate biopsy. Eur Urol. 2013;64:876–92.
Chiu PK, Roobol MJ, Teoh JY, Lee WM, Yip SY, Hou SM, et al. Prostate health index (phi) and prostate-specific antigen (PSA) predictive models for prostate cancer in the Chinese population and the role of digital rectal examination-estimated prostate volume. Int Urol Nephrol. 2016;48:1631–7.
Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humprey RA, et al. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol. 2016;40:244–52.
Semjonow A, Köpke T, Eltze E, Pepping-Schefers B, Burgel H, Darte C. Pre-analytical in-vitro stability of [−2]proPSA in blood and serum. Clin Chem. 2010;43:926–8.
Pannek J, Marks LS, Pearson JD, Rittenhouse HG, Chan DW, Sherry ED, et al. Influence of finasteride on free and total serum prostate specific antigen levels in men with benign prostatic hyperplasia. J Urol. 1998;159:449–53.
Mottet N, van den Burg R, Briers E, van den Brock T, Cumberbatch MG, De Santis M, et al. EAU—ESTRO—ESUR—SIOG Guidelines on Prostate Cancer. EAU Guidelines. Edn. presented at the EAU Annual Congress Amsterdam 2020. ISBN 978-94-92671-07-3.
Druskin SC, Tosoian JJ, Young A, Collica S, Srivastava A, Ghabili K, et al. Combining Prostate Health Index density, magnetic resonance imaging and prior negative biopsy status to improve the detection of clinically significant prostate cancer. BJU Int. 2018;121:619–26.
Tosoian JJ, Druskin SC, Andreas D, Mullane P, Chappidi M, Joo S, et al. Prostate Health Index density improves detection of clinically significant prostate cancer. BJU Int. 2017;120:793–8.
Huang YP, Lin TP, Cheng WM, Wei TC, Huang IS, Fan YH, et al. Prostate health index density predicts aggressive pathological outcomes after radical prostatectomy in Taiwanese patients. J Chin Med Assoc. 2019;82:835–9.
Chen R, Sjoberg DD, Huang Y, Xie LP, Zhou L, He D, et al. Prostate specific antigen and prostate cancer in Chinese men undergoing initial prostate biopsies compared with western cohorts. J Urol. 2017;197:90–6.
Cheung NT, Fung V, Kong JHB. The Hong Kong Hospital Authority’s information architecture. Stud Health Technol Inform. 2004;107:1183–6.
Ahmed HU, El-Shater BA, Brown LC, Gabe R, Kaplan R, Parmar MK, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet. 2017;389:815–22.
Kasivisvanathan V, Rannikko AS, Borghi M, Panebianco V, Mynderse LA, Vaarala MH, et al. MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med. 2018;378:1767–77.
Author information
Authors and Affiliations
Contributions
Conceptualization, MR, CFNg, PKC; Methodology, AQL, SR, PKC; formal analysis, AQL, SR, CHL; investigation, SYL, SYY; resources, CFNg; data curation, SYL, SYY, CWM, AQL; writing—original draft preparation, AQL, PKC; writing—review and editing, SR, JYT, SMH, MR; visualization, SR, CHL; supervision, MR, CFNg.; project administration, PKC; funding acquisition, CFNg.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, A.Q., Remmers, S., Lau, SY. et al. Initial Prostate Health Index (phi) and phi density predicts future risk of clinically significant prostate cancer in men with initial negative prostate biopsy: a 6-year follow-up study. Prostate Cancer Prostatic Dis 25, 684–689 (2022). https://doi.org/10.1038/s41391-021-00444-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-021-00444-y
This article is cited by
-
A prospective evaluation of the effect of finasteride on prostate health index (phi)
International Urology and Nephrology (2023)
-
Selective Bone Scan staging for patients with Prostate cancer: do absolute categories really make sense?
Prostate Cancer and Prostatic Diseases (2022)