Abstract
Background
To systematically review and analyse the associations between fat and muscle mass measures with overall survival in men with prostate cancer.
Methods
A systematic search was conducted in CINAHL, Cochrane Library, EMBASE, PubMed, and Web of Science databases from inception to December 2020, while abstracts from the American Society of Clinical Oncology (ASCO), Clinical Oncology Society of Australia (COSA), and the American College of Sports Medicine (ACSM) conferences were searched from 2014 to 2020. Eligible articles examined the association of body composition measures, such as fat mass (e.g., fat mass, visceral adipose tissue (VAT), subcutaneous adipose tissue (SAT), and VAT/SAT) and muscle mass measures, with overall survival in prostate cancer patients at any treatment stage. The primary endpoint was overall survival. Random-effect meta-analysis was conducted for studies reporting multivariable or univariable analysis assessing the associations of fat mass measures (i.e., fat mass, VAT, SAT, VAT/SAT) and muscle mass measures with overall survival.
Results
Sixteen cohort studies that comprised 4807 men with prostate cancer were included. Total adiposity (hazard ratio (HR) 0.98, 95% CI: 0.75–1.28, p = 0.888) and VAT (HR 1.03, 95% CI: 0.74–1.43, p = 0.873) were not significantly associated with overall survival, while higher subcutaneous adipose tissue levels were associated with higher survival (HR 0.68, 95% CI: 0.54–0.84, p = 0.001). Greater mortality risk was found in patients with localised (HR 1.91, 95% CI: 1.40–2.62, p < 0.001) and advanced disease (HR 1.43, 95% CI: 1.07–1.92, p = 0.020) presenting with low levels of muscle mass compared to those presenting with high levels.
Discussion
These results indicate that although overall adiposity should be cautiously interpreted in regards to survival, high muscle mass and SAT, and low VAT/SAT ratio values are associated with overall survival in men with prostate cancer.
Similar content being viewed by others
Introduction
Prostate cancer is one of the most prevalent cancers worldwide, accounting for one in five new cancer cases in men [1]. Among the available treatments, androgen deprivation therapy (ADT) is commonly used alone or in combination with other forms of therapy to delay prostate cancer progression and improve survival in patients with advanced prostate cancer [2]. However, as a result of resistance to treatment [3, 4], altered metabolic profile and body composition impairments such as increased fat mass and reduced muscle mass [5, 6], patients are at an increased risk of both cancer and non-cancer related mortality with 5-year survival rates as low as 30% depending on health status and stage at the time of prostate cancer diagnosis [7].
Obesity is a potential predictor of mortality in men with prostate cancer [8, 9], affecting not only tumour biology [10] but also the outcomes of radical prostatectomy and radiation therapy [8, 11,12,13]. Significant associations between high body mass index (BMI; >30 kg m−2) and a 23% increased risk for all-cause mortality [9], or increases of 5 kg m−2 with a 20% increased risk of prostate cancer-specific mortality [8] were reported in previous investigations. However, the association of obesity with all-cause mortality is not consistent across all prostate cancer studies, with some studies challenging this relationship by presenting no significant association between higher BMI values and overall survival in this population [14, 15], or presenting an inverse relationship between obesity and survival [16]. This apparent obesity paradox may be related to the reliance on BMI since this measure does not differentiate lean from fat mass or visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT) [17, 18], masking the relationship of fat mass with overall survival in men with prostate cancer [19, 20]. Furthermore, sarcopenia or the loss of muscle mass has also been considered an important prognostic factor [6, 21,22,23], although its association with overall survival in men with prostate cancer is largely controversial depending on the cancer stage or phase of treatment [16, 24, 25]. Therefore, it remains to be determined if excess fat mass, reduced levels of muscle mass, or both treatment-related changes in body composition have an impact on overall survival in men with prostate cancer [20]. Determining these associations may potentially inform specific and tailored strategies to improve overall survival in this group of patients.
As a result, we investigated in this systematic review the role of body composition on overall survival in men with prostate cancer, analysing the associations of low muscle mass and high fat mass as prognostic factors. In addition, a range of possible clinical (i.e., localised vs. advanced disease) and methodological (i.e., definition of cut-off values for muscle mass, depots of fat mass and controlling for BMI in multivariable analysis) variables that may affect the associations of body composition with overall survival were examined by subgroup analyses.
Methods
Study selection procedure
A systematic search was conducted in the following electronic databases: CINAHL, Cochrane Library, EMBASE, PubMed and Web of Science from inception to December 2020. The search strategy is presented in the Supplementary eAppendix 1. In addition, we also performed a manual search of the reference lists provided in the selected papers as well as in abstracts from the American Society of Clinical Oncology, Clinical Oncology Society of Australia and the American College of Sports Medicine conferences from 2014 to 2020. All procedures were undertaken in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement [26, 27] and based on the minimum criteria established by the Cochrane Back Review Group [28], with registration at the international prospective register of systematic reviews (PROSPERO identifier: CRD42020218736).
This review included published articles and conference abstracts [29] of studies evaluating the association of body composition measures, such as fat mass (e.g., fat mass, VAT, SAT and VAT/SAT) and muscle mass measures, with overall survival in prostate cancer patients at any treatment stage. The primary and only outcome for this review was overall survival, defined as the time in months of death by any cause. The exclusion criteria were: (1) studies involving mixed cancer patients without specific information on the results for prostate cancer patients; (2) studies not including or reporting on the specific outcomes for this review, or did not include sufficient information such as hazard ratios (HR) and 95% confidence intervals (CI) for overall survival analysis; (3) studies evaluating specific interventions for body composition such as nutrition or exercise; and (4) written in a language other than English. In the search strategy, titles and abstracts were first independently evaluated following the eligibility criteria. When abstracts did not provide sufficient information, they were selected for full-text evaluation. In addition, authors were contacted for further information when necessary. Eligibility was assessed independently in duplicate (PL and FS), with differences resolved by consensus.
Data extraction
Data extraction was performed via a standardised form. Clinical and methodological information were extracted from the included studies such as cancer stage and treatment, number of participants at baseline, geographical region, age and BMI at baseline, fat and muscle mass assessments (i.e., method of assessment, location and cut-off values), follow-up period, HR for overall survival with their associated dispersion values such as 95% CI or standard errors (SE) from univariable and multivariable analyses, when available, and the number of covariates included in the multivariable models.
Study quality assessment
The study quality assessment was evaluated according to the Newcastle-Ottawa Quality Assessment Scale (NOS) for cohort studies [30]. The NOS consists of eight items related to representativeness of the exposed cohort, comparability based on the study design or analysis and assessment of outcome and adequacy of follow-up with a total maximum score of 9 [30]. Studies were assessed by the following items: (1) Representativeness of the exposed cohort; (2) Selection of the non-exposed cohort; (3) Ascertainment of exposure; (4) Demonstration that outcome of interest was not present at start of study; (5) Comparability of cohorts on the basis of the design or analysis; (6) Assessment of outcome; (7) Was follow-up long enough for outcomes to occur; (8) Adequacy of follow up of cohorts. The study quality assessment for all included studies were performed independently by two reviewers (PL and FS) with disagreements resolved by consensus.
Data analysis
Data from the associations of body composition with overall survival such as HR and their associated dispersion values were pooled using inverse variance random-effects models. These values were extracted from univariable and multivariable models and log-transformed to be included in further analyses. Analyses were conducted for studies reporting multivariable or univariable analysis and subgroup analyses were provided for the following: (1) removing outliers; (2) for prostate cancer subgroups (stage or phase of treatment); (3) previously defined or median cut-off values for muscle mass outcomes; (4) specific depots of fat and (5) studies using BMI as a covariate or not in the multivariable models. A p value of ≤0.05 was considered statistically significant. Forest plots were generated to present the results for multivariable and univariable analysis of fat and muscle mass. Heterogeneity between studies was assessed by using the I2 statistic and the p value from χ2-based Cochran’s Q test with a high heterogeneity defined by a threshold p value of 0.1 or I2 value greater than 50% [31]. We examined outliers using sensitivity analysis by omitting one study at a time. To check for publication bias, contour-enhanced funnel plots of log HR against its SE were generated and explored using Egger’s regression asymmetry test when more than ten studies were available [32]. Analyses were conducted using the Review Manager (RevMan) software from the Cochrane Collaboration (version 5.4, Copenhagen: The Nordic Cochrane Centre) and the package ‘meta’ from R (R Core Team, 2020).
Results
Studies included and characteristics
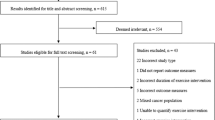
Of the 805 retrieved studies, 514 potential records were retained for screening after duplicate removals. Of these, 373 were excluded due to their irrelevance to the research question and 141 articles were deemed eligible and undertaken for review (Fig. 1 and Supplementary eAppendix 2). A total of 16 cohort studies undertaking retrospective analyses [16, 24, 25, 33,34,35,36,37,38,39,40,41,42,43,44,45] were included in the primary analysis. During the eligibility assessment, six additional studies [46,47,48,49,50,51] were initially selected and authors contacted given the lack of specific information on the results for prostate cancer patients. Responses were not obtained and, as a result, these studies were not included in our review.
The characteristics of the individual studies are presented in Tables 1 and 2. In summary, a total of 4807 prostate cancer patients with a median age of 69.0 years (interquartile range (IQR): 67.2–71.3) and BMI of 26.6 kg m−2 (IQR: 24.3–28.7) participated in the included studies. All studies except one derived fat and muscle mass measures from CT scans [16, 24, 25, 34,35,36,37,38,39,40,41,42,43,44,45]. Most studies (n = 11) included advanced prostate cancer patients (e.g., metastatic, castration-resistant or metastatic castration-resistant patients) [16, 24, 34, 35, 38, 39, 41,42,43,44,45], and the majority of patients received treatments such as radiotherapy [33, 36,37,38,39,40,41,42,43] and ADT [33, 35,36,37, 40,41,42,43,44] (n = 9 for both), followed by surgery [25, 33, 36, 37, 39, 42, 43] and chemotherapy [34, 35, 39, 41,42,43, 45] (n = 7 for both), and novel hormonal agents such as abiraterone and enzalutamide (n = 1) [24]. Regarding the quality assessment, the median overall score was seven out of nine ranging from 4 to 9 pts. The quality assessment of individual studies is presented in eTable 1 (Supplementary material).
Fat mass and overall survival
Eight studies [24, 33,34,35, 40, 43,44,45] comparing high vs. low levels of fat mass on overall survival were included in the analysis, with six studies examining VAT (cut-off values reported: 52.2 cm2 m−2 [23], 58.7 cm2 m−2 [35], 59.4 cm2 m−2 [43], 68.0 cm2 m−2 [45], 100.0 cm2 [44] and 287.3 cm2 [40]) [24, 35, 40, 43,44,45], five studies examining SAT (cut-off values reported: 48.2 cm2 m−2 [43], 51.7 cm2 m−2 [24], 55.3 cm2 m−2 [35], 64.1 cm2 m−2 [45] and 36.4 cm2 [40]) [24, 35, 40, 43, 45], three studies examining VAT/SAT ratio (with one study reporting a cut-off of 1.0 [44]) [34, 44, 45] and one study examining whole-body fat mass [33]. Given that six studies [24, 34, 35, 40, 43, 45] undertook multivariable models controlling for BMI (median number of covariates of 7.0, ranging from 2 to 12; with two studies also controlling for muscle mass measures [24, 43]), the results from the meta-analysis provided no differences in overall survival (HR 0.98, p = 0.888; Table 3) in a sample of 1697 prostate cancer patients. The heterogeneity was I2 = 70%. Patients presenting with high levels of SAT are at an advantage for overall survival compared to those presenting with low SAT levels (HR 0.68, 95% CI: 0.54–0.84; Fig. 2A), while analysis for VAT/SAT ratio provided a 50% greater mortality risk (HR 1.50, 95% CI: 1.15–1.97; Fig. 2A) to patients presenting high levels compared to those presenting with low levels. No difference was observed regarding VAT (p = 0.873; Fig. 2A), between results derived VAT and VAT/SAT (χ2 = 3.1; p = 0.080), while VAT and SAT (χ2 = 4.0; p = 0.045) and SAT and VAT/SAT (χ2 = 19.5; p < 0.001) were significantly different (Table 3). Differences were also not observed between patients with localised and advanced disease (χ2 = 1.2; p = 0.275) or for studies controlling for BMI (χ2 = 1.2; p = 0.273). In the univariable analysis, a 23% survival advantage was found after removing the study of Stangl-Kremser et al. [45] considered an outlier for the overall effect (HR 0.77, 95% CI: 0.64–0.92; Table 3), while the direction of the results was maintained for all subgroup analyses (p = 0.061–0.438; Table 2 and Fig. 2B) without differences between covariates. No publication bias was found (p = 0.146; Supplementary eFig. 1A).
Association of low and high levels of VAT, SAT and VAT/SAT ratio (A, B) and muscle mass (C, D) with overall survival in men with prostate cancer. Analyses derived from multivariable and univariate models were presented in A, C and B, D, respectively. Higher VAT/SAT ratio indicates poorer overall survival. Overall effects analyses conducted with inverse variance random-effects meta-analysis. Squares represent study-specific estimates; diamonds represent pooled hazard ratios estimates of random-effects meta-analysis. *Study-specific estimate based on median values derived from skeletal muscle mass index and skeletal muscle volume indexes; FM fat mass, SAT subcutaneous adipose tissue, VAT visceral adipose tissue.
Muscle mass and overall survival
Thirteen studies [16, 24, 25, 33, 35,36,37,38,39, 41,42,43, 45] comparing low vs. high levels of muscle mass on overall survival were included in the analysis, with eight studies examining skeletal muscle mass index (cut-off values reported: 43.0 or 53.0 cm2 m−2 [16, 35, 41, 45], 45.0 cm2 m−2 [24], 45.2 cm2 m−2 [22], 49.9 cm2 m−2 [43] and 55.0 cm2 m−2 [37]) [16, 24, 35, 37, 41,42,43, 45], three studies examining psoas muscle index (cut-off values reported: 4.7 cm2 m−2 [25], 5.7 cm2 m−2 [39] and 7.5 cm2 m−2 [36]) [25, 36, 39], one study examining average psoas muscle size [38] or skeletal muscle volume index (cut-off value reported: 28.7 kg [45]). Meta-analysis involving data derived from multivariable models (median number of covariates of 5, ranging from 1 to 12; with two studies also controlling for fat mass measures [24, 43]) resulted in 50% greater mortality risk (HR 1.50, 95% CI: 1.11–2.05; Table 4 and Fig. 2C) for patients presenting with low levels of muscle mass compared to those presenting with high levels in a sample of 3275 men with prostate cancer. The study of Xu et al. [16] was considered an outlier in the analysis. After adjustment, the meta-analysis resulted in a HR of 1.63 (95% CI: 1.27–2.08; Table 3) with a heterogeneity I2 = 58%. The results were maintained in the subgroup analyses (HR 1.43–1.91, p = <0.001–0.036) except for studies controlling for BMI, which approached statistical significance (HR 1.48, 95% CI: 0.98–2.26, p = 0.060). Similarly, results were similar in univariable model analyses (HR 1.31–1.40; p = 0.002–0.004; Table 4 and Fig. 2D) except for those using previously defined cut-off values (p = 0.271; Table 3). No differences were observed between covariates in either multivariable or univariable models (p = 0.184–0.974). No publication bias was found (p = 0.301; Supplementary eFig. 1B).
Discussion
In this review we examined the role of fat and muscle mass on survival in men with prostate cancer. The main findings of our study were: (1) although overall fat mass was not a prognostic factor in men with prostate cancer, high levels of subcutaneous fat and low levels of VAT/SAT were associated with a 32% and 50% survival advantage, respectively, in patients at advanced stages of the disease; and (2) patients presenting with low muscle mass levels are at ~50% increased risk of mortality compared to those presenting with high levels regardless of the cancer stage or methodological characteristics. These results are clinically relevant and indicate the importance of muscle mass in particular during the course of therapy given the substantial impact on overall survival of patients with prostate cancer.
Although obesity and the resulting metabolic environment are deemed important factors for biochemical recurrence, metastatic disease and mortality in men with prostate cancer [8, 9], our finding is that total adiposity is not associated with overall survival in prostate cancer patients. Interestingly, the reasons for this particular outcome may be related to the metabolic differences between SAT and VAT [52], with subcutaneous and visceral depots of fat exerting conflicting effects on overall survival in prostate cancer patients. For example, researchers have suggested that VAT is closely associated with inflammatory cytokines (e.g., interleukin-6 and tumour necrosis factor-alpha) which may potentially affect the tumour microenvironment [10, 52], while subcutaneous tissue-derived factors such as leptin may act in contrast by increasing insulin sensitivity and lipid metabolism, thereby, effectively improving survival [52,53,54,55]. Another potential explanation for the different findings reported previously [8, 9] and this study may be related to cancer cachexia [19]. This phenomenon may mislead the association of obesity with cancer progression or mortality given the unintentional weight loss that can occur during cancer treatment or even before the cancer detection (i.e., reverse causation) in obese cancer patients [19]. Thus, the assessment of BMI alone at the time of cancer may not inform whether prostate cancer patients have been obese before diagnostic, precluding us to specifically observe the influence of obesity on cancer survival in prostate cancer patients. Finally, our data on fat mass and overall survival were derived from studies mostly with advanced prostate cancer patients (i.e., metastatic and castration-resistant patients) and this may explain the difference between our findings and a previous study indicating significant associations between BMI and weight gain with prostate cancer outcomes in nonmetastatic patients [9]. Our results are in line with previous studies concerning the prognostic value of different depots of fat mass in cancer patients [24, 52, 56] and may indicate the necessity to cautiously interpret total adiposity in this group of patients, as different levels of obesity and depots of fat are influencing overall survival in opposite ways [57]. Therefore, the utilisation of the VAT/SAT ratio may be a good strategy to avoid such conflicting effects derived from different depots of fat. For example, in a previous study [34] high levels of VAT/SAT ratio were significantly associated with shorter survival in normal weight prostate cancer patients, although this relationship was not observed in overweight or obese patients. Consequently, more research is required to elucidate the physiological value of VAT/SAT ratio on overall survival. Moreover, although high levels of VAT did not significantly increase the risk of mortality in our analysis, previous studies have indicated the association with radical prostatectomy and radiation therapy outcomes [40, 58] increasing surgical and recurrence risks, respectively, as well as increased risk of cardiovascular and metabolic disease [59]. Thus, more studies are necessary to elucidate the indirect or direct role of VAT on overall survival in men with prostate cancer.
Contrary to the results regarding total adiposity, a high level of muscle mass was associated with improved overall survival in prostate cancer patients regardless of treatment stage or methodological characteristics. This may be related to the numerous benefits of muscle mass on metabolic health such as regulating and mobilising natural killer cells into the tumour, or even altering other biomarkers associated with the tumour biology [60, 61]. In addition, crosstalk between muscle and other organs has also emerged as a potential mechanism by which the musculoskeletal system supresses cancer growth and therefore increases overall survival in men with prostate cancer [60, 61]. Moreover, the present findings on muscle mass are in accordance with several other studies indicating a relationship between sarcopenia and survival in cancer patients [21,22,23] suggesting the importance of improving or maintaining muscle mass in this population before and during treatment [62]. For example, several trials have demonstrated the benefits of exercise, specifically resistance-based exercise programmes (i.e., anabolic exercise) increasing muscle mass during and following ADT [63,64,65,66], as well as preserving muscle mass in high-grade patients [67]. Therefore, the findings from our review are clinically meaningful indicating that muscle mass is an important prognostic factor for men with prostate cancer regardless of cancer stage. Also, accrual or maintenance of muscle mass through prescribed and tailored exercise, specifically resistance-based exercise, undertaken before, during and following cancer treatment would be beneficial in this population to effectively increase the chances of overall survival.
The strengths of the present study are: (1) a relatively large number of studies (n = 16) with up to 4807 prostate cancer patients included; (2) the assessment of both univariable and multivariable models; and (3) subgroup analyses based on different clinical and methodological characteristics. However, there are also some limitations which are worthy of comment. First, only cohort studies undertaking retrospective analyses were included in our review and this precludes determining causality of body composition changes such as increase in muscle mass and reduction in fat mass on overall survival. Future prospective analyses are necessary to improve current knowledge by indicating if interventions targeting fat and muscle mass are able to improve overall and disease-specific survival as well as recurrence in men with prostate cancer. In addition, researchers used different definitions for sarcopenia such as the skeletal muscle index, psoas muscle or median values, while no definition for adiposity measures was used, leading to high heterogeneity within the models. Sarcopenia has become a topic of great interest in oncology [68]; however, poorly understood given the lack of reporting on assessment characteristics and definitions. For example, although studies had reported the time of body composition assessment [25, 33, 34, 36, 37, 40,41,42,43, 45], the high heterogeneity and lack of standardisation could misclassify prostate cancer patients with obesity or sarcopenia and, therefore, mask the impact of these outcomes on overall survival. Future research should better inform definitions (i.e., cut-off values and rationale) and time of assessments, and information about clinical factors associated with muscle mass accrual or maintenance in this group of patients. This will improve the assessment of sarcopenia as well as provide information about its interaction with obesity on overall survival in this group of patients and assist future systematic reviews and meta-analyses. Nonetheless, subgroup analysis was undertaken based on previously defined methods to identify sarcopenia vs. median values to minimise such bias, with the results largely maintained, although the same was not conducted for fat mass given the lack of previous definitions. Finally, data concerning the association of fat mass and muscle mass measures with prostate cancer-specific and cardiovascular mortality as well as specific information about deaths are limited. Therefore, it is not possible to account for deaths directly or indirectly related to prostate cancer treatment comorbidities (e.g., metabolic syndrome, diabetes, cardiovascular disease).
As far as we are aware, the present systematic review and meta-analysis is the first to examine the prognostic value of fat and muscle mass in men with prostate cancer. In summary, increased levels of muscle mass and SAT and reduced VAT/SAT ratio rather than overall adiposity are important prognostic factors in men with prostate cancer, even when controlling for multiple confounding factors. Furthermore, we provide rationale for future prospective analyses investigating the impact of sarcopenia and changes in muscle mass during cancer treatment on prostate cancer outcomes, as well as the investigation of strategies such as exercise and nutritional interventions to improve survival in this population.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30.
D’Amico AV, Chen MH, Renshaw AA, Loffredo M, Kantoff PW. Androgen suppression and radiation vs radiation alone for prostate cancer: a randomized trial. JAMA. 2008;299:289–95.
Prencipe M, Madden SF, O’Neill A, O’Hurley G, Culhane A, O’Connor D, et al. Identification of transcription factors associated with castration-resistance: is the serum responsive factor a potential therapeutic target? Prostate. 2013;73:743–53.
Lin T-T, Chen Y-H, Wu Y-P, Chen S-Z, Li X-D, Lin Y-Z, et al. Risk factors for progression to castration-resistant prostate cancer in metastatic prostate cancer patients. J Cancer. 2019;10:5608–13.
Galvao DA, Spry NA, Taaffe DR, Newton RU, Stanley J, Shannon T, et al. Changes in muscle, fat and bone mass after 36 weeks of maximal androgen blockade for prostate cancer. BJU Int. 2008;102:44–7.
Smith MR, Saad F, Egerdie B, Sieber PR, Tammela TL, Ke C, et al. Sarcopenia during androgen-deprivation therapy for prostate cancer. J Clin Oncol. 2012;30:3271–6.
Kirby M, Hirst C, Crawford ED. Characterising the castration-resistant prostate cancer population: a systematic review. Int J Clin Pract. 2011;65:1180–92.
Cao Y, Ma J. Body mass index, prostate cancer-specific mortality, and biochemical recurrence: a systematic review and meta-analysis. Cancer Prev Res (Philos). 2011;4:486–501.
Troeschel AN, Hartman TJ, Jacobs EJ, Stevens VL, Gansler T, Flanders WD, et al. Postdiagnosis body mass index, weight change, and mortality from prostate cancer, cardiovascular disease, and all causes among survivors of nonmetastatic prostate cancer. J Clin Oncol. 2020;38:2018–27.
Deng T, Lyon CJ, Bergin S, Caligiuri MA, Hsueh WA. Obesity, inflammation, and cancer. Annu Rev Pathol. 2016;11:421–49.
Wiltz AL, Shikanov S, Eggener SE, Katz MH, Thong AE, Steinberg GD, et al. Robotic radical prostatectomy in overweight and obese patients: oncological and validated-functional outcomes. Urology. 2009;73:316–22.
Freedland SJ, Grubb KA, Yiu SK, Nielsen ME, Mangold LA, Isaacs WB, et al. Obesity and capsular incision at the time of open retropubic radical prostatectomy. J Urol. 2005;174:1798–801.
Mikhail AA, Stockton BR, Orvieto MA, Chien GW, Gong EM, Zorn KC, et al. Robotic-assisted laparoscopic prostatectomy in overweight and obese patients. Urology. 2006;67:774–9.
Farris MS, Courneya KS, Kopciuk KA, McGregor SE, Friedenreich CM. Anthropometric measurements and survival after a prostate cancer diagnosis. Br J Cancer. 2018;118:607–10.
Zhong S, Yan X, Wu Y, Zhang X, Chen L, Tang J, et al. Body mass index and mortality in prostate cancer patients: a dose-response meta-analysis. Prostate Cancer Prostatic Dis. 2016;19:122–31.
Xu MC, Huelster HL, Hatcher JB, Avulova S, Stocks BT, Glaser ZA, et al. Obesity is associated with longer survival independent of sarcopenia and myosteatosis in metastatic and/or castrate-resistant prostate cancer. J Urol. 2021;205:800–5.
Brown JC, Cespedes Feliciano EM, Caan BJ. The evolution of body composition in oncology-epidemiology, clinical trials, and the future of patient care: facts and numbers. J Cachexia Sarcopenia Muscle. 2018;9:1200–8.
Flegal KM, Shepherd JA, Looker AC, Graubard BI, Borrud LG, Ogden CL, et al. Comparisons of percentage body fat, body mass index, waist circumference, and waist-stature ratio in adults. Am J Clin Nutr. 2009;89:500–8.
Lee DH, Giovannucci EL. The obesity paradox in cancer: epidemiologic insights and perspectives. Curr Nutr Rep. 2019;8:175–81.
Marshall CH, Joshu CE. Mounting weight of evidence on the importance of body weight for men with prostate cancer. J Clin Oncol. 2020;38:2007–9.
Ubachs J, Ziemons J, Minis-Rutten IJG, Kruitwagen R, Kleijnen J, Lambrechts S, et al. Sarcopenia and ovarian cancer survival: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2019;10:1165–74.
Lee CM, Kang J. Prognostic impact of myosteatosis in patients with colorectal cancer: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2020;11:1270–82.
Antoniou GA, Rojoa D, Antoniou SA, Alfahad A, Torella F, Juszczak MT. Effect of low skeletal muscle mass on post-operative survival of patients with abdominal aortic aneurysm: a prognostic factor review and meta-analysis of time-to-event data. Eur J Vasc Endovasc Surg. 2019;58:190–8.
Antoun S, Bayar A, Ileana E, Laplanche A, Fizazi K, Di Palma M, et al. High subcutaneous adipose tissue predicts the prognosis in metastatic castration-resistant prostate cancer patients in post chemotherapy setting. Eur J Cancer. 2015;51:2570–7.
Pak S, Park SY, Shin TJ, You D, Jeong IG, Hong JH, et al. Association of muscle mass with survival after radical prostatectomy in patients with prostate cancer. J Urol. 2019;202:525–32.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann T, Mulrow CD, et al. Mapping of reporting guidance for systematic reviews and meta-analyses generated a comprehensive item bank for future reporting guidelines. J Clin Epidemiol. 2020;118:60–8.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Open Med. 2009;3:e123–30.
Furlan AD, Pennick V, Bombardier C, van Tulder M,Editorial Board CBRG. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Philos Pa 1976). 2009;34:1929–41.
Scherer RW, Saldanha IJ. How should systematic reviewers handle conference abstracts? A view from the trenches. Syst Rev. 2019;8:264.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. Newcastle-Ottawa quality assessment scale cohort studies. University of Ottawa. 2014. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp2014.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol. 2008;61:991–6.
Buttigliero C, Vana F, Bertaglia V, Vignani F, Fiori C, Osella G, et al. The fat body mass increase after adjuvant androgen deprivation therapy is predictive of prostate cancer outcome. Endocrine. 2015;50:223–30.
Wu W, Liu X, Chaftari P, Cruz Carreras MT, Gonzalez C, Viets-Upchurch J, et al. Association of body composition with outcome of docetaxel chemotherapy in metastatic prostate cancer: a retrospective review. PLoS ONE. 2015;10:e0122047.
Cushen SJ, Power DG, Murphy KP, McDermott R, Griffin BT, Lim M, et al. Impact of body composition parameters on clinical outcomes in patients with metastatic castrate-resistant prostate cancer treated with docetaxel. Clin Nutr Espen. 2016;13:e39–45.
McDonald AM, Swain TA, Mayhew DL, Cardan RA, Bakder CB, Harris DM, et al. (S010) Computed tomography–assessed measures of bone mineral density and muscle mass as predictors of survival in men with prostate cancer. Oncology (08909091). 2016 Supplement A Century of Caring, p5-5. 1/2p.
Mason RJ, Boorjian SA, Bhindi B, Rangel L, Frank I, Karnes RJ, et al. The association between sarcopenia and oncologic outcomes after radical prostatectomy. Clin Genitourin Cancer. 2018;16:e629–36.
Zakaria HM, Massie L, Basheer A, Elibe E, Boyce-Fappiano D, Shultz L, et al. Application of morphometrics as a predictor for survival in patients with prostate cancer metastasis to the spine. World Neurosurg. 2018;114:e913–9.
Ohtaka A, Aoki H, Nagata M, Kanayama M, Shimizu F, Ide H, et al. Sarcopenia is a poor prognostic factor of castration-resistant prostate cancer treated with docetaxel therapy. Prostate Int. 2019;7:9–14.
Di Bella CM, Howard LE, Oyekunle T, De Hoedt AM, Salama JK, Song H, et al. Abdominal and pelvic adipose tissue distribution and risk of prostate cancer recurrence after radiation therapy. Prostate. 2020;80:1244–52.
Ikeda T, Ishihara H, Iizuka J, Hashimoto Y, Yoshida K, Kakuta Y, et al. Prognostic impact of sarcopenia in patients with metastatic hormone-sensitive prostate cancer. Jpn J Clin Oncol. 2020;50:933–9.
Lee J, Park JS, Heo JE, Ahn HK, Jang WS, Ham WS, et al. Muscle characteristics obtained using computed tomography as prognosticators in patients with castration-resistant prostate cancer. Cancers. 2020;12:1864.
Pak S, Kim MS, Park EY, Kim SH, Lee KH, Joung JY. Association of body composition with survival and treatment efficacy in castration-resistant prostate cancer. Front Oncol. 2020;10:558.
Sasaki T, Sugino Y, Kato M, Nishikawa K, Kanda H. Pre-treatment ratio of periprostatic to subcutaneous fat thickness on MRI is an independent survival predictor in hormone-naive men with advanced prostate cancer. Int J Clin Oncol. 2020;25:370–6.
Stangl-Kremser J, Suarez-Ibarrola R, Andrea D, Korn SM, Pones M, Kramer G, et al. Assessment of body composition in the advanced stage of castration-resistant prostate cancer: special focus on sarcopenia. Prostate Cancer Prostatic Dis. 2020;23:309–15.
Mukherji D, Pezaro CJ, Bianchini D, Tunariu N, Cassidy MA, Omlin AG, et al. Sarcopenia and altered body composition following abiraterone acetate (AA) and corticosteroid (C) treatment in men with castration-refractory prostate cancer (CRPC). J Clin Oncol Am Soc Clin Oncol. 2012;30(15_suppl):e15134–e15134.
Blauwhoff-Buskermolen S, Langius JAE, Becker A, Verheul HMW, de van der Schueren MAE. The influence of different muscle mass measurements on the diagnosis of cancer cachexia. J Cachexia Sarcopenia Muscle. 2017;8:615–22.
Versteeg KS, Blauwhoff-Buskermolen S, Buffart LM, de van der Schueren MAE, Langius JAE, Verheul HMW, et al. Higher muscle strength is associated with prolonged survival in older patients with advanced cancer. Oncologist. 2018;23:580–5.
Delouya G, Tiberi D, Bhatnagar SR, Campeau S, Saad F, Taussky D. Impact of adipose tissue on prostate cancer aggressiveness—analysis of a high-risk population. Horm Mol Biol Clin Investig. 2018;36:1–6.
Pennington Z, Pielkenrood B, Ahmed AK, Goodwin CR, Verlaan JJ, Sciubba DM. Visceral fat volume from standard preoperative ct is an independent predictor of short-term survival in patients undergoing surgery for metastatic spine disease. Clin Spine Surg. 2019;32:E303–10.
Zakaria HM, Llaniguez JT, Telemi E, Chuang M, Abouelleil M, Wilkinson B, et al. Sarcopenia predicts overall survival in patients with lung, breast, prostate, or myeloma spine metastases undergoing stereotactic body radiation therapy (SBRT), independent of histology. Neurosurgery. 2020;86:705–16.
Ebadi M, Martin L, Ghosh S, Field CJ, Lehner R, Baracos VE, et al. Subcutaneous adiposity is an independent predictor of mortality in cancer patients. Br J Cancer. 2017;117:148–55.
Ebadi M, Baracos VE, Bathe OF, Robinson LE, Mazurak VC. Loss of visceral adipose tissue precedes subcutaneous adipose tissue and associates with n-6 fatty acid content. Clin Nutr. 2016;35:1347–53.
Porter SA, Massaro JM, Hoffmann U, Vasan RS, O’Donnel CJ, Fox CS. Abdominal subcutaneous adipose tissue: a protective fat depot? Diabetes Care. 2009;32:1068–75.
Ogino S, Shima K, Baba Y, Nosho K, Irahara N, Kure S, et al. Colorectal cancer expression of peroxisome proliferator-activated receptor gamma (PPARG, PPARgamma) is associated with good prognosis. Gastroenterology. 2009;136:1242–50.
Lee JS, Lee HS, Ha JS, Han KS, Rha KH, Hong SJ, et al. Subcutaneous fat distribution is a prognostic biomarker for men with castration resistant prostate cancer. J Urol. 2018;200:114–20.
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309:71–82.
Uchida T, Higure T, Kawakami M, Nakano M, Nakajima N, Kim H, et al. What factors affect the operative time of robot-assisted laparoscopic radical prostatectomy? Surg Endosc. 2020;35:4436–43.
Karlsson T, Rask-Andersen M, Pan G, Höglund J, Wadelius C, Ek WE, et al. Contribution of genetics to visceral adiposity and its relation to cardiovascular and metabolic disease. Nat Med. 2019;25:1390–5.
Severinsen MCK, Pedersen BK. Muscle-organ crosstalk: the emerging roles of myokines. Endocr Rev. 2020;41:594–609.
Pedersen BK, Febbraio MA. Muscles, exercise and obesity: skeletal muscle as a secretory organ. Nat Rev Endocrinol. 2012;8:457–65.
Sartori R, Romanello V, Sandri M. Mechanisms of muscle atrophy and hypertrophy: implications in health and disease. Nat Commun. 2021;12:330.
Lopez P, Taaffe DR, Newton RU, Galvao DA. Resistance exercise dosage in men with prostate cancer: systematic review, meta-analysis, and meta-regression. Med Sci Sports Exerc. 2021;53:459–69.
Newton RU, Galvao DA, Spry N, Joseph D, Chambers SK, Gardiner RA, et al. Exercise mode specificity for preserving spine and hip bone mineral density in prostate cancer patients. Med Sci Sports Exerc. 2019;51:607–14.
Taaffe DR, Galvao DA, Spry N, Joseph D, Chambers SK, Gardiner RA, et al. Immediate versus delayed exercise in men initiating androgen deprivation: effects on bone density and soft tissue composition. BJU Int. 2019;123:261–9.
Galvao DA, Taaffe DR, Spry N, Joseph D, Newton RU. Combined resistance and aerobic exercise program reverses muscle loss in men undergoing androgen suppression therapy for prostate cancer without bone metastases: a randomized controlled trial. J Clin Oncol. 2010;28:340–7.
Galvao DA, Taaffe DR, Spry N, Cormie P, Joseph D, Chambers SK, et al. Exercise preserves physical function in prostate cancer patients with bone metastases. Med Sci Sports Exerc. 2018;50:393–9.
Williams GR, Dunne RF, Giri S, Shachar SS, Caan BJ. Sarcopenia in the Older Adult With Cancer. J Clin Oncol. 2021;39:2068–78.
Acknowledgements
PL is supported by the National Health and Medical Research Council (NHMRC) Centre of Research Excellence (CRE) in Prostate Cancer Survivorship Scholarship. DAG and RUN are funded by a NHMRC CRE in Prostate Cancer Survivorship. The results of the study are presented clearly, honestly, without fabrication, falsification or inappropriate data manipulation.
Author information
Authors and Affiliations
Contributions
PL had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis; Conception and design: PL, RUN, DRT and DAG; Acquisition, analysis, or interpretation of data: PL, RUN, DRT, Favil S and DAG; Drafting of the manuscript: PL, RUN, DRT, Favil S, LMB, NS, CT, Fred S and DAG; Critical revision of the manuscript for important intellectual content: PL, RUN, DRT, Favil S, LMB, NS, CT, Fred S and DAG; Statistical analysis: PL.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lopez, P., Newton, R.U., Taaffe, D.R. et al. Associations of fat and muscle mass with overall survival in men with prostate cancer: a systematic review with meta-analysis. Prostate Cancer Prostatic Dis 25, 615–626 (2022). https://doi.org/10.1038/s41391-021-00442-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-021-00442-0
This article is cited by
-
Association between muscle mass and overall survival among colorectal cancer patients at tertiary cancer center in the Middle East
Scientific Reports (2024)
-
Psoas mass index at the level of the third lumbar vertebra on computed tomography is a prognostic predictor for metastatic castration-sensitive prostate cancer
International Journal of Clinical Oncology (2024)
-
A qualitative analysis of nutritional needs and dietary changes during cancer treatment in Ireland
Irish Journal of Medical Science (1971 -) (2024)
-
Prognostic value of a baseline prognostic nutritional index for patients with prostate cancer: a systematic review and meta-analysis
Prostate Cancer and Prostatic Diseases (2023)
-
Elastic tubes: the ideal equipment for telehealth exercise medicine in the management of prostate cancer?
Supportive Care in Cancer (2022)