Abstract
Purpose
To assess the prevalence of sarcopenia and whether body composition parameters are associated with disease progression and overall survival (OS) in castration-resistant prostate cancer (CRPC) patients.
Materials and methods
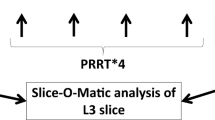
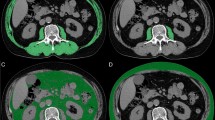
This single-centre retrospective study evaluated data of 186 consecutive patients who underwent chemohormonal therapy between 2005 and 2016 as first-line systemic treatment for CRPC. Skeletal muscle and fat indices were determined using computerized tomography data before initiation of chemotherapy. Sarcopenia was defined as SMI of <55 cm2/m2. Visceral-to-subcutaneous fat ratio and skeletal muscle volume were calculated with body composition specific areas. Harrell’s concordance index was used for predictive accuracy.
Results
A total of 154 (82.8%) patients met the criteria for sarcopenia; 139 (74.7%) individuals completed at least six cycles of docetaxel. Within a median follow-up of 24.1 months, age (HR 1.03, 95% CI 1.01–1.06, p = 0.02), high PSA (1.55, 95% CI 1.07–2.25, p = 0.02) and low skeletal muscle volume (HR 1.61, 95% CI 1.10–2.35, p = 0.02) were the only independent prognostic factor for tumor progression. Overall, 93 (50%) patients died during the follow-up period. The established prognosticator, the prechemotherapy presence of liver metastases (HR 1.32, 95% CI 1.08–1.61, p < 0.01) was associated with shorter OS. Moreover, we noted that patients with an elevated visceral-to-subcutaneous fat ratio tended to have a shorter OS (p = 0.06).
Conclusion
The large majority of men with CRPC suffers from sarcopenia. In our cohort, low skeletal muscle volume was an independent adverse prognosticator for progression of disease. We could not detect a statistically significant body composition parameter for OS, although patients with a high proportion of visceral fat had a trend for shorter OS. However, we suggest that body composition parameters determined by CT data can provide useful objective prognostic factors that may support tailored treatment decision-making.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34.
American Cancer Society’s (ACS). Cancer facts and figures 2018. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2018.html. Accessed on 20.08.2019.
Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M, et al. EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol. 2017;71:618–29.
Saylor PJ, Smith MR. Metabolic complications of androgen deprivation therapy for prostate cancer. J Urol. 2013;189:S34–42.
Smith MR, Saad F, Egerdie B, Sieber PR, Tammela TL, Ke C, et al. Sarcopenia during androgen-deprivation therapy for prostate cancer. J Clin Oncol. 2012;30:3271–6.
Hamilton EJ, Gianatti E, Strauss BJ, Wentworth J, Lim-Joon D, Bolton D, et al. Increase in visceral and subcutaneous abdominal fat in men with prostate cancer treated with androgen deprivation therapy. Clin Endocrinol. 2011;74:377–83.
Sharifi N, Dahut WL, Steinberg SM, Figg WD, Tarassoff C, Arlen P, et al. A retrospective study of the time to clinical endpoints for advanced prostate cancer. BJU Int. 2005;96:985–9.
Cushen SJ, Power DG, Murphy KP, McDermott R, Griffin BT, Lim M, et al. Impact of body composition parameters on clinical outcomes in patients with metastatic castrate-resistant prostate cancer treated with docetaxel. Clin Nutr ESPEN. 2016;13:e39–e45.
Antoun S, Bayar A, Ileana E, Laplanche A, Fizazi K, di Palma M, et al. High subcutaneous adipose tissue predicts the prognosis in metastatic castration-resistant prostate cancer patients in post chemotherapy setting. Eur J Cancer. 2015;51:2570–7.
Halabi S, Ou SS, Vogelzang NJ, Small EJ. Inverse correlation between body mass index and clinical outcomes in men with advanced castration–recurrent prostate. Cancer Cancer. 2007;110:1478–84.
Vidal AC, Howard LE, de Hoedt A, Kane CJ, Terris MK, Aronson WJ, et al. Obese patients with castration-resistant prostate cancer may be at a lower risk of all-cause mortality: results from the Shared Equal Access Regional Cancer Hospital (SEARCH) database. BJU Int 2018;122:76–82.
Wu W, Liu X, Chaftari P, Cruz Carreras MT, Gonzalez C, Viets-Upchurch J, et al. Association of body composition with outcome of docetaxel chemotherapy in metastatic prostate cancer: a retrospective review. PLoS One. 2015;10:e0122047.
Lee JS, Lee HS, Ha JS, Han KS, Rha KH, Hong SJ, et al. Subcutaneous fat distribution is a prognostic biomarker for men with castration resistant prostate cancer. J Urol. 2018;200:114–20.
Baracos VE, Arribas L. Sarcopenic obesity: hidden muscle wasting and its impact for survival and complications of cancer therapy. Ann Oncol. 2018;29:ii1–ii9.
Ohtaka A, Aoki H, Nagata M, Kanayamaa M, Shimizu F, Ide H, et al. Sarcopenia is a poor prognostic factor of castration-resistant prostate cancer treated with docetaxel therapy. Prostate Int. 2019;7:9–14.
Shariat SF, Semjonow A, Lilja H, Savage C, Vickers AJ, Bjartell A. Tumor markers in prostate cancer I: blood-based markers. Acta Oncol Stock Swed. 2011;50:61–75.
Mourtzakis M, Prado CM, Lieffers JR, Reiman T, McCargar LJ, Baracos VE. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab. 2008;33:997–1006.
Fearon K, Strasser F, Anker SD. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12:489–95.
Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar LJ, et al. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol. 2013;31:1539–47.
Shen W, Punyanitya M, Wang Z, Gallagher D, St-Onge MP, Albu J, et al. Total body skeletal muscle and adipose tissue volumes: estimation from a single abdominal cross-sectional image. J Appl Physiol. 2004;97:2333–8.
Scher HI, Halabi S, Tannock I, Morris M, Sternberg CN, Carducci MA, et al. Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol J Am Soc Clin Oncol. 2008;26:1148–59.
Halabi S, Kelly WK, Ma H, Zhou H, Solomon NC, Fizazi K, et al. Meta-analysis evaluating the impact of site of metastasis on overall survival in men with castration-resistant prostate cancer. J Clin Oncol J Am Soc Clin Oncol. 2016;34:1652–9.
Foulkes SJ, Daly RM, Fraser SF. The clinical importance of quantifying body fat distribution during androgen deprivation therapy for prostate cancer. Endocr Relat Cancer. 2017;24:R35–R48.
Mitsuzuka K, Arai Y. Metabolic changes in patients with prostate cancer during androgen deprivation therapy. Int J Urol. 2018;25:45–53.
Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar LJ, et al. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol J Am Soc Clin Oncol. 2013;31:1539–47.
Acknowledgements
We would like to thank G. Poglitsch for assistance with the collection of the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SFS: advisory board of and/or speaker for Astellas, Astra Zeneca, Bayer, BMS, Cepheid, Ferring, Ipsen, Jansen, Lissy, MSD, Olympus, Pfizer, Pierre Fabre, Roche, Sanochemia, Sanofi, and Wolff. GK: advisory board of and/or speaker for Astellas, Bayer AG, BMS, Ipsen, Janssen, MSD, Roche, Takeda, and Sanofi. All other authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Stangl-Kremser, J., Suarez‐Ibarrola, R., Andrea, D.D. et al. Assessment of body composition in the advanced stage of castration-resistant prostate cancer: special focus on sarcopenia. Prostate Cancer Prostatic Dis 23, 309–315 (2020). https://doi.org/10.1038/s41391-019-0186-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-019-0186-6
This article is cited by
-
Creatine supplementation and resistance training to preserve muscle mass and attenuate cancer progression (CREATINE-52): a protocol for a double-blind randomized controlled trial
BMC Cancer (2024)
-
Associations of fat and muscle mass with overall survival in men with prostate cancer: a systematic review with meta-analysis
Prostate Cancer and Prostatic Diseases (2022)
-
Adiposity and cancer survival: a systematic review and meta-analysis
Cancer Causes & Control (2022)
-
Opportunistic skeletal muscle metrics as prognostic tools in metastatic castration-resistant prostate cancer patients candidates to receive Radium-223
Annals of Nuclear Medicine (2022)