Abstract
Background
Docetaxel is widely used in metastatic castration-resistant prostate cancer (mCRPC), however its optimal use remains unclear in the current treatment landscape. Biomarkers to predict Docetaxel toxicity may help optimize treatment selection. We aimed to create a predictive model for toxicity-related Docetaxel discontinuation (TRDD).
Methods
Through Project Data Sphere, we accessed individual patient data from the control arms of three frontline mCRPC trials: ASCENT2, VENICE, and MAINSAIL. The inclusion criteria for these trials were all similar and included patients with chemotherapy-naïve mCRPC. The primary outcome was occurrence of TRDD. A competing risks regression (CRR) was used to predict TRDD, after accounting for the occurrence of competing events (death or progression). The output of the model was used as the dependent variable on a classification and regression tree (CART) to identify risk groups for TRDD.
Results
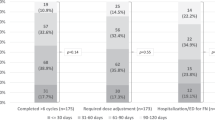
Overall, 1568 patients were considered. Pooled CI of TRDD was 19% after accounting for competing events (death: 474; progression: 59) within 12 months of starting treatment. To build a risk calculator we relied on a CRR that ultimately included age, ECOG performance status, AST, bilirubin, use of analgesics, and presence of diabetes and chronic kidney disease. The CART analysis identified three risk groups that were named: low (model-derived TRDD risk ≤24%), intermediate (25–64%), and high (≥65%) risk group. In each risk group, probability of TRDD during treatment was 14%, 58%, and 79%, and median OS was 24 months, 20 months, and 13 months, respectively (p < 0.001).
Conclusions
Treatment selection in mCRPC remains a challenge. Our model can help clinicians balance Docetaxel toxicity and efficacy. The three risk categories that we identified correlated with OS and this is particularly useful for an optimal shared decision-making process.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Petrylak DP, Tangen CM, Hussain MH, et al. Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med. 2004;351:1513–20.
Tannock IF, de Wit R, Berry WR, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004;351:1502–12.
Berthold DR, Pond GR, Soban F, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer: updated survival in the TAX 327 study. J Clin Oncol. 2008;26:242–5.
Beer TM, Armstrong AJ, Rathkopf DE, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371:424–33.
de Bono JS, Logothetis CJ, Molina A, et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med. 2011;364:1995–2005.
de Bono JS, Oudard S, Ozguroglu M, et al. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet. 2010;376:1147–54.
Kantoff PW, Higano CS, Shore ND, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363:411–22.
Kawalec P, Paszulewicz A, Holko P, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. A systematic review and meta-analysis. Arch Med Sci. 2012;8:767–75.
Parker C, Nilsson S, Heinrich D, et al. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369:213–23.
Ryan CJ, Smith MR, de Bono JS, et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med. 2013;368:138–48.
Scher HI, Fizazi K, Saad F, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367:1187–97.
Templeton AJ, Vera-Badillo FE, Wang L, et al. Translating clinical trials to clinical practice: outcomes of men with metastatic castration resistant prostate cancer treated with docetaxel and prednisone in and out of clinical trials. Ann Oncol. 2013;24:2972–7.
Kongsted P, Svane IM, Lindberg H, et al. Clinical impact of the number of treatment cycles in first-line docetaxel for patients with metastatic castration-resistant prostate cancer. Clin Genitourin Cancer. 2017;15:e281–e287.
Poon DM, Ng J, Chan K. Importance of cycles of chemotherapy and postdocetaxel novel therapies in metastatic castration-resistant prostate cancer. Prostate Int. 2015;3:51–5.
de Morree ES, Vogelzang NJ, Petrylak DP, et al. Association of survival benefit with docetaxel in prostate cancer and total number of cycles administered: a post hoc analysis of the mainsail study. JAMA Oncol. 2017;3:68–75.
Sonpavde G, Bhor M, Hennessy D, et al. Sequencing of cabazitaxel and abiraterone acetate after docetaxel in metastatic castration-resistant prostate cancer: treatment patterns and clinical outcomes in multicenter community-based US oncology practices. Clin Genitourin Cancer. 2015;13:309–18.
James ND, Sydes MR, Clarke NW, et al. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet. 2016;387:1163–77.
Sweeney CJ, Chen YH, Carducci M, et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N. Engl J Med. 2015;373:737–46.
Seyednasrollah F, Koestler DC, Wang T, et al. A DREAM challenge to build prediction models for short-term discontinuation of docetaxel in metastatic castration-resistant prostate cancer. JCO Clin Cancer Inf. 2017;1:1–15.
Petrylak DP, Vogelzang NJ, Budnik N, et al. Docetaxel and prednisone with or without lenalidomide in chemotherapy-naive patients with metastatic castration-resistant prostate cancer (MAINSAIL): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet Oncol. 2015;16:417–25.
Scher HI, Jia X, Chi K, et al. Randomized, open-label phase III trial of docetaxel plus high-dose calcitriol versus docetaxel plus prednisone for patients with castration-resistant prostate cancer. J Clin Oncol. 2011;29:2191–8.
Tannock IF, Fizazi K, Ivanov S, et al. Aflibercept versus placebo in combination with docetaxel and prednisone for treatment of men with metastatic castration-resistant prostate cancer (VENICE): a phase 3, double-blind randomised trial. Lancet Oncol. 2013;14:760–8.
Rich JT, Neely JG, Paniello RC, et al. A practical guide to understanding Kaplan-Meier curves. Otolaryngol Head Neck Surg. 2010;143:331–6.
Bland JM, Altman DG. The logrank test. BMJ. 2004;328:1073.
Dignam JJ, Zhang Q, Kocherginsky M. The use and interpretation of competing risks regression models. Clin Cancer Res. 2012;18:2301–8.
Simon RM, Subramanian J, Li MC, et al. Using cross-validation to evaluate predictive accuracy of survival risk classifiers based on high-dimensional data. Brief Bioinform. 2011;12:203–14.
Breiman L. Classification and regression trees. Belmont, CA: Wadsworth International Group; 1984.
Sathianathen NJ, Alarid-Escudero F, Kuntz KM, et al. A cost-effectiveness analysis of systemic therapy for metastatic hormone-sensitive prostate cancer. Eur Urol Oncol. 2019;2:649–55.
Handy CE, Antonarakis ES. Sequencing treatment for castration-resistant prostate cancer. Curr Treat Options Oncol. 2016;17:64.
Lorente D, Mateo J, Perez-Lopez R, et al. Sequencing of agents in castration-resistant prostate cancer. Lancet Oncol. 2015;16:e279–92.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Martini, A., Parikh, A.B., Sfakianos, J.P. et al. Predicting toxicity-related docetaxel discontinuation and overall survival in metastatic castration-resistant prostate cancer: a pooled analysis of open phase 3 clinical trial data. Prostate Cancer Prostatic Dis 24, 743–749 (2021). https://doi.org/10.1038/s41391-021-00326-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-021-00326-3
This article is cited by
-
The obesity paradox in metastatic castration-resistant prostate cancer
Prostate Cancer and Prostatic Diseases (2022)
-
Is BMI a reliable prognostic parameter in metastatic prostate cancer patients?
Prostate Cancer and Prostatic Diseases (2022)