Abstract
Background
Concurrent with the decrease in the number of men diagnosed with prostate cancer (PCa), the proportion of men with low-risk PCa managed conservatively (active surveillance or watchful waiting) has increased in the United States. We aimed to determine whether this increase is a result of more men being managed conservatively or rather a higher proportion of the diminishing number of low-risk PCa managed this way.
Methods
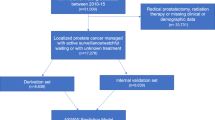
The SEER “Prostate Watchful Waiting Database” identified men managed initially with conservative management between 2010 and 2016. Men > 40 years old who were diagnosed with low-risk (Gleason score 3 + 3, T1–T2a, PSA level < 10 ng/mL) PCa were included. Age-standardized and age-specific PCa incidence and conservative management rates were calculated per 100,000 man-years. The annual percent change in rates for the entire time period was also calculated.
Results
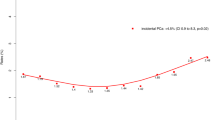
The incidence of low-risk PCa declined by 11.8% per year (95% confidence interval [CI] −15.4% to −8.0%), whereas the number of men assigned to conservative management for low-risk disease did not increase significantly, rising by +3.7% per year (95% CI −0.7% to 8.4%). In age-specific analysis, the number of men < 60 years and those who were 60–69 years managed conservatively increased by +9.6% per year (95% CI 2.7% to 16.9%) and 4.5% per year (95% CI 0.1% to 9.1%), respectively, whereas the number of men ≥ 70 years electing conservative management remained stable at −4% per year (95% CI −11.2% to 3.7%).
Conclusions
The number of men electing conservative management has remained largely stable between 2010 and 2016, despite an increase in the proportion of low-risk PCa managed in this manner.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Chen RC, Rumble RB, Loblaw DA, Finelli A, Ehdaie B, Cooperberg MR, et al. Active surveillance for the management of localized prostate cancer (Cancer Care Ontario Guideline): American Society of Clinical Oncology clinical practice guideline endorsement. J Clin Oncol. 2016;34:2182–90.
Briganti A, Fossati N, Catto JWF, Cornford P, Montorsi F, Mottet N, et al. Active surveillance for low-risk prostate cancer: the European Association of Urology Position in 2018. Eur Urol. 2018;74:357–68.
Mahal BA, Butler S, Franco I, Spratt DE, Rebbeck TR, D’Amico AV, et al. Use of active surveillance or watchful waiting for low-risk prostate cancer and management trends across risk groups in the United States, 2010-2015. JAMA. 2019;321:704–6.
Cooperberg MR, Carroll PR. Trends in management for patients with localized prostate cancer, 1990-2013. JAMA. 2015;314:80–82.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34.
Prostate with Watchful Waiting Database - SEER Data & Software. https://seer.cancer.gov/seerstat/databases/prostate-ww/index.html. Accessed 21 Feb 2019.
Mohler JL, Antonarakis ES, Armstrong AJ, D’Amico AV, Davis BJ, Dorff T, et al. Prostate cancer, version 2.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019;17:479–505.
Jemal A, Fedewa SA, Ma J, Siegel R, Lin CC, Brawley O, et al. Prostate cancer incidence and PSA testing patterns in relation to USPSTF screening recommendations. JAMA. 2015;314:2054–61.
Thompson IM, Canby-Hagino E, Lucia MS. Stage migration and grade inflation in prostate cancer: Will Rogers meets Garrison Keillor. J Natl Cancer Inst. 2005;97:1236–7.
Shoag JE, Cai PY, Gross MD, Gaffney C, Li D, Mao J, et al. Impact of prebiopsy magnetic resonance imaging on biopsy and radical prostatectomy grade concordance. Cancer 2020;126:2986-–90. https://doi.org/10.1002/cncr.32821.
Sathianathen NJ, Omer A, Harriss E, Davies L, Kasivisvanathan V, Punwani S, et al. Negative Predictive Value of Multiparametric Magnetic Resonance Imaging in the Detection of Clinically Significant Prostate Cancer in the Prostate Imaging Reporting and Data System Era: A Systematic Review and Meta-analysis. Eur Urol. 2020;S0302-2838:30223–2. https://doi.org/10.1016/j.eururo.2020.03.048.
Cucchiara V, Cooperberg MR, Dall’Era M, Lin DW, Montorsi F, Schalken JA, et al. Genomic markers in prostate cancer decision making. Eur Urol. 2018;73:572–82.
Loeb S, Shin SS, Broyles DL, Wei JT, Sanda M, Klee G, et al. Prostate Health Index improves multivariable risk prediction of aggressive prostate cancer. BJU Int. 2017;120:61–68.
Ankerst DP, Hoefler J, Bock S, Goodman PJ, Vickers A, Hernandez J, et al. Prostate Cancer Prevention Trial risk calculator 2.0 for the prediction of low- vs high-grade prostate cancer. Urology. 2014;83:1362–7.
Lamy P-J, Allory Y, Gauchez A-S, Asselain B, Beuzeboc P, de Cremoux P, et al. Prognostic biomarkers used for localised prostate cancer management: A systematic review. Eur Urol Focus. 2018;4:790–803.
Weinstock C, Suzman D, Kluetz P, Baxley J, Viviano C, Ibrahim A, et al. Development of treatments for localized prostate cancer in patients eligible for active surveillance: FDA oncology center of excellence public workshop. J Urol. 2019;203:115-9.
Moyer VA.U.S. Preventive Services Task Force Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157:120–34.
Jeong CW, Washington SL, Herlemann A, Gomez SL, Carroll PR, Cooperberg MR. The new Surveillance, Epidemiology, and End Results prostate with watchful waiting database: opportunities and limitations. Eur Urol. 2020;S0302-2838:30045–2. https://doi.org/10.1016/j.eururo.2020.01.009.
Funding
JS and JCH are supported by The Frederick J. and Theresa Dow Wallace Fund of the New York Community Trust. JS is supported by the Damon Runyon Cancer Research Foundation Physician Scientist Training Award.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Al Hussein Al Awamlh, B., Ballman, K.V., Ma, X. et al. Temporal trends in the number of men electing for conservative management for low-risk prostate cancer in the United States. Prostate Cancer Prostatic Dis 23, 714–717 (2020). https://doi.org/10.1038/s41391-020-0252-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-020-0252-0