Abstract
Background
Population-based studies assessing various active surveillance (AS) protocols for prostate cancer, to date, have inferred AS participation by the lack of definitive treatment and use of post-diagnostic testing. This is problematic as evidence suggests that most men do not adhere to AS protocols. We sought to develop a novel method of identifying men on AS or watchful waiting (WW) independent of post-diagnostic testing and aimed to identify possible predictors of follow-up intensity in men on AS/WW.
Methods
A predictive model was developed using SEER watchful waiting data to identify men ≥66 years on AS between 2010–2015, irrespective of post-diagnostic testing, and applied to SEER-Medicare database. AS intensity among different variables including age, prostate-specific antigen (PSA) level, number of total and positive biopsy cores, Charlson comorbidity index, race (Black vs. non-Black), US census region, and county poverty, income, and education levels were compared using multivariable regression analyses for PSA testing, surveillance biopsy, and magnetic resonance imaging (MRI).
Results
A total of 2238 men were identified as being on AS. Of which, 81%, 33%, and 10% had a PSA test, surveillance biopsy, and MRI scan within 1–2 years, respectively. On multivariable analyses, Black men were less likely to have a PSA test (adjusted rate ratio [ARR] 0.60, 95% CI: 0.53–0.69), MRI scan (ARR 0.40, 95% CI: 0.24–0.68), and surveillance biopsy (ARR 0.71, 95% CI: 0.55–0.92) than non-Black men. Men within the highest income quintile were more likely to undergo PSA test (ARR 1.16, 95% CI: 1.05–1.27) and MRI scan (ARR 1.60, 95% CI 1.15–2.27) compared to men with the lowest income.
Conclusions
Black men and men with lower incomes on AS underwent less rigorous monitoring. Further study is needed to understand and ameliorate differences in AS rigor stemming from sociodemographic differences.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the Surveillance, Epidemiology, and End Results (SEER) Program and SEER-Medicare but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the National Cancer Institute – SEER Database (https://seer.cancer.gov/data/)
References
Chen RC, Rumble RB, Loblaw DA, Finelli A, Ehdaie B, Cooperberg MR, et al. Active surveillance for the management of localized prostate cancer (Cancer Care Ontario Guideline): American Society of Clinical Oncology clinical practice guideline endorsement. J Clin Oncol. 2016;34:2182–90.
Auffenberg GB, Lane BR, Linsell S, Cher ML, Miller DC. Practice- vs physician-level variation in use of active surveillance for men with low-risk prostate cancer: implications for collaborative quality improvement. JAMA Surg. 2017;152:978–80.
Al Hussein Al Awamlh B, Patel N, Ma X, Calaway A, Ponsky L, Hu JC, et al. Variation in the use of active surveillance for low-risk prostate cancer across US census regions. Front Oncol. 2021;11:644885.
Peterson S, Basak R, Moon DH, Liang C, Basak RS, Walden S, et al. Population-based cohort of prostate cancer patients on active surveillance (AS): guideline adherence, conversion to treatment and decisional regret. J Clin Oncol. 2019;37:6512–6512.
Filson CP, Schroeck FR, Ye Z, Wei JT, Hollenbeck BK, Miller DC. Variation in use of active surveillance among men undergoing expectant treatment for early stage prostate cancer. J Urol. 2014;192:75–80.
Loeb S, Walter D, Curnyn C, Gold HT, Lepor H, Makarov DV. How active is active surveillance? Intensity of followup during active surveillance for prostate cancer in the United States. J Urol. 2016;196(Sep):721–6.
Krishna S, Fan Y, Jarosek S, Adejoro O, Chamie K, Konety B. Racial disparities in active surveillance for prostate cancer. J Urol. 2017;197:342–9.
Sayyid RK, Klotz L, Benton JZ, Lodh A, Lambert JH, Woodruff P, et al. Influence of sociodemographic factors on definitive intervention among low-risk active surveillance patients. Urology. 2021;155:117–23.
Butler SS, Loeb S, Cole AP, Zaslowe-Dude C, Muralidhar V, Kim DW, et al. United States trends in active surveillance or watchful waiting across patient socioeconomic status from 2010 to 2015. Prostate Cancer Prostatic Dis. 2020;23:179–83.
Deka R, Courtney PT, Parsons JK, Nelson TJ, Nalawade V, Luterstein E, et al. Association between African American race and clinical outcomes in men treated for low-risk prostate cancer with active surveillance. JAMA. 2020;324:1747–54.
Prostate with Watchful Waiting Database - SEER Data & Software [Internet]. [cited 2019 Feb 21]. Available from: https://seer.cancer.gov/seerstat/databases/prostate-ww/index.html
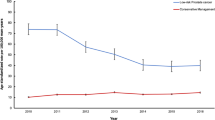
Al Hussein Al Awamlh B, Ma X, Scherr D, Hu JC, Shoag JE. Temporal changes in demographic and clinical characteristics of men with prostate cancer electing for conservative management in the united states. Urology. 2020;137:60–5.
Scosyrev E, Messing J, Noyes K, Veazie P, Messing E. Surveillance Epidemiology and End Results (SEER) program and population-based research in urologic oncology: an overview. Urol Oncol. 2012;30:126–32.
Brief Description of SEER-Medicare Database [Internet]. [cited 2020 Dec 30]. Available from: https://healthcaredelivery.cancer.gov/seermedicare/overview/
healthcaredelivery.cancer.gov/seermedicare/considerations/comorbidity.input.file.example.sas [Internet]. [cited 2020 Dec 30]. Available from: https://healthcaredelivery.cancer.gov/seermedicare/considerations/comorbidity.input.file.example.sas
Shoag JE, Cai PY, Gross MD, Gaffney C, Li D, Mao J, et al. Impact of prebiopsy magnetic resonance imaging on biopsy and radical prostatectomy grade concordance. Cancer. 2020;126:2986–90.
Macleod LC, Yabes JG, Fam MM, Bandari J, Yu M, Maganty A, et al. Multiparametric magnetic resonance imaging is associated with increased medicare spending in prostate cancer active surveillance. Eur Urol Focus 2020;6:242–8.
Dess RT, Hartman HE, Mahal BA, Soni PD, Jackson WC, Cooperberg MR, et al. Association of black race with prostate cancer-specific and other-cause mortality. JAMA Oncol. 2019;5:975–83.
Iremashvili V, Soloway MS, Rosenberg DL, Manoharan M. Clinical and demographic characteristics associated with prostate cancer progression in patients on active surveillance. J Urol. 2012;187:1594–9.
Odom BD, Mir MC, Hughes S, Senechal C, Santy A, Eyraud R, et al. Active surveillance for low-risk prostate cancer in African American men: a multi-institutional experience. Urology. 2014;83:364–8.
Al Hussein Al Awamlh B, Ma X, Christos P, Hu JC, Shoag JE. Active surveillance for black men with low-risk prostate cancer in the United States. N. Engl J Med. 2019;381:2581–2.
DeWitt-Foy ME, Gam K, Modlin C, Kim SP, Abouassaly R. Race, decisional regret and prostate cancer beliefs: identifying targets to reduce racial disparities in prostate cancer. J Urol. 2021;205:426–33.
Walton EL, Deebajah M, Keeley J, Fakhouri S, Yaguchi G, Pantelic M, et al. Barriers to obtaining prostate multi-parametric magnetic resonance imaging in African-American men on active surveillance for prostate cancer. Cancer Med. 2019;8:3659–65.
Chamie K, Williams SB, Hershman DL, Wright JD, Nguyen PL, Hu JC. Population-based assessment of determining predictors for quality of prostate cancer surveillance. Cancer. 2015;121:4150–7.
Carter HB, Walsh PC, Landis P, Epstein JI. Expectant management of nonpalpable prostate cancer with curative intent: preliminary results. J Urol. 2002;167:1231–4.
Bul M, Zhu X, Valdagni R, Pickles T, Kakehi Y, Rannikko A, et al. Active surveillance for low-risk prostate cancer worldwide: the PRIAS study. Eur Urol. 2013;63:597–603.
Hoffman RM, Mott SL, McDowell BD, Anand ST, Nepple KG. Trends and practices for managing low-risk prostate cancer: a SEER-Medicare study. Prostate Cancer Prostatic Dis. 2022;25:100–8.
Ginsburg KB, Auffenberg GB, Qi J, Powell IJ, Linsell SM, Montie JE, et al. Risk of becoming lost to follow-up during active surveillance for prostate cancer. Eur Urol. 2018;74:704–7.
Bhanji Y, Rowe SP, Pavlovich CP. New imaging modalities to consider for men with prostate cancer on active surveillance. World J Urol. 2022;40:51–9.
Funding
The work presented here was not directly funded by an outside organization or sponsor. JES is supported by the Frederick J. and Theresa Dow Fund of the New York Community Trust, the Vinney Scholars Award, and a Damon Runyon Cancer Research Foundation Physician-Scientist Training Award. JES had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Contributions
Study conception and design: BA, JES; Acquisition of data: BA, XW, JES; Analysis and interpretation of data: BA, XW, DAB, KAM, RMH, SPB, PL, WWS, CAG, JES; Drafting of manuscript: BA, XW, DAB, KAM, RMH, SPB, PL, WWS, CAG, JES; Critical revision: BA, XW, DAB, KAM, RMH, SPB, PL, WWS, CAG, JES.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Al Hussein Al Awamlh, B., Wu, X., Barocas, D.A. et al. Intensity of observation with active surveillance or watchful waiting in men with prostate cancer in the United States. Prostate Cancer Prostatic Dis 26, 395–402 (2023). https://doi.org/10.1038/s41391-022-00580-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00580-z
This article is cited by
-
The evolving standards of active surveillance monitoring
Prostate Cancer and Prostatic Diseases (2023)
-
Concerns regarding prostate cancer screening guidelines in minority populations
Prostate Cancer and Prostatic Diseases (2023)
-
Patient and physician perspectives on treatments for low-risk prostate cancer: a qualitative study
BMC Cancer (2023)