Abstract
Background
In men with recurrence of prostate cancer post radiation therapy, further treatment remains a challenge. The default salvage option of androgen-deprivation therapy (ADT) has adverse effects. Alternatively, selected men may be offered salvage therapy to the prostate. Herein, we present long-term oncological outcomes of two whole-gland ablation techniques, cryotherapy (sCT) and high-intensity-focused ultrasound (sHIFU).
Methods
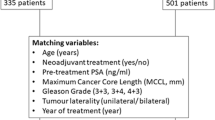
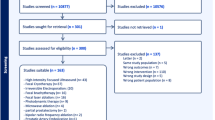
Men undergoing sCT (1995–2004) and sHIFU (2006–2018) at Western University were identified. Oncological endpoints included biochemical recurrence (BCR), ADT initiation, metastases, castration resistance (CRPC), and prostate cancer-specific mortality (PCSM). Survival analysis with competing risks of mortality was performed. Multivariable analysis was performed using Fine and Gray regression.
Results
A total of 187 men underwent sCT and 113 sHIFU. Mean (SD) age of the entire cohort was 69.9 (5.9 years), median pre-radiation PSA 9.6 ng/ml (IQR 6.1–15.2), and pre-salvage PSA 4.5 ng/ml (IQR 2.8–7.0). Median total follow-up was 116 months (IQR 67.5–173.8). A total of 170 (57.6%) developed BCR, 68 (23.4%) metastases, 143 (49.3%) were started on ADT, 58 (20.1%) developed CRPC, and 162 (56%) patients died of which 59 (36.4%) were of prostate cancer. On multivariable analysis, sHIFU (HR 1.65, 95% CI 1.15–2.36, p = 0.006) and pre-salvage PSA (HR 1.09, 95% CI 1.06–1.13, p < 0.0001) were associated with a higher risk of BCR. Similarly, sHIFU patients had a higher risk of CRPC (HR 2.31, 95% CI 1.23–4.35, p = 0.009). The cumulative incidence (for both treatments) of PCSM was 16.5% (95% CI 12.2–21.4%) at 10 years and 28.4% (95% CI 22.1–34.9%) at 20 years, with no difference between treatment modalities. Pre-salvage PSA was a common predictor for the measured oncological outcomes.
Conclusions
Although sHIFU had higher BCR and CRPC rates, there were no differences in PCSM when compared with sCT. The long-term oncological data on two ablation techniques highlighted that only 50% of patients started ADT after 10-year follow-up.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Zelefsky MJ, Eastham JA, Cronin AM, Fuks Z, Zhang Z, Yamada Y, et al. Metastasis after radical prostatectomy or external beam radiotherapy for patients with clinically localized prostate cancer: a comparison of clinical cohorts adjusted for case mix. J Clin Oncol. 2010;28:1508–13.
Beckmann K, Garmo H, Adolfsson J, Bosco C, Johansson E, Robinson D et al. Androgen deprivation therapies and changes in comorbidity: a comparison of gonadotropin-releasing hormone agonists and antiandrogen monotherapy as primary therapy in men with high-risk prostate cancer. Eur Urol 2018; 75:676–83.
Siddiqui KM, Billia M, Williams A, Alzahrani A, Chin JL. Comparative morbidity of ablative energy-based salvage treatments for radio-recurrent prostate cancer. Can Urol Assoc J. 2015;9:325–9.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509.
Gray RJ. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat. 1988;16:1141–54.
Duchesne GM, Woo HH, Bassett JK, Bowe SJ, D’Este C, Frydenberg M, et al. Timing of androgen-deprivation therapy in patients with prostate cancer with a rising PSA (TROG 03.06 and VCOG PR 01-03 [TOAD]): a randomised, multicentre, non-blinded, phase 3 trial. Lancet Oncol. 2016;17:727–37.
Kongnyuy M, Berg CJ, Kosinski KE, Habibian DJ, Schiff JT, Corcoran AT, et al. Salvage focal cryosurgery may delay use of androgen deprivation therapy in cryotherapy and radiation recurrent prostate cancer patients. Int J Hyperth. 2017;33:810–3.
Pisters LL, Leibovici D, Blute M, Zincke H, Sebo TJ, Slezak JM, et al. Locally recurrent prostate cancer after initial radiation therapy: a comparison of salvage radical prostatectomy versus cryotherapy. J Urol. 2009;182:517–25. Discussion 525-517.
Wenske S, Quarrier S, Katz AE. Salvage cryosurgery of the prostate for failure after primary radiotherapy or cryosurgery: long-term clinical, functional, and oncologic outcomes in a large cohort at a tertiary referral centre. Eur Urol. 2013;64:1–7.
Steele EM, Holmes JA. A review of salvage treatment options for disease progression after radiation therapy for localized prostate cancer. Urol Oncol. 2019;37:582–98.
Crouzet S, Blana A, Murat FJ, Pasticier G, Brown SCW, Conti GN, et al. Salvage high-intensity focused ultrasound (HIFU) for locally recurrent prostate cancer after failed radiation therapy: multi-institutional analysis of 418 patients. BJU Int. 2017;119:896–904.
Chade DC, Shariat SF, Cronin AM, Savage CJ, Karnes RJ, Blute ML, et al. Salvage radical prostatectomy for radiation-recurrent prostate cancer: a multi-institutional collaboration. Eur Urol. 2011;60:205–10.
Nair SM, Lyon T, Dewar M, Rangel L, Abed H, Hetou K, et al. Salvage cryotherapy versus salvage radical prostatectomy for radiorecurrent prostate cancer: long-term oncologic outcomes. Eur Urol. 2019;18:e872.
Williams AK, Martinez CH, Lu C, Ng CK, Pautler SE, Chin JL. Disease-free survival following salvage cryotherapy for biopsy-proven radio-recurrent prostate cancer. Eur Urol. 2011;60:405–10.
Spiess PE, Levy DA, Mouraviev V, Pisters LL, Jones JS. Predictors of biochemical failure in patients undergoing prostate whole-gland salvage cryotherapy: a novel risk stratification model. BJU Int. 2013;112:E256–61.
Ceci F, Castellucci P, Graziani T, Farolfi A, Fonti C, Lodi F et al. (68)Ga-PSMA-11 PET/CT in314 recurrent prostate cancer: efficacy in different clinical stages of PSA failure after radical315 therapy. Eur J Nucl Med Mol Imaging 2019;46:31–9
Pasoglou V, Michoux N, Van Damme J, Van Nieuwenhove S, Halut M, Triqueneaux P, et al. Pattern of metastatic deposit in recurrent prostate cancer: a whole-body MRI-based assessment of lesion distribution and effect of primary treatment. World J Urol. 2019;37:2585–95.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Nair, S.M., Peters, M., Kurver, P. et al. Long-term outcomes of two ablation techniques for treatment of radio-recurrent prostate cancer. Prostate Cancer Prostatic Dis 24, 186–192 (2021). https://doi.org/10.1038/s41391-020-00265-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-020-00265-5