Abstract
Bakcground
The aim of this study was to evaluate the efficacy and safety of citrate versus heparin anticoagulation for CRRT in critically-ill children.
Methods
This retrospective comparative cohort reviewed the clinical records of critically-ill children undergoing CRRT with either RCA or systemic heparin anticoagulation. The primary outcome measure was hemofilter survival time. Secondary outcomes included the comparison of complications and metabolic disorders.
Results
A total of 131 patients (55 RCA and 76 systemic heparin) were included, in which a cumulative number of 280 hemofilters were used (115 in RCA with 5762 h total CRRT time, and 165 in systemic heparin with 6230 h total CRRT time). Hemofilter survival was significantly longer for RCA (51.0 h; IQR: 24–67 h) compared to systemic heparin (29.5 h; IQR, 17–48 h) (p = 0.002). Clotting-related hemofilter failure occurred in 9.6% of the RCA group compared to 19.6% in the systemic heparin group (p = 0.038). Citrate accumulation occurred in 4 (3.5%) of 115 RCA sessions. Hypocalcemia and metabolic alkalosis episodes were significantly more frequent in RCA recipients (35.7% vs 15.2%, p < 0.0001; 33.0% vs 19.4%, p = 0.009).
Conclusion
RCA is a safe and effective anticoagulation method for CRRT in critically-ill children and it prolongs hemofilter survival.
Impact
-
RCA is superior to systemic heparin for the prolongation of circuit survival (overall and for clotting-related loss) during CRRT.
-
These data indicate that RCA can be used to maximize the effective delivery of CRRT in critically-ill patients admitted to the PICU.
-
There are potential cost-saving implications from our results owing to benefits such as less circuit downtime and fewer circuit changes.
Similar content being viewed by others
Introduction
Continuous renal replacement therapy (CRRT) is the most commonly used renal replacement therapy (RRT) in critically-ill children. It is used in various indications, including acute kidney injury (AKI), severe electrolyte imbalance/metabolic acidosis, refractory or diuretic-resistant fluid overload, intoxications, and inborn metabolic disorders.1,2 Therapeutic efficacy is associated with a number of factors, one of which is circuit survival (CS) that depends on anticoagulation.3 During CRRT, ideal anticoagulation should be able to sustain the circuit while causing minimal side effects on circulation. It should be safe, available, consistent, easily monitored, and reversible. Premature clotting of the CRRT circuit can lead to increased workload and health care costs, as well as adverse outcomes for the patient.4,5 Thus, efficient anticoagulation protocols are required to prevent clotting and prolong circuit life (CL).
In clinical practice, systemic heparin anticoagulation and regional citrate anticoagulation (RCA) are the two main anticoagulation strategies for CRRT. The major advantages of using heparin are its low cost, ease of administration, monitoring, and reversibility. However, the increased risks for bleeding with heparin use is a major concern in critically-ill children who are predisposed to bleeding for many reasons such as surgical procedures, trauma, severe liver dysfunction, and thrombocytopenia.6 RCA is favoured by many intensivist as it avoids systemic anticoagulation and inhibits the clotting cascade by chelating ionized calcium (iCa) preventing the initiation of the coagulation cascade also thrombin formation.7
RCA was studied for the first time by Mehta et al who examined a group of 18 adults with acute renal failure. The study revealed the superiority of RCA over heparin in terms of bleeding risk and thrombocytopenia.8 In subsequent adult studies, RCA has been demonstrated to be superior to systemic heparin anticoagulation based on reduced clotting, prolonged hemofilter life, and lower risk of bleeding.7,8,9,10,11,12,13 Indeed, the 2012 kidney disease improving global outcomes (KDIGO) guidelines recommended using RCA for adult patients at increased risk of bleeding –given that there are no contraindications for citrate infusion.10 In critically-ill children requiring dialysis, citrate anticoagulation was used successfully by Bunchman et al. in the early 2000s.14 However, when compared to adults, research concerning critical-ill children receiving CRRT is limited in terms of evaluating RCA for hemofilter survival, treatment efficacy, and safety, particularly in Turkey. Furthermore, available studies are mostly comprised of limited patient series and some results are conflicting.7,9,15,16,17,18,19,20,21,22 This study aims to compare RCA and systemic heparin in pediatric CRRT to assess safety and efficacy by examining hemofilter survival, complications, and metabolic disturbance.
Materials and methods
Study design
This study was conducted in a multidisciplinary tertiary PICU of Prof. Dr. Suleyman Yalcin City Hospital in Istanbul, Turkey. Our research design is based on a retrospective single-center cohort. The study was approved by Medical Ethics Committee of our hospital (Registration number: 2021/0017). Patient consent was waived due to retrospective nature of the study.
Study population
All critically-ill children who were admitted to our general PICU from April 2015 to January 2021 and received CRRT with either systemic anticoagulation (heparin) or RCA were assessed for enrolment. Patients were excluded if they fulfilled at least one of the following criteria: (i) insufficient data, (ii) received anticoagulation therapy for therapeutic purposes during CRRT or up to 24 h (h) before the start of CRRT, (iii) received an RRT modality other than CRRT (intermittent or peritoneal hemodialysis), (iv) underwent RRT for various other reasons, such as chronic renal failure, before admission to the unit.
The subjects were divided into two groups: one group comprising patients who received RCA and the second group comprising of those who received systemic anticoagulant with heparin (Fig. 1).
Data collection and definitions
CRRT was performed according to locally-defined protocols. Demographic data, laboratory results, and CRRT-specific data were extracted from medical records or any other pertinent clinical data storage (physical files, notes etc.). Age, weight, sex, presence of comorbidities, diagnosis, Pediatric Risk of Mortality (PRISM) III score, and risk factors associated with bleeding were recorded at admission to the PICU. Admission diagnoses were classified into eleven groups as follows: renal disease, hemato-oncologic disease, sepsis, pneumonia, respiratory failure, liver failure, cardiac arrest, metabolic disease, cardiopathies, intoxication, acute abdomen, and others. Identified risk factors for bleeding were admission due to major surgery or trauma, thrombocytopenia/coagulopathy, hematologic malignancies, sepsis, respiratory failure (requiring invasive mechanical ventilation), hepatic failure, extracorporeal membrane oxygenation (ECMO), and higher PRISM III score at admission.23,24
Clinical data collected at CRRT initiation were as follows: indication for CRRT initiation, percentage of fluid overload (%FO), urine output (UO), need for invasive mechanical ventilation, presence of multiple organ dysfunction syndrome (MODS), need for ECMO, vasoactive inotropic support / vasoactive inotrope score (VIS), and stage of AKI. The indications for CRRT initiation were classified as electrolyte or acid-base imbalance, AKI, FO, hyperammonemia, acute exacerbation of inborn metabolic disorders, intoxication, tumor lysis syndrome, and rhabdomyolysis. The indications for commencing CRRT were identified from the documentation of the attending intensivist. Survival was defined as surviving until pediatric intensive care unit (PICU) discharge.
%FO at CRRT initiation was calculated using the following formula: (total fluid intake [L] – total fluid output [L] / (PICU admission weight [kg]) × 100.25 Analysis was performed separately for three FO categories (<10%, 10–20%, and >20%), which were defined based on previous studies.26,27 UO was calculated for the 24 h before the initiation of CRRT. VIS was calculated using the following formula: (dose of dopamine + dobutamine + [100 × epinephrine] + [100 × norepinephrine] + [10 × milrinone] [all in microgram/kg/min] + [10.000 × vasopressin] [U/kg/hr]).28 AKI was classified using KDIGO criteria based on changes in serum creatinine. If baseline serum creatinine was not available, we instead utilized the value of UO in the last 24 h before CRRT initiation.10 Finally, MODS was defined as the presence of at least three failed organs, according to the guidelines put forth by the Pediatric Sepsis Consensus Conference.28
Biochemical variables collected at the initiation of CRRT were as follows: creatinine, urea, hemoglobin, platelet count, pH/arterial blood gases, lactate, serum electrolytes, prothrombin time (PT) (sec), activated partial thromboplastin time (aPTT) (sec) and international normalization ratio (INR).
The CRRT operating parameters were as follows: total CRRT time, the number of hemofilters used and survival, the size of hemofilters and catheters, CS time (irrespective of cause), CRRT parameters (pump flow rate, dialysate/replacement flow rates), and the calcium infusion rate and citrate dosage in RCA recipients. Reasons for disconnection/hemofilter failure were categorized as (i) clotting in the circuit, (ii) vascular access malfunction, (iii) scheduled replacement after 72 h, (iv) end of CRRT treatment, and (v) technical issues/alarms.
CS time was defined as the time from the beginning of CRRT with the corresponding filter until filter replacement (until the upper limit for regular filter replacement; 72 h) or termination of CRRT session due to various reasons including achievement of treatment goals or death or clotting & non-clotting events (vascular access malfunction, technical reasons).
Electrolyte-related and metabolic disturbances during CRRT were recorded and categorized as follows: hypocalcemia (iCa++ < 0.9 mmol/L), hypercalcemia (iCa++, > 1.25 mmol/L), hyponatremia (Na < 130 mmol/L), hypernatremia (Na > 145 mmol/L), hypomagnesemia (< 1.5 mg/dl), hypophosphatemia (< 2.5 mg/dL), metabolic acidosis (pH < 7.36 or base excess [BE] < −3), and metabolic alkalosis (pH > 7.46 or BE > + 3). Citrate accumulation (CA) was defined as a ratio of total calcium (totCal++)-to-ionized calcium (iCal + +) of > 2.5 for longer than 48 h with high anion gap metabolic acidosis.29
The volume of packed red cells transfused during CRRT (and after circuit clotting) was recorded for each circuit. Transfusions were initiated in response to hemoglobin concentration measurements obtained from regular blood sampling, with a threshold of 7.0 g/dL during CRRT.30 If the reason for hemoglobin decrease below 7.0 g/dL was circuit clotting, the indication for transfusion was defined to be due to the circuit clotting. Bleeding site (catheter insertion site, gastrointestinal site etc.) and bleeding severity were recorded. Severe bleeding was defined as bleeding associated with hypotension or tachycardia, bleeding that necessitated red blood cell transfusion, or a 2 g/dl drop in hemoglobin within 24 h.
A number of other variables that may affect circuit survival, as suggested by prior research,5,31,32 were also assessed. These variables included use of femoral vein catheter, low patient weight (< 10 kg), small hemofilter size (60 m2 or 93 m2), lower pump flow rate (< 100 mL/min) and use of systemic anticoagulation with heparin.
CRRT protocol and anticoagulation method
Initial CRRT was performed according to our institutional protocol. All CRRT treatments were performed using a Prismaflex HF20, M60 and M100 control unit (Gambro, Sweden and Baxter). Continuous veno-venous hemodiafiltration was administered to all subjects. Venous access was obtained by dual lumen hemodialysis catheters (7 F to 12 F) depending on the age and weight of the child.
During treatments, blood flow rate was set 3–8 ml/kg/min with respect to patient weight, catheter size and filter surface. Total clearance rate was set between 2–3 L/1.73 m2/hr for the majority of patients, while higher total clearance rates (up to a maximum of 5 L/1.73 m2/hr) were reached in cases with specific indications, such as intoxication or hyperammonemia. The dialysate flow rate, replacement fluid rate and ultrafiltration rate values were customized based on diagnosis, hemodynamic parameters and FO values. In both anticoagulation strategies, while regulating dialysate and replacement flows, care was taken not to increase the filtration fraction above 25%.
Poly aryl ethylene sulphone (PAES) membranes (Prismaflex HF20; circuit volume 60 ml, surface area 0.2 m2) or AN69 membranes (Prismaflex M60; circuit volume 93 ml, surface area 0.6 m2 and Prismaflex M100; circuit volume 152 ml, surface area 0.9 m2) were used. Children with a body weight of < 10 kg underwent CRRT using a Prismaflex HF20 set, those with a body weight between 10 kg and 25 kg received the Prismaflex M60 set, while those exceeding 25 kg received a Prismaflex M100 set.
Heparinized saline (5 U/mL) was used for hemofilter priming. In patients with high risk for hemorrhage, the circuit was primed with physiological saline only. An overall exception was use of blood to prime the circuit in children with a bodyweight of less than 10 kg and those with hemoglobin values below 10 g/dL. For this purpose, erythrocyte suspension was diluted 1-to-1 with saline.
Anticoagulation method
Before March 2017, RCA was not performed at our center; thus, the anticoagulation protocol was systemic heparin in all patients admitted before this date. After this date, anticoagulation was chosen based on age, clinical characteristics and diagnosis.
For heparin, infusion was started with 10 international units (IU)/kg/hr pre-filter. The heparin dose was subsequently adjusted toward a target postfilter activated clotting time (ACT) of 180–220 s. Dialysis and replacement solutions were the Dialisan (DVVHD BG2D, Baxter) and Prism0calB22 (Baxter) solutions.
For citrate administration, a Prismaflex system (Baxter), employing an automated RCA method with commercially available citrate-buffered solution (Prismocitrate 18/0, Baxter) and compatible bicarbonate dialysate solutions (Prism0cal B22, Baxter), was used. Citrate flow was coupled to blood flow and adjusted by the CRRT device to achieve the prescribed citrate dose (3 mmol per L of blood). CRRT was performed with pre-filter citrate anticoagulation and post-filter replacement fluid. Citrate effect was neutralized using a continuous calcium infusion, calcium gluconate 10% 50/50 with dextrose 5% (116 mmol/L). Calcium infusion was administered through a different central venous line. Only when a separate central line was not available, we administered calcium infusion through the return line of the circuit. An initial infusion rate of 1 mL/kg/h was used to maintain ionized calcium blood level. Calcium compensation was determined according to systemic ionized calcium values. The filter target iCa++ level was between 0.25 and 0.35 mmol/L and the patient’s iCa++ target was between 1 and 1.2 mmol/L. The monitoring of iCa++ concentrations was performed at several time points to ensure maintenance of target concentrations: at the 30th minute, the first, second and fourth hour of therapy, and then routinely every 4 h. Patient calcium levels were also checked one hour after any change in blood flow, citrate concentration, or dialysis. Biochemical indicators and electrolytes were checked every 12–24 h in both anticoagulation strategies.
In the presence of CA, interventions were made to reduce blood flow rate or citrate flow rate/dose, or to increase dialysate flow rate to facilitate citrate clearance. In order to correct ionized hypocalcemia, calcium infusion rate was increased. In case of metabolic alkalosis, in addition to the interventions performed for CA, we administered 0.9% sodium chloride infusion as pre- or post-replacement fluid.29,33
Statistical analysis
The demographic and clinical characteristics of the study subjects were described as well as variables associated with the filter. Characteristics of patients, as n (percent) or median (interquartile range [IQR]) for categorical and continuous variables, respectively, and were compared among groups using chi-square or Mann-Whitney tests, as appropriate. Results were evaluated with a significance value of p < 0.05. Kaplan-Meier survival analysis was applied for survival curves. The median survival for each group, with its respective 95% confidence interval (CI), was reported, and a comparison of the curves was tested using a log-rank test. The magnitude of the effect of the anticoagulant on clotting in the filter was analyzed using Cox’s non-parametric proportional hazards model, which was adjusted for potential confounding variables (size of the filter and pump flow) that could affect the lifetime of the filter. The statistical analysis was performed using the SPSS (version 23.0) software (SPSS Inc., Chicago, IL).
Results
During the 6-year period, 2410 patients were admitted to the PICU and 163 patients received CRRT treatment. All 163 patients were analyzed in the study. Thirty-two children were excluded based on mentioned criteria and a final total of 131 children were included in final analysis. The flow-chart describing participant inclusion is shown in Fig. 1.
Description of the study population
A total of 131 patients (55 in the RCA group and 76 in the systemic heparin group) were included in the analysis. The demographic and clinical characteristics of the patients were largely similar in the two groups (Table 1), except for the presence of liver failure and hyperammonemia, which were more frequent among heparin recipients (p = 0.010, p = 0.044), and the frequency of tumor lysis syndrome which was more common in the RCA group (p = 0.029). There was no significant difference in length of PICU stay and PICU survival.
CRRT and hemofilter characteristics
A total of 11,992 h of dialysis therapy (RCA group 5762 h, heparin group 6230 h) were included in the analysis (Table 2). Cumulatively, a total of 280 hemofilters/circuits were used in all therapies, 115 in the RCA group and 165 in the systemic heparin group.
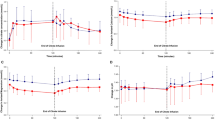
Kaplan Meier analysis showing overall CS time (for all reasons of circuit disconnection) was significantly higher in the RCA group compared to the systemic heparin group [51.0 h (95% CI 39.6–62.4 h) vs. 29.5 h (95% CI 20.5–37.5 h); p = 0.024] (Fig. 2). Similarly, CS time limited by clotting hemofilter was significantly higher in the RCA group [38 h (95% CI 20.7–55.3 h) vs. 15 h (95% CI 7.1–20.9 h); p = 0.001] (Fig. 3).
In the RCA group, there were 11 events of hemofilter removal due to clotting. The systemic heparin group presented with 32 such events, which was significantly higher than the RCA group (respectively; 19.4% vs. 9.6%, p = 0.03). Other reasons of circuit disconnection were not different between groups (Table 3).
Cox’s proportional risk analysis showed that the risk of hemofilter clotting (median CS time limited by clotting hemofilter) was 3.3-fold higher with the use of systemic heparin compared to RCA (HR: 3.30; 95% CI: 1.57–7.09; p = 0.002). Dialysis catheter placement, low weight, small filter size and low pump flow rates were not significantly associated with hemofilter clotting (Table 4).
Safety issues
Bleeding complication
Among all subjects, 20 episodes of severe bleeding (6 in the RCA group and 14 in the systemic heparin group) occurred. The frequency of severe bleeding was similar in the two groups (p = 0.35). There was no significant difference in red cell transfusion ratio. The RCA group had a significantly lower frequency of circuit clotting-related transfusions-to-total transfusions compared to the heparin group (12.5% vs. 42.5%, respectively) (p < 0.001) (Table 5).
Metabolic complications
The most frequent complications were hypocalcemia (35.7% in the RCA group, 15.2% in the heparin group) and metabolic alkalosis (33% in the RCA group, 19.4% in the heparin group). Both of these complications were significantly more common with RCA than systemic heparin (p < 0.001 and p = 0.009). There were 4 cases of CA (3.5%). Median totCa++ to iCal++ index (CaI) was 2.24 (IQR: 1.92- 2.24), and the maximum CaI was 2.59 with metabolic acidosis. The groups were similar in terms of other electrolyte imbalances (hypercalcemia, hyponatremia, hypernatremia, hypomagnesemia, hypophosphatemia) (Table 6). No association was found between metabolic complications and citrate dosage, patient weight, dialysate, or replacement flow rate (p > 0.05, data not shown).
Discussion
The key findings of this study are that RCA is superior to systemic heparin for the prolongation of CS (overall and for clotting-related loss) during CRRT. RCA also reduces hemofilter failure due to clotting and need for transfusion after circuit clotting. It has manageable and limited side effects like hypocalcemia, CA and metabolic alkalosis. Therefore, the current study confirms that RCA is relatively safe and can prolong the survival of hemofilters as compared to heparin anticoagulation, which conforms with the data provided by several pediatric studies. Our data specifically indicate that RCA can be used to maximize the effective delivery of CRRT in critically-ill patients admitted to the PICU. There are also potential cost-saving implications from our results owing to benefits such as less circuit downtime and fewer circuit changes.
Although no significant difference was found between RCA and systemic heparin in some adult studies evaluating anticoagulation efficacy, RCA has been emphasized as a more effective method in recent years, and this has resulted in the recognition of RCA as the recommended approach.6,11,12,34,35 In the meta-analysis of adult studies conducted by Liu et al, it was stated that the use of RCA prolonged filter life by an average of 15.6 h compared to systemic heparin.11 Recently, in a randomized controlled study conducted by Zarbock et al in adults (596 patients), it was reported that RCA prolonged filter life (47 h vs 26 h) compared to systemic heparin.35 Few studies have been carried out in children regarding the anticoagulation strategy in CRRT and most of these studies were conducted in small series. Nonetheless, in the majority of these studies, RCA has been shown to prolong mesh life compared to systemic heparin.17,18,19,22,31,36,37,38,39,40 In a prospective study by Brophy et al on 138 patients and 442 CRRT circuits, no significant difference was found between RCA and systemic heparin use in terms of circuit life (42.1 ± 27.1 h vs. 44.7 ± 35.9 h), albeit systemic heparin was found to cause increased risks for severe bleeding.41 In recent years, with the development of reliable dialysis devices with very small extracorporeal volumes, CRRT treatment has been used more frequently in young infants and newborns, as well as in adult and pediatric cases.37,42,43 Although the number of cases is limited, RCA can be used safely in newborns receiving CRRT. There are reported publications in this age groups.16,42,43,44,45 In the Critical Care Nephrology Section of The European Society of Paediatric and Neonatal Intensive Care (ESPNIC), as a result of the evaluation of current pediatric and neonatal studies, it was reported that RCA may extend circuit life by reducing coagulation.46
In our study, median hemofilter survival was 51.0 h (IQR: 24–67), which was similar to some pediatric studies,17,18,36,40 but shorter than those reported by other pediatric studies.14,22,38 These differences between the filter lifetimes in the studies may be due to variations in filter size, catheter site, citrate concentration used, targeted ionized calcium level, and age groups.22,47
CS time is dependent on many factors including clotting and non-clotting events (vascular access malfunction and technical issues/alarms etc.).19,22 In our study, the rate of hemofilter failure due to clotting was significantly higher in the systemic heparin group (19.4% vs. 9.4%). In addition, in our subgroup analysis, the median CS time for clotting hemofilters was significantly higher in the RCA group than in the systemic heparin group (15 h vs. 28 h). Similar results were found in other pediatric studies.19,22,36 Moreover, the CS time is claimed to be influenced by many factors, such as the patient’s clinical condition, coagulation status, the position and patency of the vascular access and catheter size, the choice of anticoagulant, CRRT modality, and filtration fraction.5,31,32,47 In our study, Cox regression did not yield evidence to support the literature in a number of factors, including patient weight (< 10 kg), filter size, catheter location, pump flow rate and the half-life of the clotted hemofilter. We found that the risk of hemofilter clotting was 3.3-fold higher with systemic heparin compared to citrate. This result was in support of our previously mentioned data and we can conclude that citrate can improve CS by reducing the likelihood of clotting. Therefore we can conclude that RCA is an efficient method in critically in children under CRRT with respect to progress of treatment.
The potential advantage of RCA for CRRT is that it may reduce the occurrence of systemic adverse events. The reported bleeding incidences associated with systemic heparin use in CRRT ranges from 10% to 50%, with bleeding mortality rates as high as 15%.12,35,48 In addition to various adult studies and meta-analyses, pediatric studies have also shown that RCA use in CRRT reduces bleeding risk by more than half compared to systemic heparin use.4,6,7,35,39,41 However, the effect of RCA in reducing the need for transfusion compared to systemic heparin use is controversial.35 This may be explained by the direct shutdown of systemic heparin in case of bleeding complications. However, discontinuation or interruption of heparin anticoagulation may increase the risk of clotting, leading to interruption of CRRT treatment and treatment failure. As opposed to previously reported results, we found that severe bleeding episodes were less frequent among RCA recipients (18.4% vs. 10.9%), albeit without statistical significance. Moreover, the need for red blood cell transfusions was higher in systemic heparin recipients compared to RCA, but again significance was not achieved. However, the frequency of blood transfusion requirement after circuit clotting (relative to all-cause transfusions) was significantly higher (42.5% vs 12.55%) among those who received systemic heparinization compared to RCA. In the pediatric study by Rico et al, it was observed that the use of RCA did not achieve a significant decrease in the incidence of serious bleeding events, but all bleeding events in the heparin group were systemic (gastrointestinal, central nervous system, intraabdominal) bleeding, whereas in the RCA group, up to 30% were local events (high flow catheter insertion site).38 In addition to prolonging filter life, RCA use may reduce filter clotting-related blood transfusions. This property might be crucial for small infants and may contribute to the reduction of costs and blood transfusions.
Since the main site of citrate metabolism is the liver, patients with hepatic failure and neonatal and small infants with immature liver function are risky groups for CA.20 In our study, we did not apply RCA in patients with hepatic failure because of concerns about citrate metabolism. However, in recent years, there are studies showing that it can be used safely in pediatric cases with hepatic failure and neonatal cases, but with strict monitoring.20,41,49 In a series of 50 cases including neonatal patients by Cappoli et al. it was reported that clinical findings of CA were observed in only 6 patients, all of whom had a calcium index of > 2.5. It is interesting that none of these 6 patients had liver failure.40 Rodriguez et al. reported that 70% of pediatric patients with liver failure experienced at least one episode of CA, but RCA had to be interrupted in only two such cases.20 In some pediatric studies, CA was not observed in any of the patients.19,22,36,39 In our study, CA was observed in 4 (3.5%) of 115 CRRT sessions with RCA. In adult studies, CA episodes have been reported at much lower rates (0%–0.7%) compared to pediatric studies.6,35 Since routine measurement of blood citrate level is not possible in practice, it should be kept in mind that CA can be estimated indirectly by totCa++ / iCa++ ratio ( > 2.5 mmol/L). In the present study, the definition of CA was based on an elevated totCa++ / iCal++ ratio accompanied by metabolic acidosis with high anion gap. However, in some studies, the totCa++ to iCal++ ratio of > 2.5 was accepted to establish CA diagnosis. However, the direct relationship between high totCa++ / iCa++ ratio and metabolic complications is controversial.38
The increased risk of CA in children undergoing RCA compared to adult patients may be explained by two factors. First, citrate infusions are often administered at much higher rates as compared to adults (on a mg per kg basis). This is because citrate infusion rates are based on blood flow and not patient weight. As discussed earlier, blood flow rates, especially in small children, are disproportionately high compared to adults when calculated in mL/min/kg, and therefore, citrate infusion rates must be increased to accommodate this difference.7,50 Second, lower citrate clearance rates have been reported in CRRT, compared to intermittent hemodialysis, and the rates are even lower when this therapy is used in children. In adults, clearance rates of 35–50% have been reported, compared with rates of only 20% in pediatric patients.18 In infants, strategies such as using lower concentrations of citrate (< 2.5 mmol/L) and targeting higher filter ionized calcium levels (< 0.5 mmol) and maintaining blood flow below a certain threshold (< 50 mL/min) can be used to reduce the risk of CA.15,21,38 In our study, none of the metabolic complications analyzed (including CA) were found to be associated with citrate dose or patient weight. We infer that the population could have other risk factors (metabolic capacity etc.) and/or triggers for complications apart from citrate use. All four episodes of CA were managed with conservative methods (such as decreasing blood flow rate, decreasing citrate flow rate, increasing dialysate rate) without altering the anticoagulation method.
The use of RCA is associated with metabolic complications, including possible life-threatening systemic hypocalcemia and metabolic alkalosis. Citrate is metabolized mainly in the liver into three moles of bicarbonate. Exposure to excessive citrate results in metabolic alkalosis in cases with sufficient liver metabolic capacity. This can be addressed by administering 0.9% sodium chloride infusion as pre- or post-replacement fluid, in addition to the conservative methods used for CA.29,33,39 Hypocalcemia, one of the most dangerous metabolic complications associated with RCA, occurs through two mechanisms. The first is the elevation of dialyzable calcium fraction due to the citrate-calcium complex. The second is the continuous binding of calcium by free citrate efflux, as the citrate clearance applied before the filter remains at the level of 35–50%.51
Frequency of these metabolic complications is variable and heterogeneous in both adult and pediatric studies.6,18 Similarly, the reported frequency of metabolic complications associated with the use of RCA is variable in both adult and pediatric population studies. In a meta-analysis, it was reported that hypocalcemia was 3.9 times more common with RCA, but no adverse events related to hypocalcemia were observed. Also, no significant difference was observed in the frequency of metabolic alkalosis.11 Zarbock et al. reported that RCA use did not pose a risk for the development of severe hypocalcemia (1.4% vs 0.3%), but increased the frequency of severe alkalosis (2.4% vs 0.3%) in adults.35 In pediatric studies, there is a wide range of reported frequencies for both metabolic alkalosis (2.0% to 86.5%) and hypocalcemia (0% to 60%) with RCA.19,22,36,38,40,50 In our study, hypocalcemia (35.7%) and metabolic alkalosis (33%) were significantly more common in RCA recipients compared to heparin recipients (15.2% vs. 19.4%, respectively).
These complications were diagnosed early by close monitoring of acid base status and calcium level, and were managed with conservative methods mentioned above. Thus, metabolic complications in patients treated with RCA should not be considered as a drawback, since they are mild and easily resolved. An important strategy to reduce metabolic complications associated with RCA is to reduce citrate exposure by lowering citrate infusion rate and dosage.52,53,54 Poh et al reported that applying a citrate protocol at a dose of 2.5 mmol/L reduced citrate-related metabolic complications without causing a decrease in anticoagulation effectiveness compared to 3 mmol/L.54
In the literature, the mortality rate in pediatric CRRT patients undergoing RCA varies between 16.7% and 50%, and in the majority of studies, no significant relationship has been found between anticoagulation choice and mortality.9,39,40,49 Overall mortality in our study was 28.2% and frequencies were similar in the two groups.
This study has several limitations. First, this is a single-center retrospective study. Second, we did not use RCA in patients with hepatic failure due to concerns regarding contraindication. Therefore, the systemic heparin and citrate groups are biased in this regard, potentially distorting findings. Third, patients from the 2015–2017 periods received standard anticoagulation with systemic heparin, because citrate was not used at our center before 2017. In March 2017, we started treating patients with RCA, and therefore, we cannot rule out a bias in this regard or an effect of increasing experience with CRRT. In addition, the sample size is smaller relative to adult studies which may subject the analyses to statistical bias; however, to our knowledge, this study has one of the largest sample sizes and longest CRRT duration (total hours) among pediatric CRRT studies comparing the efficacy and safety of these two anticoagulation methods.
Our data demonstrate that RCA could be more effective than systemic heparin for prolongation of CS during CRRT in critically-ill children. It appears to prolong CS with a lower incidence of clotting and blood transfusion after circuit clotting. We did not find any serious side effects of RCA, indicating that the efficacy is complemented by safety in pediatric CRRT. Notably, RCA may cause minimal metabolic and ionic imbalances which can be easily resolved. Further prospective studies are needed to assess the safety and efficacy of RCA in this population.
Data availability
Data included in this manuscript are available upon request by contacting with the corresponding author and will be freely available to any researcher wishing to use them for non-commercial purposes, without breaching participant confidentiality.
References
Sethi, S. K., Bunchman, T., Raina, R. & Kher, V. Unique considerations in renal replacement therapy in children: core curriculum 2014. Am. J. Kidney Dis. 63, 329–345 (2014).
Garzotto, F., Zanella, M. & Ronco, C. The evolution of pediatric continuous renal replacement therapy. Nephron. Clin. Pract. 127, 172–175 (2014).
Joannidis, M. & Oudemans-Van Straaten, H. M. Clinical review: Patency of the circuit in continuous renal replacement therapy. Crit. Care. 11, 218 (2007).
Zhang, Z. & Hongying, N. Efficacy and safety of regional citrate anticoagulation in critically ill patients undergoing continuous renal replacement therapy. Intensive Care Med. 38, 20–28 (2012).
Del Castillo, J. et al. Circuit life span in critically ill children on continuous renal replacement treatment: a prospective observational evaluation study. Crit. Care. 12, R93 (2008).
Wu, M. Y. et al. Regional citrate versus heparin anticoagulation for continuous renal replacement therapy: a meta-analysis of randomized controlled trials. Am. J. Kidney Dis. 59, 810–818 (2012).
Davis, T. K., Neumayr, T., Geile, K., Doctor, A. & Hmeil, P. Citrate anticoagulation during continuous renal replacement therapy in pediatric critical care. Pediatr. Crit. Care Med. 15, 471–485 (2014).
Mehta, R. L., McDonald, B. R., Aguilar, M. M. & Ward, D. M. Regional citrate anticoagulation for continuous arteriovenous hemodialysis in critically ill patients. Kidney Int. 38, 976–981 (1990).
Buccione, E. et al. Regional Citrate Anticoagulation and Systemic Anticoagulation during Pediatric Continuous Renal Replacement Therapy: A Systematic Literature Review. J. Clin. Med. 11, 3121 (2022).
Group KDIGOGW. KDIGO clinical practice guideline for glomerulonephritis. Kidney Int. Suppl. 2, 139–274 (2012).
Liu, C., Mao, Z., Kang, H., Hu, J. & Zhou, F. Regional citrate versus heparin anticoagulation for continuous renal replacement therapy in critically ill patients: a meta-analysis with trial sequential analysis of randomized controlled trials. Crit. Care. 20, 144 (2016).
Bai, M. et al. Citrate versus heparin anticoagulation for continuous renal replacement therapy: an updated meta-analysis of RCTs. Intensive Care Med. 41, 2098–2110 (2015).
Meersch, M. et al. Regional citrate versus systemic heparin anticoagulation for continuous renal replacement therapy in critically ill patients with acute kidney injury (RICH) trial: study protocol for a multicentre, randomised controlled trial. BMJ Open 9, e024411 (2019).
Bunchman, T. E., Maxvold, N. J. & Brophy, P. D. Pediatric convective hemofiltration: Normocarb replacement fluid and citrate anticoagulation. Am. J. Kidney Dis. 42, 1248–1252 (2003).
Liet, J. M. et al. Regional citrate anticoagulation for pediatric CRRT using integrated citrate software and physiological sodium concentration solutions. Pediatr. Nephrol. 29, 1625–1631 (2014).
Persic, V. et al. Regional citrate anticoagulation for continuous renal replacement therapy in newborns and infants: Focus on citrate accumulation. Artif. Organs 44, 497–503 (2020).
Elhanan, N., Skippen, P., Nuthall, G., Krahn, G. & Seear, M. Citrate anticoagulation in pediatric continuous venovenous hemofiltration. Pediatr. Nephrol. 19, 208–212 (2004).
Chadha, V., Garg, U., Warady, B. A. & Alon, U. S. Citrate clearance in children receiving continuous venovenous renal replacement therapy. Pediatr. Nephrol. 17, 819–824 (2002).
Fernández, S. N. et al. Citrate anticoagulation for CRRT in children: comparison with heparin. Biomed. Res. Int. 2014, 786301 (2014).
Rodriguez, K. et al. Regional citrate anticoagulation for continuous renal replacement therapy in pediatric patients with liver failure. PLoS One 12, e0182134 (2017).
Musielak, A. et al. Outcomes of Continuous Renal Replacement Therapy With Regional Citrate Anticoagulation in Small Children After Cardiac Surgery: Experience and Protocol From a Single Center. Ther. Apher. Dial. 20, 639–644 (2016).
Raymakers-Janssen, P. et al. Citrate versus heparin anticoagulation in continuous renal replacement therapy in small children. Pediatr. Nephrol. 32, 1971–1978 (2017).
Kenet, G., Strauss, T., Kaplinsky, C. & Paret, G. Hemostasis and thrombosis in critically ill children. Semin Thromb. Hemost. 34, 451–458 (2008).
Bateman, S. T. et al. Anemia, blood loss, and blood transfusions in North American children in the intensive care unit. Am. J. Respir. Crit. Care Med. 178, 26–33 (2008).
Sutherland, S. M. et al. Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am. J. Kidney Dis. 55, 316–325 (2010).
Foland, J. A. et al. Fluid overload before continuous hemofiltration and survival in critically ill children: a retrospective analysis. Crit. Care Med. 32, 1771–1776 (2004).
Cortina, G. et al. Mortality of Critically Ill Children Requiring Continuous Renal Replacement Therapy: Effect of Fluid Overload, Underlying Disease, and Timing of Initiation. Pediatr. Crit. Care Med. 20, 314–322 (2019).
Goldstein, B., Giroir, B. & Randolph, A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr. Crit. Care Med. 6, 2–8 (2005).
Schneider, A. G., Journois, D. & Rimmelé, T. Complications of regional citrate anticoagulation: accumulation or overload? Crit. Care. 21, 281 (2017).
Valentine, S. L. et al. Consensus Recommendations for RBC Transfusion Practice in Critically Ill Children From the Pediatric Critical Care Transfusion and Anemia Expertise Initiative. Pediatr. Crit. Care Med. 19, 884–898 (2018).
Buccione, E. et al. Continuous Renal Replacement Therapy in Critically Ill Children in the Pediatric Intensive Care Unit: A Retrospective Analysis of Real-Life Prescriptions, Complications, and Outcomes. Front. Pediatr. 9, 696798 (2021).
Baldwin, I. Factors affecting circuit patency and filter ‘life’. Contrib. Nephrol. 156, 178–184 (2007).
Davenport, A. & Tolwani, A. Citrate anticoagulation for continuous renal replacement therapy (CRRT) in patients with acute kidney injury admitted to the intensive care unit. NDT 6, 439–447 (2009).
Betjes, M. G., Van Oosterom, D., Van Agteren, M. & Van De Wetering, J. Regional citrate versus heparin anticoagulation during venovenous hemofiltration in patients at low risk for bleeding: similar hemofilter survival but significantly less bleeding. J. Nephrol. 20, 602–608 (2007).
Zarbock, A. et al. Effect of Regional Citrate Anticoagulation vs Systemic Heparin Anticoagulation During Continuous Kidney Replacement Therapy on Dialysis Filter Life Span and Mortality Among Critically Ill Patients With Acute Kidney Injury: A Randomized Clinical Trial. JAMA 324, 1629–1639 (2020).
Sık, G., Demirbuga, A., Annayev, A. & Citak, A. Regional citrate versus systemic heparin anticoagulation for continuous renal replacement therapy in critically ill children. Int. J. Artif. Organs 43, 234–241 (2020).
Askenazi, D. J. et al. Continuous renal replacement therapy for children ≤10 kg: a report from the prospective pediatric continuous renal replacement therapy registry. J. Pediatr. 162, 587–592.e583 (2013).
Rico, M. P. et al. Regional citrate anticoagulation for continuous renal replacement therapy in children. Pediatr. Nephrol. 32, 703–711 (2017).
Zaoral, T., Hladík, M., Zapletalová, J., Trávníček, B. & Gelnarová, E. Circuit Lifetime With Citrate Versus Heparin in Pediatric Continuous Venovenous Hemodialysis. Pediatr. Crit. Care Med. 17, e399–e405 (2016).
Cappoli, A. et al. A simplified protocol of regional citrate anticoagulation with phosphate-containing solutions in infants and children treated with continuous kidney replacement therapy. Pediatr. Nephrol. 38, 3835–3844 (2023).
Brophy, P. D. et al. Multi-centre evaluation of anticoagulation in patients receiving continuous renal replacement therapy (CRRT). Nephrol. Dial. Transplant. 20, 1416–1421 (2005).
Rodl, S. et al. One-year safe use of the Prismaflex HF20 (R) disposable set in infants in 220 renal replacement treatment sessions. Intensive Care Med 37, 884–885 (2011).
Ronco, C. et al. Continuous renal replacement therapy in neonates and small infants: development and first-in-human use of a miniaturised machine (CARPEDIEM). Lancet 383, 1807–1813 (2014).
Köstekci, Y. E. et al. Evaluation of the efficacy and associated complications of regional citrate anticoagulation in neonates: experience from a fourth level neonatal intensive care unit. Eur. J. Pediatr. 182, 4897–4908 (2023).
Soltysiak, J. et al. Citrate anticoagulation for continuous renal replacement therapy in small children. Pediatr. Nephrol. 29, 469–475 (2014).
Cortina, G., Daverio, M., Demirkol, D., Chanchlani, R. & Deep, A. Continuous renal replacement therapy in neonates and children: what does the pediatrician need to know? An overview from the Critical Care Nephrology Section of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC). Eur. J. Pediatr. 183, 529–541 (2024).
Miklaszewska, M. et al. Filter Size Not the Anticoagulation Method is the Decisive Factor in Continuous Renal Replacement Therapy Circuit Survival. Kidney Blood Press Res 42, 327–337 (2017).
Martin, P. Y., Chevrolet, J. C., Suter, P. & Favre, H. Anticoagulation in patients treated by continuous venovenous hemofiltration: a retrospective study. Am. J. Kidney Dis. 24, 806–812 (1994).
Huang, H. et al. Regional citrate anticoagulation for continuous renal replacement therapy in newborns. Front Pediatr. 11, 1089849 (2023).
Liet, J. M. et al. Semiautomated Regional Citrate Anticoagulation for Continuous Kidney Replacement Therapy: An Observational Study in Young Children. Pediatr. Crit. Care Med. 23, e429–e433 (2022).
Kozik-Jaromin, J., Nier, V., Heemann, U., Kreymann, B. & Böhler, J. Citrate pharmacokinetics and calcium levels during high-flux dialysis with regional citrate anticoagulation. Nephrol. Dial. Transplant. 24, 2244–2251 (2009).
Jacobs, R. et al. Regional Citrate Anticoagulation in Continuous Renal Replacement Therapy: Is Metabolic Fear the Enemy of Logic? A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Life (Basel) 17, 1198 (2023).
Tolwani, A. J., Campbell, R. C., Schenk, M. B., Allon, M. & Warnock, D. G. Simplified citrate anticoagulation for continuous renal replacement therapy. Kidney Int. 60, 370–374 (2001).
Poh, C. B. et al. Regional Citrate Anticoagulation for Continuous Renal Replacement Therapy - A Safe and Effective Low-Dose Protocol. Nephrol. (Carlton) 25, 305–313 (2020).
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Author information
Authors and Affiliations
Contributions
S.K.A., M.D., and Z.K. participated in analyzing data and wrote the manuscript. S.K.A. collected clinical samples and information. S.K.A., M.D., Z.K., A.Y., revised the manuscript for important intellectual content. S.K.A., M.D, and A.Y., coordinated the study over the entire time. All authors reviewed the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by Clinical Ethics Committee of Istanbul Medeniyet University Goztepe Training and Research Hospital (Decision date: 13.01.2021, decision no: 2021/0017). Patient consent was waived due to the retrospective nature of the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Atis, S.K., Duyu, M., Karakaya, Z. et al. Citrate anticoagulation and systemic heparin anticoagulation during continuous renal replacement therapy among critically-ill children. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03163-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03163-x