Abstract
Background
Mortality and intraventricular hemorrhage (IVH) are common adverse outcomes in preterm infants and are challenging to predict clinically. Sample entropy (SE), a measure of heart rate variability (HRV), has shown predictive power for sepsis and other morbidities in neonates. We evaluated associations between SE and mortality and IVH in the first week of life.
Methods
Participants were 389 infants born before 32 weeks of gestation for whom bedside monitor data were available. A total of 29 infants had IVH grade 3 or 4 and 31 infants died within 2 weeks of life. SE was calculated with the PhysioNet open-source benchmark. Logistic regressions assessed associations between SE and IVH and/or mortality with and without common clinical covariates over various hour of life (HOL) censor points.
Results
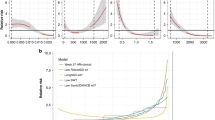
Lower SE was associated with mortality by 4 HOL, but higher SE was very strongly associated with IVH and mortality at 24–96 HOL. Bootstrap testing confirmed SE significantly improved prediction using clinical variables at 96 HOL.
Conclusion
SE is a significant predictor of IVH and mortality in premature infants. Given IVH typically occurs in the first 24–72 HOL, affected infants may initially have low SE followed by a sustained period of high SE.
Impact
-
SE correlates with IVH and mortality in preterm infants early in life.
-
SE combined with clinical factors yielded ROC AUCs well above 0.8 and significantly outperformed the clinical model at 96 h of life. Previous studies had not shown predictive power over clinical models.
-
First study using the PhysioNet Cardiovascular Toolbox benchmark in young infants.
-
Relative to the generally accepted timing of IVH in premature infants, we saw lower SE before or around the time of hemorrhage and a sustained period of higher SE after. Higher SE after acute events has not been reported previously.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Martin, J. A., Hamilton, B. E., Osterman, M. J. K., Driscoll, A. K. & Mathews, T. J. Births: Final Data for 2015. Natl. Vital-. Stat. Rep. Cent. Dis. Control Prev. Natl. Cent. Health Stat. Natl. Vital-. Stat. Syst. 66, 1 (2017).
Blencowe, H. et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet Lond. Engl. 379, 2162–2172 (2012).
Patel, R. M. Short- and long-term outcomes for extremely preterm infants. Am. J. Perinatol. 33, 318–328 (2016).
Walsh, M. C. et al. Neonatal outcomes of moderately preterm infants compared to extremely preterm infants. Pediatr. Res. 82, 297–304 (2017).
Ward, R. M. & Beachy, J. C. Neonatal complications following preterm birth. BJOG Int. J. Obstet. Gynaecol. 110, 8–16 (2003).
Stoll, B. J. et al. Trends in Care Practices, Morbidity, and Mortality of Extremely Preterm Neonates, 1993-2012. JAMA 314, 1039 (2015).
Inder T. E., Perlman J. M., Volpe J. J. Preterm Intraventricular Hemorrhage/Posthemorrhagic Hydrocephalus [Internet]. In Volpe’s Neurology of the Newborn 637–698.e21 (Elsevier, 2018 [cited 2023 May]) Available from: https://linkinghub.elsevier.com/retrieve/pii/B9780323428767000247
Inder, T. E., Warfield, S. K., Wang, H., Hüppi, P. S. & Volpe, J. J. Abnormal cerebral structure is present at term in premature infants. Pediatrics 115, 286–294 (2005).
Lazzara, A., Ahmann, P., Dykes, F., Brann, A. W. & Schwartz, J. Clinical Predictability of Intraventricular Hemorrhage in Preterm Infants. Pediatrics 65, 30–34 (1980).
Blackburn S. Assessment and management of neurologic dysfunction. In Comprehensive Neonatal Nursing. A Physiologic Perspective (Kenner C., Lott J., & Flandermeyer A., eds) 564-607 (WB Saunders Company, Philadelphia, PA, 1998)
van Ravenswaaij-Arts, C. M., Kollée, L. A., Hopman, J. C., Stoelinga, G. B. & van Geijn, H. P. Heart rate variability. Ann. Intern. Med. 118, 436–447 (1993).
Griffin, M. P., Lake, D. E., O’Shea, T. M. & Moorman, J. R. Heart rate characteristics and clinical signs in neonatal sepsis. Pediatr. Res. 61, 222–227 (2007).
Griffin, M. P. et al. Abnormal heart rate characteristics are associated with neonatal mortality. Pediatr. Res. 55, 782–788 (2004).
Chien, L.-Y. et al. Snap-II predicts severe intraventricular hemorrhage and chronic lung disease in the neonatal intensive care unit. J. Perinatol. J. Calif. Perinat. Assoc. 22, 26–30 (2002).
Singh, R. et al. A predictive model for SIVH risk in preterm infants and targeted indomethacin therapy for prevention. Sci. Rep. 3, 2539 (2013).
Luque, M. J. et al. A risk prediction model for severe intraventricular hemorrhage in very low birth weight infants and the effect of prophylactic indomethacin. J. Perinatol. 34, 43–48 (2014).
Siddappa, A. M., Quiggle, G. M., Lock, E. & Rao, R. B. Predictors of severe intraventricular hemorrhage in preterm infants under 29-weeks gestation. J. Matern. Fetal Neonatal. Med. 34, 195–200 (2021).
Perlman, J. M., McMenamin, J. B. & Volpe, J. J. Fluctuating cerebral blood-flow velocity in respiratory-distress syndrome: relation to the development of intraventricular hemorrhage. N. Engl. J. Med. 309, 204–209 (1983).
Bel, F., Bor, M., Stijnen, T., Baan, J. & Ruys, J. H. Aetiological role of cerebral blood-flow alterations in development and extension of peri-intraventricular haemorrhage. Dev. Med. Child Neurol. 29, 601–614 (2008).
Noori, S., McCoy, M., Anderson, M. P., Ramji, F. & Seri, I. Changes in cardiac function and cerebral blood flow in relation to peri/intraventricular hemorrhage in extremely preterm infants. J. Pediatr. 164, 264–270.e3 (2014).
Hanna, B. D. et al. Heart rate variability in preterm brain-injured and very-low-birth-weight infants. Biol. Neonate 77, 147–155 (2000).
Tuzcu, V., Nas, S., Ulusar, U., Ugur, A. & Kaiser, J. R. Altered heart rhythm dynamics in very low birth weight infants with impending intraventricular hemorrhage. Pediatrics 123, 810–815 (2009).
Addison, K., Griffin, M. P., Moorman, J. R., Lake, D. E. & O’Shea, T. M. Heart rate characteristics and neurodevelopmental outcome in very low birth weight infants. J. Perinatol. 29, 750–756 (2009).
Fairchild, K. D. et al. Abnormal heart rate characteristics are associated with abnormal neuroimaging and outcomes in extremely low birth weight infants. J. Perinatol. 34, 375–379 (2014).
Sullivan, B. A. et al. Early heart rate characteristics predict death and morbidities in preterm infants. J. Pediatr. 174, 57–62 (2016).
Al-Abdi, S. Y. & Al-Aamri, M. A. A systematic review and meta-analysis of the timing of early intraventricular hemorrhage in preterm neonates: clinical and research implications. J. Clin. Neonatol. 3, 76–88 (2014).
Richman, J. S. & Moorman, J. R. Physiological time-series analysis using approximate entropy and sample entropy. Am. J. Physiol. Heart Circ. Physiol. 278, H2039–H2049 (2000).
Moorman, J. R. et al. Cardiovascular oscillations at the bedside: early diagnosis of neonatal sepsis using heart rate characteristics monitoring. Physiol. Meas. 32, 1821–1832 (2011).
Takatani, T. et al. Relationship between frequency spectrum of heart rate variability and autonomic nervous activities during sleep in newborns. Brain Dev. 40, 165–171 (2018).
Delgado-Bonal, A. & Marshak, A. Approximate entropy and sample entropy: a comprehensive tutorial. Entropy Basel Switz. 21, 541 (2019).
Vest, A. N. et al. An open source benchmarked toolbox for cardiovascular waveform and interval analysis. Physiol. Meas. 39, 105004 (2018).
Papile, L. A., Burstein, J., Burstein, R. & Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J. Pediatr. 92, 529–534 (1978).
Bohlin, K., Gudmundsdottir, T., Katz-Salamon, M., Jonsson, B. & Blennow, M. Implementation of surfactant treatment during continuous positive airway pressure. J. Perinatol. J. Calif. Perinat. Assoc. 27, 422–427 (2007).
Miller, D. R., Dhillon, G. S., Bambos, N., Shin, A. Y. & Scheinker, D. WAVES - The Lucile Packard Children’s Hospital pediatric physiological waveforms dataset. Sci. Data 10, 124 (2023).
Lake, D. E., Richman, J. S., Griffin, M. P. & Moorman, J. R. Sample entropy analysis of neonatal heart rate variability. Am. J. Physiol. Regul. Integr. Comp. Physiol. 283, R789–R797 (2002).
Hastie T., Tibshirani R., Friedman J. The Elements of Statistical Learning. (Springer, New York, NY, 2009)
James G., Witten D., Hastie T., Tibshirani R. An Introduction to Statistical Learning: with Applications in R. (Springer, New York, NY, 2021)
Stålhammar, A. M. et al. Weight a minute: The smaller and more immature, the more predictable the autonomic regulation? Acta Paediatr. Oslo Nor. 112, 1443–1452 (2023).
Ribeiro, M. et al. Evolution of heart rate complexity indices in the early detection of neonatal sepsis. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. IEEE Eng. Med. Biol. Soc. Annu. Int. Conf. 2022, 367–372 (2022).
Jost, K., Datta, A. N., Frey, U. P., Suki, B. & Schulzke, S. M. Heart rate fluctuation after birth predicts subsequent cardiorespiratory stability in preterm infants. Pediatr. Res. 86, 348–354 (2019).
Beuchée, A. et al. Uncorrelated randomness of the heart rate is associated with sepsis in sick premature infants. Neonatology 96, 109–114 (2009).
Lake, D. E., Fairchild, K. D. & Moorman, J. R. Complex signals bioinformatics: evaluation of heart rate characteristics monitoring as a novel risk marker for neonatal sepsis. J. Clin. Monit. Comput. 28, 329–339 (2014).
Kovatchev, B. P. et al. Sample asymmetry analysis of heart rate characteristics with application to neonatal sepsis and systemic inflammatory response syndrome. Pediatr. Res. 54, 892–898 (2003).
Rudolph, A. J., Vallbona, C. & Desmond, M. M. Cardiodynamic Studies in the Newborn: III. Heart Rate Patterns in Infants with Idiopathic Respiratory Distress Syndrome. Pediatrics 36, 551–559 (1965).
Alonzo, C. J. & Fairchild, K. D. Dexamethasone effect on heart rate variability in preterm infants on mechanical ventilation. J. Neonatal. Perinat. Med. 10, 425–430 (2017).
Doyle, L. W., Ehrenkranz, R. A. & Halliday, H. L. Early (< 8 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database Syst. Rev. 5, 1146 (2014).
Renolleau, C. et al. Association between Baseline Cortisol Serum Concentrations and the Effect of Prophylactic Hydrocortisone in Extremely Preterm Infants. J. Pediatr. 234, 65–70 (2021).
Griffin, M. P. & Moorman, J. R. Toward the early diagnosis of neonatal sepsis and sepsis-like illness using novel heart rate analysis. Pediatrics 107, 97–104 (2001).
Babyak M. A. What You See May Not Be What You Get: A Brief, Nontechnical Introduction to Overfitting in Regression-Type Models. Psychosom. Med. [Internet] 66, 411-421 (2004). Available from: https://journals.lww.com/psychosomaticmedicine/Fulltext/2004/05000/What_You_See_May_Not_Be_What_You_Get__A_Brief,.21.aspx.
Hawkins, D. M. The problem of overfitting. J. Chem. Inf. Comput. Sci. 44, 1–12 (2004).
Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur. Heart J. 17, 354–381 (1996).
Valderrama, C. E., Marzbanrad, F., Hall-Clifford, R., Rohloff, P. & Clifford, G. D. A Proxy for Detecting IUGR Based on Gestational Age Estimation in a Guatemalan Rural Population. Front. Artif. Intell. 3, 56 (2020).
Magawa, S. et al. Fetal heart rate variability is a biomarker of rapid but not progressive exacerbation of inflammation in preterm fetal sheep. Sci. Rep. 12, 1771 (2022).
Henriques, T. et al. Nonlinear Methods Most Applied to Heart-Rate Time Series: A Review. Entropy Basel Switz. 22, 309 (2020).
Ribeiro, M. et al. The Entropy Universe. Entropy Basel Switz. 23, 222 (2021).
Acknowledgements
This research used data or services provided by STARR, “STAnford medicine Research data Repository,” a clinical data warehouse containing live Epic data from Stanford Health Care, the Stanford Children’s Hospital, the University Healthcare Alliance and Packard Children’s Health Alliance clinics and other auxiliary data from Hospital applications such as radiology PACS. STARR platform is developed and operated by the Stanford Medicine Research Technology team and is made possible by the Stanford School of Medicine Research Office. This work was supported by a grant from the Stanford Maternal & Child Health Research Institute (MCHRI, https://med.stanford.edu/mchri.html) with Melissa Scala as the principal investigator. Additional support included a faculty scholar award from MCHRI and resources generated from NIH/NICHD (R00 HD084749-01A1) to Katherine Travis (PI).
Author information
Authors and Affiliations
Contributions
M.D.S., V.C., K.T. and M.S. were responsible for the study design. M.D.S. and M.S. were responsible for the literature search and manuscript drafting. All authors were responsible for the critical revision of the manuscript, contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
E.H. is a full-time employee of Philips Healthcare and owns stock in the company. M.D.S., V.C., K.T., M.L., and M.S. declare no competing interests.
Ethical approval
The Stanford University Institutional Review Board approved this study (protocol number 50602). All data were gathered in the course of routine clinical care and anonymized, and so no specific consent was indicated.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Scahill, M.D., Chock, V., Travis, K. et al. Sample entropy correlates with intraventricular hemorrhage and mortality in premature infants early in life. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03075-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03075-w
This article is cited by
-
Monitoring chaos at the cot-side
Pediatric Research (2024)