Abstract
Background
Neonatal sepsis remains a leading cause of mortality in neonatal units. Neonatologist-performed echocardiography (NPE) offers the potential for early detection of sepsis-associated cardiovascular dysfunction. This review examines available echocardiographic findings in septic neonates.
Methods
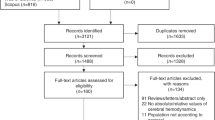
Following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, we systematically reviewed prospective observational, cross-sectional, case control, and cohort studies on septic newborns with echocardiographic assessments from PubMed, Scopus and Embase. Quality assessment employed the Newcastle–Ottawa Scale, with results analyzed descriptively.
Results
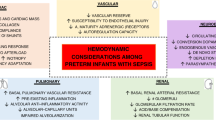
From an initial pool of 1663 papers, 12 studies met inclusion criteria after relevance screening and eliminating duplicates/excluded studies. The review encompassed 438 septic newborns and 232 controls. Septic neonates exhibited either increased risk of pulmonary hypertension or left ventricular diastolic dysfunction, and a warm shock physiology characterized by higher cardiac outputs.
Discussion
The included studies exhibited heterogeneity in sepsis definitions, sepsis severity scores, echocardiographic evaluations, and demographic data of newborns. Limited sample sizes compromised analytical interpretability. Nonetheless, this work establishes a foundation for future high-quality echocardiographic studies.
Conclusion
Our review confirms that septic neonates show significant hemodynamic changes that can be identified using NPE. These findings underscore the need for wider NPE use to tailor hemodynamics-based strategies within this population.
Impact
-
1.
Our study emphasizes the value of neonatologist-performed echocardiography (NPE) as a feasible tool for identifying significant hemodynamic changes in septic neonates.
-
2.
Our study underscores the importance of standardized echocardiographic protocols and frequent monitoring of cardiac function in septic neonates.
-
3.
The impact of the study lies in its potential to increase researchers’ awareness for the need for more high-quality echocardiographic data in future studies. By promoting wider use of NPE, neonatologists can more accurately assess the hemodynamic status of septic newborns and tailor treatment approaches, potentially improving patient outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Jacob, J., Kamitsuka, M., Clark, R. H., Kelleher, A. S. & Spitzer, A. R. Etiologies of NICU deaths. Pediatrics 135, e59–e65 (2015).
Raj, S., Killinger, J. S., Gonzalez, J. A. & Lopez, L. Myocardial dysfunction in pediatric septic shock. J. Pediatr. 164, 72–77.e2 (2014).
Weiss, S. L. et al. The epidemiology of hospital death following pediatric severe sepsis: when, why, and how children with sepsis die*. Pediatr. Crit. Care Med. 18, 823–830 (2017).
Schmatz, M. et al. Surviving sepsis in a referral neonatal intensive care unit: association between time to antibiotic administration and in-hospital outcomes. J. Pediatr. 217, 59–65.e1 (2020).
Kharrat, A. & Jain, A. Hemodynamic dysfunction in neonatal sepsis. Pediatr. Res. 91, 413–424 (2022).
Ince, C. et al. The endothelium in sepsis. Shock 45, 259–270 (2016).
Knuefermann, P. et al. Bacterial DNA induces myocardial inflammation and reduces cardiomyocyte contractility: role of Toll-like receptor 9. Cardiovasc. Res. 78, 26–35 (2008).
Virág, M., Leiner, T., Rottler, M., Ocskay, K. & Molnar, Z. Individualized hemodynamic management in sepsis. J. Pers. Med. 11, 157 (2021).
Cuenca, J., Martín-Sanz, P., Álvarez-Barrientos, A. M., Boscá, L. & Goren, N. Infiltration of inflammatory cells plays an important role in matrix metalloproteinase expression and activation in the heart during sepsis. Am. J. Pathol. 169, 1567–1576 (2006).
Frayn, K. N. Hormonal control of metabolism in trauma and sepsis. Clin. Endocrinol. 24, 577–599 (1986).
Aradhya, A. S. et al. Low vasopressin and progression of neonatal sepsis to septic shock: a prospective cohort study. Eur. J. Pediatr. 179, 1147–1155 (2020).
Khashana, A., Ojaniemi, M., Leskinen, M., Saarela, T. & Hallman, M. Term neonates with infection and shock display high cortisol precursors despite low levels of normal cortisol. Acta Paediatr. 105, 154–158 (2016).
Ni, M. et al. Use of vasopressin in neonatal intensive care unit patients with hypotension. J. Pediatr. Pharmacol. Ther. 22, 430–435 (2017).
LeFlore, J. L. & Engle, W. D. Capillary refill time is an unreliable indicator of cardiovascular status in term neonates. Adv. Neonatal Care 5, 147–154 (2005).
Takci, S., Yigit, S., Korkmaz, A. & Yurdakök, M. Comparison between oscillometric and invasive blood pressure measurements in critically ill premature infants. Acta Paediatr. 101, 132–135 (2012).
Zonnenberg, I. A., van Dijk, J., van den Dungen, F. A. M., Vermeulen, R. J. & van Weissenbruch, M. M. The prognostic value of NIRS in preterm infants with (suspected) late-onset sepsis in relation to long term outcome: a pilot study. PLoS ONE 14, e0220044 (2019).
de Boode, W. P. et al. The role of Neonatologist Performed Echocardiography in the assessment and management of neonatal shock. Pediatr. Res. 84, 57–67 (2018).
Groves, A. M. et al. Introduction to neonatologist-performed echocardiography. Pediatr. Res. 84, 1–12 (2018).
Lai, W. W. et al. Guidelines and standards for performance of a pediatric echocardiogram: a report from the Task Force of the Pediatric Council of the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 19, 1413–1430 (2006).
Mertens, L. et al. Targeted neonatal echocardiography in the neonatal intensive care unit: practice guidelines and recommendations for trainingwriting group of the American Society of Echocardiography (ASE) in collaboration with the European Association of Echocardiography (EAE) and the Association for European Pediatric Cardiologists (AEPC). J. Am. Soc. Echocardiogr. 24, 1057–1058 (2011).
Lopez, L. et al. Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the Pediatric Measurements Writing Group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J. Am. Soc. Echocardiogr. 23, 465–495 (2010).
Riggs, T. W. et al. Doppler echocardiographic evaluation of right and left ventricular diastolic function in normal neonates. J. Am. Collage Cardiol. 13, 700–705 (1989).
Koestenberger, M. et al. Systolic right ventricular function in preterm and term neonates: reference values of the tricuspid annular plane systolic excursion (TAPSE) in 258 patients and calculation of Z-score values. Neonatology 100, 85–92 (2011).
Koestenberger, M. et al. Right ventricular function in infants, children and adolescents: reference values of the tricuspid annular plane systolic excursion (TAPSE) in 640 healthy patients and calculation of z score values. J. Am. Soc. Echocardiogr. 22, 715–719 (2009).
Aslan, E. et al. Left and right ventricular function by echocardiography, tissue Doppler imaging, carotid intima-media thickness, and asymmetric dimethyl arginine levels in obese adolescents with metabolic syndrome. Cardiol. Young 29, 310–318 (2019).
Basu, S. et al. Two-dimensional speckle tracking imaging detects impaired myocardial performance in children with septic shock, not recognized by conventional echocardiography*. Pediatr. Crit. Care Med. 13, 259–264 (2012).
Patel, M. D. et al. Cardiac dysfunction identified by strain echocardiography is associated with illness severity in pediatric sepsis. Pediatr. Crit. Care Med. 21, e192–e199 (2020).
Sanfilippo, F. et al. Echocardiographic parameters and mortality in pediatric sepsis: a systematic review and meta-analysis*. Pediatr. Crit. Care Med. 22, 251–261 (2021).
Sanfilippo, F. et al. Tissue Doppler assessment of diastolic function and relationship with mortality in critically ill septic patients: a systematic review and meta-analysis. Br. J. Anaesth. 119, 583–594 (2017).
Sanfilippo, F. et al. Diastolic dysfunction and mortality in septic patients: a systematic review and meta-analysis. Intensive Care Med. 41, 1004–1013 (2015).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6, e1000097 (2009).
Ottawa Hospital Research Institute. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (2021).
Abdel-Hady, H. E., Matter, M. K. & El-Arman, M. M. Myocardial dysfunction in neonatal sepsis: a tissue Doppler imaging study*. Pediatr. Crit. Care Med. 13, 318–323 (2012).
Ahmed, T., Abqari, S., Firdaus, U., Shahab, T. & Ali, S. M. Status of pulmonary artery pressures on echocardiography among high‑risk newborns. J. Clin. Neonatol. 9, 235–241 (2020).
Alzahrani, A. K. Cardiac function affection in infants with neonatal sepsis. J. Clin. Trial 7, 5 (2017).
Deshpande, S., Suryawanshi, P., Chaudhary, N. & Maheshwari, R. Cardiac output in late onset neonatal sepsis. J. Clin. Diagn. Res. 11, 4 (2017).
Deshpande, S. et al. Pulmonary hypertension in late onset neonatal sepsis using functional echocardiography: a prospective study. J. Ultrasound 25, 233–239 (2021).
Fahmey, S. S., Hodeib, M., Refaat, K. & Mohammed, W. Evaluation of myocardial function in neonatal sepsis using tissue Doppler imaging. J. Matern. Fetal Neonatal Med. 33, 3752–3756 (2020).
Saini, S. S., Kumar, P. & Kumar, R. M. Hemodynamic changes in preterm neonates with septic shock: a prospective observational study*. Pediatr. Crit. Care Med. 15, 443–450 (2014).
Yengkhom, R. et al. Point of care neonatal ultrasound in late-onset neonatal sepsis. J. Neonatol. 35, 59–63 (2021).
de Waal, K. & Evans, N. Hemodynamics in preterm infants with late-onset sepsis. J. Pediatr. 156, 918–922.e1 (2010).
Bandyopadhyay, T., Saili, A., Yadav, D. K. & Kumar, A. Correlation of functional echocardiography and clinical parameters in term neonates with shock. J. Neonatal Perinat. Med. 13, 167–173 (2020).
Hassan, M. et al. PO-0540 changes in haemodynamic and peripheral perfusion in suspected neonatal sepsis. Arch. Dis. Child. 99, A426.2–A426 (2014).
Tomerak, R. H., El-Badawy, A. A., Hussein, G., Kamel, N. R. M. & Razak, A. R. A. Echocardiogram done early in neonatal sepsis: what does it add? J. Investig. Med. 60, 680–684 (2012).
Töllner, U. Early diagnosis of septicemia in the newborn. Clinical studies and sepsis score. Eur. J. Pediatr. 138, 331–337 (1982).
Rodwell, R. L., Leslie, A. L. & Tudehope, D. I. Early diagnosis of neonatal sepsis using a hematologic scoring system. J. Pediatr. 112, 761–767 (1988).
NNF Teaching Aids. Newborn care. Neonatal sepsis. Management of neonatal sepsis. NNF clinical practice guidelines http://www.nnfi.org/assests/upload/usefull-links-pdf/Diagnosis_and_Management_of_Neonatal_Sepsis_NNFI_CPG_Dec2021.pdf (2021).
Goldstein, B., Giroir, B. & Randolph, A., International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics*. Pediatr. Crit. Care Med. 6, 2–8 (2005).
de Boode, W. P. et al. Application of Neonatologist Performed Echocardiography in the assessment and management of persistent pulmonary hypertension of the newborn. Pediatr. Res. 84, 68–77 (2018).
Kluckow, M. Use of ultrasound in the haemodynamic assessment of the sick neonate. Arch. Dis. Child. Fetal Neonatal Ed. 99, F332–F337 (2014).
Kluckow, M., Seri, I. & Evans, N. Functional echocardiography: an emerging clinical tool for the neonatologist. J. Pediatr. 150, 125–130 (2007).
Mohsen, A. A. & Amin, A. Risk factors and outcomes of persistent pulmonary hypertension of the newborn in neonatal intensive care unit of al-minya University Hospital in Egypt. J. Clin. Neonatol. 2, 78–82 (2013).
Verma, B., Daga, S. R. & Mahapankar, A. Persistent pulmonary hypertension among neonates with sepsis. Indian J. Pediatr. 73, 250–251 (2006).
Dempsey, E. & Rabe, H. The use of cardiotonic drugs in neonates. Clin. Perinatol. 46, 273–290 (2019).
Sehgal, A., Athikarisamy, S. E. & Adamopoulos, M. Global myocardial function is compromised in infants with pulmonary hypertension. Acta Paediatr. 101, 410–413 (2012).
Moore, T. D. et al. Ventricular interaction and external constraint account for decreased stroke work during volume loading in CHF. Am. J. Physiol. Heart Circ. Physiol. 281, H2385–H2391 (2001).
Chagnon, F., Bentourkia, M., Lecomte, R., Lessard, M. & Lesur, O. Endotoxin-induced heart dysfunction in rats: assessment of myocardial perfusion and permeability and the role of fluid resuscitation*. Crit. Care Med. 34, 127–133 (2006).
Galiuto, L., Ignone, G. & DeMaria, A. N. Contraction and relaxation velocities of the normal left ventricle using pulsed-wave tissue Doppler echocardiography. Am. J. Cardiol. 81, 609–614 (1998).
Nagueh, S. F., Middleton, K. J., Kopelen, H. A., Zoghbi, W. A. & Quiñones, M. A. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J. Am. Collage Cardiol. 30, 1527–1533 (1997).
Haileselassie, B. et al. Strain echocardiography parameters correlate with disease severity in children and infants with sepsis. Pediatr. Crit. Care Med. 17, 383–390 (2016).
Rivers, E. et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N. Engl. J. Med. 345, 1368–1377 (2001).
Nguyen, H. B. et al. Early goal-directed therapy in severe sepsis and septic shock: insights and comparisons to ProCESS, ProMISe, and ARISE. Crit. Care 20, 160 (2016).
Menon, K. et al. Criteria for pediatric sepsis-a systematic review and meta-analysis by the pediatric sepsis definition taskforce. Crit. Care Med. 50, 21–36 (2022).
Sullivan, B. A., Kausch, S. L. & Fairchild, K. D. Artificial and human intelligence for early identification of neonatal sepsis. Pediatr. Res. 93, 350–356 (2023).
Sahu, P. et al. Prediction modelling in the early detection of neonatal sepsis. World J. Pediatr. 18, 160–175 (2022).
Acknowledgements
This work was supported by the Italian Ministry of Health with “Current Research funds”.
Author information
Authors and Affiliations
Contributions
F.P. and C.A. contributed to the study conception and design. Material preparation, data collection, and analysis were performed by F.P. and D.U.D.R. The first draft of the manuscript was written by F.P. and revised by D.U.D.R. N.P., F.K., M.P.R., A.D., P.B., and C.A. critically revised it for important intellectual content. All authors reviewed and approved the final version of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pugnaloni, F., De Rose, D.U., Kipfmueller, F. et al. Assessment of hemodynamic dysfunction in septic newborns by functional echocardiography: a systematic review. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03045-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03045-2