Abstract
The coronavirus disease 2019 (COVID-19) in pregnancy causes adverse outcomes for both the mother and the fetus. Neonates are at risk of vertical transmission and in-utero infection. Additionally, intensive care unit (ICU) admission and impairment in the organ systems of the mother are associated with neonatal outcomes, including impaired intrauterine growth, prematurity, and neonatal ICU admission. The management of neonates born from infected mothers has changed over the progress of the pandemic. At the beginning of the pandemic, cesarean section, immediate separation of mother-infant dyads, isolation of neonates, and avoiding of skin-to-skin contact, breast milk, and breastfeeding were the main practices to reduce vertical and horizontal transmission risk in the era of insufficient knowledge. The effects of antenatal steroids and delayed cord clamping on COVID-19 were also not known. As the pandemic progressed, data showed that prenatal, delivery room, and postnatal care of neonates can be performed as pre-pandemic practices. Variants and vaccines that affect clinical course and outcomes have emerged during the pandemic. The severity of the disease and the timing of infection in pregnancy also influence maternal and neonatal outcomes. The knowledge and lessons from COVID-19 will be helpful for the next pandemic if it happens.
Impact
-
Prenatal infection with COVID-19 is associated with adverse maternal and neonatal outcomes.
-
Our review includes the management of neonates with prenatal COVID-19 infection exposure, maternal-fetal, delivery room, and postnatal care of neonates, clinical features, treatment of neonates, and influencing factors such as variants, vaccination, severity of maternal disease, and timing of infection during pregnancy.
-
There is a growing body of data and evidence about the COVID-19 pandemic. The knowledge and lessons from the pandemic will be helpful for the next pandemic if it happens.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Covid-19 Coronavirus Outbreak, https://www.worldometers.info/coronavirus/ (2021).
Manti, S. et al. Effects of vertical transmission of respiratory viruses to the offspring. Front Immunol. 13, 853009 (2022).
Sankaran, D., Nakra, N., Cheema, R., Blumberg, D. & Lakshminrusimha, S. Perinatal Sars-Cov-2 infection and neonatal Covid-19: A 2021 update. Neoreviews 22, e284–e295 (2021).
Gee, S. et al. The legacy of maternal Sars-Cov-2 infection on the immunology of the neonate. Nat. Immunol. 22, 1490–1502 (2021).
Rubio, R. et al. Maternal and neonatal immune response to Sars-Cov-2, Igg transplacental transfer and cytokine profile. Front Immunol. 13, 999136 (2022).
Jamieson, D. J. & Rasmussen, S. A. An update on Covid-19 and pregnancy. Am. J. Obstet. Gynecol. 226, 177–186 (2022).
Tanacan, A. et al. The rate of Sars-Cov-2 positivity in asymptomatic pregnant women admitted to hospital for delivery: Experience of a pandemic center in Turkey. Eur. J. Obstet. Gynecol. Reprod. Biol. 253, 31–34 (2020).
Jamieson, D. J. et al. H1n1 2009 Influenza Virus Infection During Pregnancy in the USA. Lancet 374, 451–458 (2009).
Zambrano, L. D. et al. Update: Characteristics of symptomatic women of reproductive age with laboratory-confirmed Sars-Cov-2 infection by pregnancy status - United States, January 22-October 3, 2020. MMWR Morb. Mortal. Wkly Rep. 69, 1641–1647 (2020).
Lokken, E. M. et al. Disease severity, pregnancy outcomes, and maternal deaths among pregnant patients with severe acute respiratory syndrome Coronavirus 2 infection in Washington State. Am. J. Obstet. Gynecol. 225, 77.e71–77.e14 (2021).
Liu, H. et al. Why are pregnant women susceptible to Covid-19? An immunological viewpoint. J. Reprod. Immunol. 139, 103122 (2020).
Ryan, L. et al. Neonates and Covid-19: State of the art : Neonatal sepsis series. Pediatr. Res 91, 432–439 (2022).
Oncel, M. Y. et al. A multicenter study on epidemiological and clinical characteristics of 125 newborns born to women infected with Covid-19 by Turkish Neonatal society. Eur. J. Pediatr. 180, 733–742 (2021).
Akin, I. M. et al. Epidemiologic and clinical characteristics of neonates with late-onset Covid-19: 1-year data of turkish neonatal society. Eur. J. Pediatr. 181, 1933–1942 (2022).
Bellos, I., Pandita, A. & Panza, R. Maternal and perinatal outcomes in pregnant women infected by Sars-Cov-2: A meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 256, 194–204 (2021).
Chowdhury, S. et al. Covid-19 and pregnancy. Discoveries (Craiova) 10, e147 (2022).
Smith, E. R. et al. Adverse maternal, fetal, and newborn outcomes among pregnant women with Sars-Cov-2 infection: An individual participant data meta-analysis. BMJ Glob. Health 8, e009495 (2023).
Wang, J. & Dong, W. Covid-19: The possibility, ways, mechanisms, and interruptions of mother-to-child transmission. Arch. Gynecol. Obstet. 307, 1687–1696 (2023).
Dong, Y. et al. Epidemiology of Covid-19 among Children in China. Pediatrics 145, e20200702 (2020).
Yoon, H. E. et al. Age-associated changes in the vascular renin-angiotensin system in mice. Oxid. Med. Cell Longev. 2016, 6731093 (2016).
Zimmermann, P. & Curtis, N. Why Is Covid-19 less severe in children? A review of the proposed mechanisms underlying the age-related difference in severity of Sars-Cov-2 Infections. Arch Dis Child (2020).
Sahin, D. et al. Comparison of clinical features and perinatal outcomes between pre-variant and post-variant periods in pregnant women with Sars-Cov-2: Analysis of 1935 cases. Arch. Gynecol. Obstet. 306, 1939–1948 (2022).
National Institutes of Health. Covid-19 Treatment Guidelines. Pregnancy, Lactation, and Covid-19 Therapeutics (Last Updated April 20, 2023), https://www.covid19treatmentguidelines.nih.gov/special-populations/pregnancy/pregnancy-lactation-and-covid-19-therapeutics/? (2023).
Who Therapeutic Guidance: Review of Current Recommendations and Application in Pregnancy (Last Updated Jan 11, 2022), https://cdn.who.int/media/docs/default-source/health-care-readiness-post-covid-19-condition/4_who-therapeutic-guidelines_review-of-current-recommendations-and-application-in-pregnancy_beverley-hunt.pdf (2023).
Committee on Obstetric, P. Committee opinion no. 713: Antenatal corticosteroid therapy for fetal maturation. Obstet. Gynecol. 130, e102–e109 (2017).
Publications & Clinical Guidance. Society for Maternal Fetal Medicine (Updated June, 2022). https://www.smfm.org/covidclinical.
American Academy of Pediatrics. Faqs: Management of Infants Born to Mothers with Suspected or Confirmed Covid-19 (Last Updated:11/10/2022), https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/faqs-management-of-infants-born-to-covid-19-mothers/.
Dubey, P., Reddy, S. Y., Manuel, S. & Dwivedi, A. K. Maternal and neonatal characteristics and outcomes among Covid-19 Infected Women: An updated systematic review and meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 252, 490–501 (2020).
Conde-Agudelo, A. & Romero, R. Sars-Cov-2 infection during pregnancy and risk of preeclampsia: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 226, 68–89.e63 (2022).
Papapanou, M. et al. Maternal and neonatal characteristics and outcomes of Covid-19 in pregnancy: An overview of systematic reviews. Int J. Environ. Res Public Health 18, 596 (2021).
Committee Opinion No. 400: Covid-19 and Pregnancy. Infectious Disease Committee of the Society of Obstetricians and Gynaecologists of Canada., https://sogc.org/common/Uploaded%20files/Latest%20News/Committee%20Opinion%20No.%20400%20COVID-19%20and%20Pregnancy.pdf.
Aguar-Carrascosa, M. et al. General approach to delivery and resuscitation of newborn infants from mothers at risk or proven Covid-19. Semin Fetal Neonatal Med. 28, 101432 (2023).
Wyckoff, M. H. et al. 2021 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations: Summary from the Basic Life Support; Advanced Life Support; Neonatal Life Support; Education, Implementation, and Teams; First Aid Task Forces; and the Covid-19 Working Group. Resuscitation 169, 229–311 (2021).
Erdeve, O. et al. The Turkish Neonatal Society Proposal for the Management of Covid-19 in the Neonatal Intensive Care Unit. Turk. Pediatr. Ars 55, 86–92 (2020).
Shalish, W., Lakshminrusimha, S., Manzoni, P., Keszler, M. & Sant’Anna, G. M. Covid-19 and neonatal respiratory care: Current evidence and practical approach. Am. J. Perinatol. 37, 780–791 (2020).
Hosono, S. et al. Management of infants born to mothers with suspected or confirmed Sars-Cov-2 infection in the delivery room: A tentative proposal 2020. Pediatr. Int 63, 260–263 (2021).
Saus-Ortega, C. Skin-to-skin contact in mothers with suspected, probable, or confirmed Covid-19. Birth.50, 486–495 (2023).
Cdc. Coronavirus Disease (Covid-19) and Breastfeeding, https://www.cdc.gov/breastfeeding/breastfeeding-special-circumstances/maternal-or-infant-illnesses/covid-19-and-breastfeeding.html (2023).
Briana, D., Syridou, G. & Papaevangelou, V. Perinatal Covid-19. Pediatr. Infect. Dis. J. 40, e504–e506 (2021).
Dowse, G. et al. Born into an isolating world: Family-centred care for babies born to mothers with Covid-19. EClinicalMedicine 56, 101822 (2023).
Briana, D. D. & Malamitsi-Puchner, A. Breastfeeding provides a protective hug and the benefits have outweighed the risks during the Covid-19 pandemic. Acta Paediatr. 112, 1177–1181 (2023).
Low, J. M. et al. Titres and neutralising capacity of Sars-Cov-2-specific antibodies in human milk: A systematic review. Arch. Dis. Child Fetal Neonatal Ed. 107, 174–180 (2022).
Vazquez-Vazquez, A., Dib, S., Rougeaux, E., Wells, J. C. & Fewtrell, M. S. The impact of the Covid-19 lockdown on the experiences and feeding practices of new mothers in the Uk: Preliminary data from the Covid-19 New Mum Study. Appetite 156, 104985 (2021).
Gunes, A. O., Dincer, E., Karadag, N., Topcuoglu, S. & Karatekin, G. Effects of Covid-19 pandemic on breastfeeding rates in a neonatal intensive care unit. J. Perinat. Med 49, 500–505 (2021).
Merewood, A. et al. Breastfeeding supportive practices in european hospitals during the Covid-19 pandemic. J. Matern Fetal Neonatal Med. 35, 8514–8520 (2022).
Darcy Mahoney, A. et al. Impact of restrictions on parental presence in neonatal intensive care units related to Coronavirus Disease 2019. J. Perinatol 40, 36-46 (2020).
Jafari, M. et al. Clinical characteristics and outcomes of pregnant women with Covid-19 and comparison with control patients: A systematic review and meta-analysis. Rev. Med Virol. 31, 1–16 (2021).
Walker, G. J. et al. Sars-Cov-2 in human milk is inactivated by holder pasteurisation but not cold storage. J. Paediatr. Child Health 56, 1872–1874 (2020).
Duguay, G. et al. Socioemotional development in infants of pregnant women during the Covid-19 pandemic: The role of prenatal and postnatal maternal distress. Child Adolesc. Psychiatry Ment. Health 16, 28 (2022).
Khan, S. et al. The Covid-19 infection in children and its association with the immune system, prenatal stress, and neurological complications. Int J. Biol. Sci. 18, 707–716 (2022).
Jin, Y. & Murray, L. Perinatal mental health and women’s lived experience of the Covid-19 pandemic: A scoping review of the qualitative literature 2020–2021. Midwifery 123, 103706 (2023).
Cruz-Ramos, M. C., Resurreccion, D. M. & Hernandez-Albujar, Y. Childbirth experience during the Covid-19 pandemic: A qualitative thematic analysis. Midwifery 121, 103669 (2023).
Iyengar, U., Jaiprakash, B., Haitsuka, H. & Kim, S. One year into the pandemic: A systematic review of perinatal mental health outcomes during Covid-19. Front Psychiatry 12, 674194 (2021).
Silva, P. Y. F. et al. Risk of global developmental delay in infants born from mothers with Covid-19: A cross-sectional study. Int. J. Women’s Health 15, 467–474 (2023).
Wiley, K. S., Fox, M. M., Gildner, T. E. & Thayer, Z. M. A Longitudinal study of how women’s prenatal and postnatal concerns related to the Covid-19 pandemic predicts their infants’ social-emotional development. Child Dev. 94, 1356–1367 (2023).
Perlman, J. M. & Salvatore, C. Coronavirus disease 2019 infection in newborns. Clin. Perinatol. 49, 73–92 (2022).
Villar, J. et al. Maternal and neonatal morbidity and mortality among pregnant women with and without Covid-19 Infection: The intercovid multinational cohort study. JAMA Pediatr. 175, 817–826 (2021).
Trevisanuto, D. et al. Coronavirus infection in neonates: A systematic review. Arch. Dis. Child Fetal Neonatal Ed. 106, 330–335 (2021).
Sanchez-Luna, M. et al. Neonates born to mothers with Covid-19: Data from the Spanish Society of Neonatology Registry. Pediatrics 147, e2020015065 (2021).
Hudak, M. L. et al. Maternal and newborn hospital outcomes of perinatal Sars-Cov-2 infection: A national registry. Pediatrics 151, e2022059565 (2023).
Barnes, E. et al. Clinical characteristics and outcomes of Sars-Cov-2 positive neonates born to persons with Sars-Cov-2 infection in pregnancy in Los Angeles County, California, May 22, 2020-February 22, 2021. Pediatr. Infect. Dis. J. 42, 418–422 (2023).
Mark, E. G. et al. Coronavirus disease 2019 in pregnancy and outcomes among pregnant women and neonates: A literature review. Pediatr. Infect. Dis. J. 40, 473–478 (2021).
Di Toro, F. et al. Impact of Covid-19 on maternal and neonatal outcomes: A systematic review and meta-analysis. Clin. Microbiol Infect. 27, 36–46 (2021).
Vergara-Merino, L. et al. Maternal and perinatal outcomes related to Covid-19 and pregnancy: An overview of systematic reviews. Acta Obstet. Gynecol. Scand. 100, 1200–1218 (2021).
Flannery, D. D. et al. Perinatal Covid-19 maternal and neonatal outcomes at two academic birth hospitals. J. Perinatol. 42, 1338–1345 (2022).
Capozza, M. et al. Perinatal transmission and outcome of neonates born to Sars-Cov-2-positive mothers: The experience of 2 highly endemic Italian regions. Neonatology 118, 665–671 (2021).
Panda, S. K., Mishra, A. & Pathak, M. Clinical outcome of neonates born to Sars-Cov-2 positive mothers in India: A systematic review and meta-analysis. Cureus 14, e22958 (2022).
Corman, V. M. et al. Detection of 2019 Novel Coronavirus (2019-Ncov) by Real-Time Rt-Pcr. Euro Surveill 25 (2020).
Kimberlin, D. W. & Stagno, S. Can Sars-Cov-2 Infection Be Acquired in Utero?: More Definitive Evidence Is Needed. JAMA 323, 1788–1789 (2020).
Who Scientific Report. Definition and Categorization of the Timing of Mother-to-Child Transmission of Sars-Cov-2 (Last Updated Feb 7, 2021), https://www.who.int/publications/i/item/WHO-2019-nCoV-mother-to-child-transmission-2021.1.
De Luca, D., Vauloup-Fellous, C., Benachi, A. & Vivanti, A. Transmission of Sars-Cov-2 from mother to fetus or neonate: What to know and what to do? Semin Fetal Neonatal Med. 28, 101429 (2023).
Egloff, C., Vauloup-Fellous, C., Picone, O., Mandelbrot, L. & Roques, P. Evidence and possible mechanisms of rare maternal-fetal transmission of Sars-Cov-2. J. Clin. Virol. 128, 104447 (2020).
Zeng, L. et al. Neonatal early-onset infection with Sars-Cov-2 in 33 neonates born to mothers with Covid-19 in Wuhan, China. JAMA Pediatr. 174, 722–725 (2020).
Amaral, W. N. D. et al. Maternal Coronavirus infections and neonates born to mothers with Sars-Cov-2: A systematic review. Healthcare (Basel) 8 (2020).
Lavizzari, A. et al. International comparison of guidelines for managing neonates at the early phase of the Sars-Cov-2 pandemic. Pediatr. Res 89, 940–951 (2021).
Raschetti, R. et al. Synthesis and systematic review of reported neonatal Sars-Cov-2 infections. Nat. Commun. 11, 5164 (2020).
Bulbul, A. et al. Covid-19 management in newborn babies in the light of recent data: Breastfeeding, rooming-in and clinical symptoms. Sisli Etfal Hastan. Tip. Bul. 54, 261–270 (2020).
Tezer, H. & Bedir Demirdağ, T. Novel Coronavirus Disease (Covid-19) in Children. Turk. J. Med. Sci. 50, 592–603 (2020).
De Luca, D. et al. The essentials about neonatal severe acute respiratory syndrome Coronavirus 2 infection and coronavirus disease: A narrative review. Am. J. Perinatol. 39, S18–S22 (2022).
Royal Collage of Obstetricians and Gynaecologists, Coronavirus (Covid-19) Infection in Pregnancy, Information for Healthcare Professionals, Version 16 (Last Updated Dec 2022), https://www.rcog.org.uk/media/ftzilsfj/2022-12-15-coronavirus-covid-19-infection-in-pregnancy-v16.pdf.
Grazioli, S. et al. Immunological assessment of pediatric multisystem inflammatory syndrome related to Coronavirus Disease 2019. J. Pediatr. Infect. Dis. Soc. 10, 706–713 (2021).
Pawar, R. et al. Neonatal multisystem inflammatory syndrome (Mis-N) associated with prenatal maternal Sars-Cov-2: A case series. Child. (Basel) 8, 572 (2021).
Lakshminrusimha, S., More, K., Shah, P. S., Wynn, J. L. & Sanchez, P. J. Multisystem inflammatory syndrome in neonates (Mis-N) associated with perinatal Sars Cov-2 Infection: Does It Exist? Semin Fetal Neonatal Med. 28, 101433 (2023).
Molloy, E. J., Nakra, N., Gale, C., Dimitriades, V. R. & Lakshminrusimha, S. Multisystem inflammatory syndrome in children (Mis-C) and neonates (Mis-N) associated with Covid-19: Optimizing definition and management. Pediatr. Res 93, 1499–1508 (2023).
Ramaswamy, V. V., Abiramalatha, T., Pullattayil, S. A. & Trevisanuto, D. Multisystem inflammatory disease in neonates (Mis-N) due to Maternal Covid-19. Semin Fetal Neonatal Med. 28, 101431 (2023).
Lima, A. R. O. et al. Maternal Sars-Cov-2 infection associated to systemic inflammatory response and pericardial effusion in the newborn: A case report. J. Pediatr. Infect. Dis. Soc. 10, 536–539 (2021).
Khaund Borkotoky, R., Banerjee Barua, P., Paul, S. P. & Heaton, P. A. Covid-19-related potential multisystem inflammatory syndrome in childhood in a neonate presenting as persistent pulmonary hypertension of the newborn. Pediatr. Infect. Dis. J. 40, e162–e164 (2021).
Sharma, P., Gupta, R. & Mahajan, V. Multisystem inflammatory syndrome presenting as sinus bradycardia in a neonate with prenatal exposure to Covid-19. Indian J. Pediatr. 89, 825 (2022).
Kappanayil, M. et al. Multisystem inflammatory syndrome in a neonate, temporally associated with prenatal exposure to Sars-Cov-2: A case report. Lancet Child Adolesc. Health 5, 304–308 (2021).
Covid-19 Vaccines and Pregnancy: Conversation Guide (Last Updated September 2022), https://www.acog.org/covid-19/covid-19-vaccines-and-pregnancy-conversation-guide-for-clinicians.
American College of Obstetricians and Gynecologists. Covid-19 Vaccination Considerations for Obstetric–Gynecologic Care (Last Updated January 6, 2023), https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/12/covid-19-vaccination-considerations-for-obstetric-gynecologic-care?.
Chen, M. J. et al. Vaccination and treatment options for Sars-Cov2 infection affecting lactation and breastfeeding. Semin Fetal Neonatal Med. 28, 101425 (2023).
Centers for Disease Control and Prevention. Covid Data Tracker. Atlanta Gudohahs, Cdc; 2023. February 15, https://covid.cdc.gov/covid-data-tracker.
Razzaghi, H. et al. Covid-19 vaccination coverage among pregnant women during pregnancy - eight integrated health care organizations, United States, December 14, 2020-May 8, 2021. MMWR Morb. Mortal. Wkly Rep. 70, 895–899 (2021).
Wainstock, T., Sergienko, R., Orenshtein, S. & Sheiner, E. Factors associated with Covid-19 vaccination likelihood during pregnancy. Int J. Gynaecol. Obstet. 161, 478–484 (2023).
Hui, L. et al. Reductions in stillbirths and preterm birth in Covid-19-vaccinated women: A multicenter cohort study of vaccination uptake and perinatal outcomes. Am. J. Obstet. Gynecol. 228, 585.e581–585.e516 (2023).
Moini, A., Rabiei, M., Pirjani, R., Abiri, A. & Maleki-Hajiagha, A. Covid‑19 Vaccine Hesitancy among Pregnant Women and Their Reported Reasons for Vaccine Refusal - a Prospective Study in Tehran, Iran. Vaccine 41, 1490–1495 (2023).
Shimabukuro, T. T. et al. Preliminary findings of Mrna Covid-19 vaccine safety in pregnant persons. N. Engl. J. Med 384, 2273–2282 (2021).
Fell, D. B. et al. Association of Covid-19 vaccination in pregnancy with adverse peripartum outcomes. JAMA 327, 1478–1487 (2022).
Ibroci, E. et al. Impact of prenatal Covid-19 vaccination on delivery and neonatal outcomes: Results from a New York City cohort. Vaccine 41, 649–656 (2023).
Peretz-Machluf, R. et al. Obstetric and neonatal outcomes following Covid-19 vaccination in pregnancy. J. Clin. Med. 11, 2540 (2022).
Carbone, L. et al. Covid-19 vaccine and pregnancy outcomes: A systematic review and meta-analysis. Int J. Gynaecol. Obstet. 159, 651–661 (2022).
Morgan, J. A. et al. Pregnancy outcomes in patients after completion of the Mrna Coronavirus Disease 2019 (Covid-19) vaccination series compared with unvaccinated patients. Obstet. Gynecol. 141, 555–562 (2023).
Olearo, F. et al. Anti-Sars-Cov-2 antibodies in breast milk during lactation after infection or vaccination: A cohort study. J. Reprod. Immunol. 153, 103685 (2022).
Pieri, M. et al. Survival of vaccine-induced human milk Sars-Cov-2 Igg, Iga and Siga immunoglobulins across simulated human infant gastrointestinal digestion. Nutrients 14, 3368 (2022).
Romero Ramirez, D. S. et al. Sars-Cov-2 Antibodies in breast milk after vaccination. Pediatrics 148, e2021052286 (2021).
Rosenberg-Friedman, M. et al. Bnt162b2 Mrna vaccine elicited antibody response in blood and milk of breastfeeding women. Nat. Commun. 12, 6222 (2021).
Collier, A. Y. et al. Immunogenicity of Covid-19 Mrna vaccines in pregnant and lactating women. JAMA 325, 2370–2380 (2021).
Kugelman, N. et al. Maternal and neonatal Sars-Cov-2 immunoglobulin G antibody levels at delivery after receipt of the Bnt162b2 messenger Rna Covid-19 vaccine during the second trimester of pregnancy. JAMA Pediatr. 176, 290–295 (2022).
Ricciardi, A. et al. Serum and breastmilk Sars-Cov-2 specific antibodies following Bnt162b2 vaccine: Prolonged protection from Sars-Cov-2 in newborns and older children. Int J. Infect. Dis. 122, 905–909 (2022).
Zerbo, O. et al. Maternal Sars-Cov-2 vaccination and infant protection against Sars-Cov-2 during the first six months of life. Nat. Commun. 14, 894 (2023).
Jorgensen, S. C. J. et al. Maternal Mrna Covid-19 vaccination during pregnancy and delta or omicron infection or hospital admission in infants: Test negative design study. BMJ 380, e074035 (2023).
Seaton, C. L. et al. Coronavirus Disease 2019 (Covid-19) perinatal outcomes across the pandemic at an academic medical center in New York City. Obstet. Gynecol. 141, 144–151 (2023).
Faraz, S. et al. An insight on the maternal-fetal outcomes of critically Ill pregnant women during the second wave of Covid-19. Cureus 14, e20998 (2022).
Favre, G. et al. Maternal and perinatal outcomes following pre-delta, delta, and omicron Sars-Cov-2 variants infection among unvaccinated pregnant women in France and Switzerland: A prospective cohort study using the Covi-Preg registry. Lancet Reg. Health Eur. 26, 100569 (2023).
Mosnino, E. et al. Impact of Sars-Cov-2 Alpha and Gamma Variants among Symptomatic Pregnant Women: A Two-Center Retrospective Cohort Study between France and Brazil. J. Clin. Med. 11, 2663 (2022).
Choi, H., Lee, E. J., Ahn, Y. S. & Yoo, Y. M. Effects of the Omicron Variant on Perinatal Outcomes in Full-Term Neonates. BMC Pediatr. 22, 625 (2022).
Deng, J. et al. Association of Infection with Different Sars-Cov-2 Variants During Pregnancy with Maternal and Perinatal Outcomes: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 19, 15932 (2022).
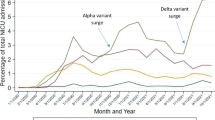
Vousden, N. et al. Severity of maternal infection and perinatal outcomes during periods of Sars-Cov-2 wildtype, alpha, and delta variant dominance in the Uk: prospective cohort study. BMJ Med. 1, e000053 (2022).
Hamidi, O. P. et al. Adverse perinatal outcomes in pregnancies affected by severe Covid-19 infection. AJOG Glob. Rep. 2, 100118 (2022).
Vouga, M. et al. Maternal outcomes and risk factors for Covid-19 severity among pregnant women. Sci. Rep. 11, 13898 (2021).
Vousden, N. et al. Management and implications of severe Covid-19 in pregnancy in the Uk: Data from the Uk obstetric surveillance system national cohort. Acta Obstet. Gynecol. Scand. 101, 461–470 (2022).
Verma, S. et al. Outcomes of maternal-newborn dyads after maternal Sars-Cov-2. Pediatrics 146, e2020005637 (2020).
Khan, D. S. A. et al. Differences in pregnancy and perinatal outcomes among symptomatic versus asymptomatic Covid-19-infected pregnant women: A systematic review and meta-analysis. BMC Pregnancy Childbirth 21, 801 (2021).
Lassi, Z. S. et al. A systematic review and meta-analysis of data on pregnant women with confirmed Covid-19: Clinical presentation, and pregnancy and perinatal outcomes based on Covid-19 severity. J. Glob. Health 11, 05018 (2021).
Sahin, D. et al. Management of pregnant women with Covid-19: A tertiary pandemic center experience on 1416 cases. J. Med. Virol. 94, 1074–1084 (2022).
Regan, A. K., Arah, O. A., Fell, D. B. & Sullivan, S. G. Sars-Cov-2 infection during pregnancy and associated perinatal health outcomes: A national Us cohort study. J. Infect. Dis. 225, 759–767 (2022).
Author information
Authors and Affiliations
Contributions
I.H.C. contributed to conception and design, acquisition of data, and analysis and interpretation of data; drafting the article and revising it critically for important intellectual content, manuscript preparation. A.O.P contributed to acquisition and interpretation of data and assisted in the manuscript preparation. F.E.C. contributed to conception and design, acquisition of data, and analysis and interpretation of data; drafting the article and revising it critically for important intellectual content and assisted in the manuscript preparation. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Celik, I.H., Ozkaya Parlakay, A. & Canpolat, F.E. Management of neonates with maternal prenatal coronavirus infection and influencing factors. Pediatr Res 95, 436–444 (2024). https://doi.org/10.1038/s41390-023-02855-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02855-0
This article is cited by
-
Lessons learned in caring for newborns from one viral outbreak to the next
Pediatric Research (2024)
-
Trends in prenatal and pediatric viral infections, and the impact of climate change
Pediatric Research (2024)
-
Viral infections in pregnancy and impact on offspring neurodevelopment: mechanisms and lessons learned
Pediatric Research (2024)