Abstract
Background
Association between early cardiac function and neonatal outcomes are scarcely reported. The aim of the current study was to describe this association with death, severe bronchopulmonary dysplasia (BPD) and BPD-related pulmonary hypertension (PH).
Methods
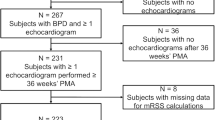
Retrospective cohort study of infants <29 weeks born between 2015 and 2019. Infants with clinically acquired echocardiography at ≤21 days after birth were included and data were extracted by an expert masked to outcomes.
Results
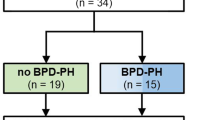
A total of 176 infants were included. Echocardiogram was performed at a median of 9 days (IQR 5-13.5). Of these, 31 (18%) had death/severe BPD and 59 (33.5%) had death/BPD-related PH. Infants with death/severe BPD were of lower birth weight (745 [227] vs 852 [211] grams, p = 0.01) and more exposed to invasive ventilation, late-onset sepsis, inotropes and/or postnatal steroids. Early echocardiograms demonstrated decreased right ventricular [Tricuspid Annular Plane Systolic Excursion: 5.2 (1.4) vs 6.2 (1.5) cm, p = 0.03] and left ventricular function [Ejection fraction 53 (14) vs 58 (10) %, p = 0.03]. Infants with death/BPD-related PH had an increased Eccentricity index (1.35 [0.20] vs 1.26 [0.19], p = 0.02), and flat/bowing septum (19/54 [35%] vs 20/109 [18%], p = 0.021).
Conclusions
In extremely premature infants, altered ventricular function and increased pulmonary pressure indices within the first 21 days after birth, were associated with the combined outcome of death/severe BPD and death/BPD-related PH.
Impact
-
Decreased cardiac function on echocardiography performed during first three weeks of life is associated with severe bronchopulmonary dysplasia in extremely premature infants.
-
In extreme preterm infants, echocardiographic signs of pulmonary hypertension in early life are associated with later BPD-related pulmonary hypertension close to 36 weeks post-menstrual age.
-
Early cardiac markers should be further studied as potential intervention targets in this population.
-
Our study is adding comprehensive analysis of echocardiographic data in infants born below 29 weeks gestational age.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Derived data generated will be shared on reasonable request to the corresponding author.
References
Mourani, P. M. et al. Early pulmonary vascular disease in preterm infants at risk for bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 191, 87–95 (2015).
Morty, R. E. Recent advances in the pathogenesis of Bpd. Semin Perinatol. 42, 404–412 (2018).
Stoll, B. J. et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA 314, 1039–1051 (2015).
Alvarez-Fuente, M. et al. Exploring clinical, echocardiographic and molecular biomarkers to predict bronchopulmonary dysplasia. PLoS One 14, e0213210 (2019).
Bancalari, E. & Claure, N. Definitions and diagnostic criteria for bronchopulmonary dysplasia. Semin Perinatol. 30, 164–170 (2006).
Pérez-Tarazona, S. et al. Respiratory outcomes of “New” bronchopulmonary dysplasia in adolescents: A multicenter study. Pediatr. Pulmonol. 56, 1205–1214 (2021).
Rite, S. et al. The consensus definition of bronchopulmonary dysplasia is an adequate predictor of lung function at preschool age. Front Pediatr. 10, 830035 (2022).
Doyle, L. W. & Anderson, P. J. Long-term outcomes of bronchopulmonary dysplasia. Semin Fetal Neonatal Med. 14, 391–395 (2009).
Dartora, D. R. et al. Association of bronchopulmonary dysplasia and right ventricular systolic function in young adults born preterm. Chest 160, 287–296 (2021).
Flahault, A. et al. Left ventricle structure and function in young adults born very preterm and association with neonatal characteristics. J. Clin. Med. 10, 1760 (2021).
Lasry, A. et al. Cardiopulmonary function abnormalities in cohort of adults following bronchopulmonary dysplasia as preterm infants. Am. J. Perinatol 39, 1410–1417 (2021).
Arjaans, S. et al. Fate of pulmonary hypertension associated with bronchopulmonary dysplasia beyond 36 weeks postmenstrual age. Arch. Dis. Child Fetal Neonatal Ed. 106, 45–50 (2021).
Doyle, L. W. Postnatal corticosteroids to prevent or treat bronchopulmonary dysplasia. Neonatology 118, 244–251 (2021).
Abman, S. H. Pulmonary hypertension: The hidden danger for newborns. Neonatology 118, 211–217 (2021).
Mourani, P. M. et al. Early pulmonary vascular disease in preterm infants is associated with late respiratory outcomes in childhood. Am. J. Respir. Crit. Care Med. 199, 1020–1027 (2019).
Mirza, H. et al. Natural history of postnatal cardiopulmonary adaptation in infants born extremely preterm and risk for death or bronchopulmonary dysplasia. J. Pediatr. 198, 187–193.e181 (2018).
Kim, H. H. et al. Early pulmonary hypertension is a risk factor for bronchopulmonary dysplasia-associated late pulmonary hypertension in extremely preterm infants. Sci. Rep. 11, 11206 (2021).
Kim, Y. J., Shin, S. H., Park, H. W., Kim, E. K. & Kim, H. S. Risk factors of early pulmonary hypertension and its clinical outcomes in preterm infants: A systematic review and meta-analysis. Sci. Rep. 12, 14186 (2022).
Sheth, S., Goto, L., Bhandari, V., Abraham, B. & Mowes, A. Factors associated with development of early and late pulmonary hypertension in preterm infants with bronchopulmonary dysplasia. J. Perinatol. 40, 138–148 (2020).
Abman, S. H. et al. Pediatric pulmonary hypertension: Guidelines from the American Heart Association and American Thoracic Society. Circulation 132, 2037–2099 (2015).
Lakshminrusimha, S. & Steinhorn, R. H. Pulmonary vascular biology during neonatal transition. Clin. Perinatol. 26, 601–619 (1999).
Jobe, A. H. & Bancalari, E. Bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med 163, 1723–1729 (2001).
Higgins, R. D. et al. Bronchopulmonary dysplasia: Executive summary of a workshop. J. Pediatr. 197, 300–308 (2018).
Richardson, D. K., Corcoran, J. D., Escobar, G. J. & Lee, S. K. Snap-Ii and Snappe-Ii: Simplified newborn illness severity and mortality risk scores. J. Pediatr. 138, 92–100 (2001).
Chou, J. H., Roumiantsev, S. & Singh, R. Peditools electronic growth chart calculators: Applications in clinical care, research, and quality improvement. J. Med. Internet Res. 22, e16204 (2020).
Lai, W. W. et al. Guidelines and standards for performance of a pediatric echocardiogram: A report from the task force of the pediatric council of the american society of echocardiography. J. Am. Soc. Echocardiogr. 19, 1413–1430 (2006).
Altit, G., Bhombal, S., Feinstein, J., Hopper, R. K. & Tacy, T. A. Diminished right ventricular function at diagnosis of pulmonary hypertension is associated with mortality in bronchopulmonary dysplasia. Pulm. Circ. 9, 2045894019878598 (2019).
Mertens, L. L., Ganame, J. & Eyskens, B. Echocardiographic evaluation of systolic function. In Echocardiography in pediatric and congenital heart disease: from fetus to adult (eds Lai, W. W., Mertens, L. L., Cohen, M. S. & Geva T.) 76-94 (John Wiley & Sons, Ltd, 2009).
Sehgal, A., Malikiwi, A., Paul, E., Tan, K. & Menahem, S. Right ventricular function in infants with bronchopulmonary dysplasia: association with respiratory sequelae. Neonatology 109, 289–296 (2016).
Altit, G. et al. Pathophysiology, screening and diagnosis of pulmonary hypertension in infants with bronchopulmonary dysplasia—a review of the literature. Paediatr. Respir. Rev. 23, 16–26 (2017).
Koestenberger, M., Friedberg, M. K., Nestaas, E., Michel-Behnke, I. & Hansmann, G. Transthoracic echocardiography in the evaluation of pediatric pulmonary hypertension and ventricular dysfunction. Pulm. Circ. 6, 15–29 (2016).
Jone, P. N., Hinzman, J., Wagner, B. D., Ivy, D. D. & Younoszai, A. Right ventricular to left ventricular diameter ratio at end-systole in evaluating outcomes in children with pulmonary hypertension. J. Am. Soc. Echocardiogr. 27, 172–178 (2014).
Jone, P. N. et al. Right atrial deformation in predicting outcomes in pediatric pulmonary hypertension. Circ. Cardiovasc Imaging 10, e006250 (2017).
Jone, P. N. & Ivy, D. D. Echocardiography in pediatric pulmonary hypertension. Front Pediatr. 2, 124 (2014).
Abraham, S. & Weismann, C. G. Left ventricular end-systolic eccentricity index for assessment of pulmonary hypertension in infants. Echocardiography 33, 910–915 (2016).
Haque, U. et al. Right ventricular performance using myocardial deformation imaging in infants with bronchopulmonary dysplasia. J. Perinatol. 37, 81–87 (2017).
Murase, M., Morisawa, T. & Ishida, A. Serial assessment of left-ventricular function using tissue doppler imaging in premature infants within 7 days of life. Pediatr. Cardiol. 34, 1491–1498 (2013).
James, A. T. et al. Longitudinal assessment of left and right myocardial function in preterm infants using strain and strain rate imaging. Neonatology 109, 69–75 (2016).
Czernik, C. et al. Development of left ventricular longitudinal speckle tracking echocardiography in very low birth weight infants with and without bronchopulmonary dysplasia during the neonatal period. PLoS One 9, e106504 (2014).
Helfer, S., Schmitz, L., Bührer, C. & Czernik, C. Tissue doppler-derived strain and strain rate during the first 28 days of life in very low birth weight infants. Echocardiography 31, 765–772 (2014).
Bokiniec, R., Własienko, P., Borszewska-Kornacka, M. & Szymkiewicz-Dangel, J. Evaluation of left ventricular function in preterm infants with bronchopulmonary dysplasia using various echocardiographic techniques. Echocardiography 34, 567–576 (2017).
Torres, E. et al. Left ventricle phenotyping utilizing tissue doppler imaging in premature infants with varying severity of bronchopulmonary dysplasia. J. Clin. Med 10, 2211 (2021).
Seth, S. A., Soraisham, A. S. & Harabor, A. Risk factors and outcomes of early pulmonary hypertension in preterm infants. J. Matern Fetal Neonatal Med 31, 3147–3152 (2018).
Bhat, R., Salas, A. A., Foster, C., Carlo, W. A. & Ambalavanan, N. Prospective analysis of pulmonary hypertension in extremely low birth weight infants. Pediatrics 129, e682–e689 (2012).
Mehler, K. et al. An echocardiographic screening program helps to identify pulmonary hypertension in extremely low birthweight infants with and without bronchopulmonary dysplasia: A single-center experience. Neonatology 113, 81–88 (2018).
Altit, G. et al. Outcomes of extremely premature infants comparing patent ductus arteriosus management approaches. J. Pediatr. 235, 49–57 (2021).
de Carvalho Nunes, G. et al. Natural evolution of the patent ductus arteriosus in the extremely premature newborn and respiratory outcomes. J. Perinatol. 42, 642–648 (2022).
Hundscheid, T. et al. Expectant management or early ibuprofen for patent ductus arteriosus. N. Engl. J. Med. 388, 980–990 (2023).
Benitz, W. E. Treatment of persistent patent ductus arteriosus in preterm infants: Time to accept the null hypothesis? J. Perinatol 30, 241–252 (2010).
Benitz, W. E. Patent ductus arteriosus: To treat or not to treat? Arch. Dis. Child. Fetal Neonatal Ed. 97, F80–F82 (2012).
Benitz, W. E. & Committee on Fetus and Newborn, American Academy of Pediatrics. Patent ductus arteriosus in preterm infants. Pediatrics 137 (2016).
El-Khuffash, A. et al. A patent ductus arteriosus severity score predicts chronic lung disease or death before discharge. J. Pediatr. 167, 1354–1361.e1352 (2015).
El-Khuffash, A., Weisz, D. E. & McNamara, P. J. Reflections of the changes in patent ductus arteriosus management during the last 10 years. Arch. Dis. Child Fetal Neonatal Ed. 101, F474–F478 (2016).
Prior presentation
Results from this study were presented in abstract, poster and oral formats at the 15th International Conference Neonatal and Childhood Pulmonary Vascular Disease (2022), the Pediatric Academic Societies meeting (2022) and at Neoheart scientific meeting (2022).
Funding
This project was supported by grants from the Just for Kids Foundation, the Montreal Children’s Hospital foundation and the Department of Pediatrics of McGill University.
Author information
Authors and Affiliations
Contributions
S.S.M. contributed to conceptualizing and designing the study, collected the data, analyzed the data, and drafted the initial and revised manuscript. G.D.C.N. collected the data and critically reviewed the manuscript. A.D. contributed to the interpretation of the findings, and critically reviewed the manuscript. P.W. collected the data and critically reviewed the manuscript. J.S. collected the data and critically reviewed the manuscript. M.B. contributed to the interpretation of the findings, and critically reviewed the manuscript. G.S.A. contributed to the interpretation of the findings, and critically reviewed the manuscript. G.A. conceptualized and designed the study, supervised data analysis, contributed to the interpretation of the findings and critically reviewed the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent Statement
Not required. The study was approved by the institutional ethics review committee.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Moore, S.S., De Carvalho Nunes, G., Dancea, A. et al. Early cardiac function and death, severe bronchopulmonary dysplasia and pulmonary hypertension in extremely preterm infants. Pediatr Res 95, 293–301 (2024). https://doi.org/10.1038/s41390-023-02817-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02817-6