Abstract
Background
To study the gestational age-specific risk factors and outcomes of severe acute kidney injury (AKI) in neonates with necrotizing enterocolitis (NEC).
Methods
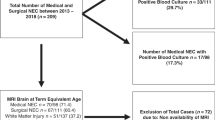
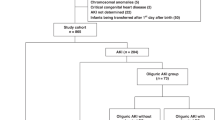
Retrospective cohort study comparing gestational age (GA)-specific clinical data between infants without severe AKI (stage 0/1 AKI) and those with severe AKI (stages 2 and 3 AKI) stratified by GA ≤27 and >27 weeks.
Results
Infants with GA ≤27 weeks had double the rate of severe AKI (46.3% vs. 20%). In infants with GA >27 weeks, male sex, outborn, and nephrotoxic medication exposure were associated with severe AKI. On multivariable logistic regression, in infants with GA ≤27 weeks, surgical NEC (OR 35.08 (CI 5.05, 243.73), p < 0.001) and ostomy (OR 6.2(CI 1.29, 29.73), p = 0.027) were associated with significantly higher odds of severe AKI. Surgical NEC infants with GA >27 weeks and severe AKI were significantly more likely to be outborn, have later NEC onset, need dopamine, and have longer hospitalization (158 days [110; 220] vs.75.5 days [38.8; 105]; p = 0.007 than those with non-severe AKI.
Conclusion
In neonates with NEC, surgical intervention was associated with moderate-to-severe AKI in infants with GA ≤27 weeks and with longer hospitalization in infants with GA >27 weeks.
Impact
-
In both cohorts need for surgery, stoma, cholestasis, and mechanical ventilation were associated with severe AKI; however, the infants with GA <27 weeks had twice the risk of severe AKI than GA >27 weeks group.
-
The longer exposure to nephrotoxic medication and referral need were significant risk factors for AKI in GA >27 weeks group.
-
GA-specific kidney protective and monitoring strategies to prevent AKI and its consequences are needed to improve the clinical outcomes in neonates with NEC. Understanding the risk factors and short- and long-term outcomes unique to different GA groups will help inform those strategies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All data generated and analyzed during this study are included in this article and its supplementary information files.
References
Neu, J. & Walker, W. A. Necrotizing enterocolitis. N. Engl. J. Med. 364, 255–264 (2011).
Sankaran, K. et al. Variations in incidence of necrotizing enterocolitis in Canadian neonatal intensive care units. J. Pediatr. Gastroenterol. Nutr. 39, 366–372 (2004).
Jetton, J. G. et al. Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc. Health 1, 184–194 (2017).
Charlton, J. R. et al. Incidence and risk factors of early onset neonatal AKI. Clin. J. Am. Soc. Nephrol. 14, 184–195 (2019).
Wu, Y., Hua, X., Yang, G., Xiang, B. & Jiang, X. Incidence, risk factors, and outcomes of acute kidney injury in neonates after surgical procedures. Pediatr Nephrol. 35, 1341–1346 (2020).
Mallory, P. P. et al. Acute kidney injury, fluid overload, and outcomes in children supported with extracorporeal membrane oxygenation for a respiratory indication. ASAIO J. 66, 319–326 (2020).
Starr, M. C. et al. Acute kidney injury and bronchopulmonary dysplasia in premature neonates born less than 32 weeks' gestation. Am. J. Perinatol. 37, 341–348 (2020).
Stoops, C. et al. The Association of Intraventricular Hemorrhage and Acute Kidney Injury in Premature Infants from the Assessment of the Worldwide Acute Kidney Injury Epidemiology in Neonates (AWAKEN) Study. Neonatology 116, 321–330 (2019).
Criss, C. N. et al. Acute kidney injury in necrotizing enterocolitis predicts mortality. Pediatr. Nephrol. 33, 503–510 (2018).
Bakhoum, C. Y., Basalely, A., Koppel, R. I. & Sethna, C. B. Acute kidney injury in preterm infants with necrotizing enterocolitis. J. Matern Fetal Neonatal Med. 32, 3185–3190 (2019).
Garg, P. M., Tatum, R., Ravisankar, S., Shekhawat, P. S. & Chen, Y. H. Necrotizing enterocolitis in a mouse model leads to widespread renal inflammation, acute kidney injury, and disruption of renal tight junction proteins. Pediatr. Res. 78, 527–532 (2015).
Sanchez, C., Garcia, M. A. & Valdes, B. D. Acute kidney injury in newborns with necrotizing enterocolitis: risk factors and mortality. Bol. Med. Hosp. Infant Mex. 76, 210–214 (2019).
Garg, P. M. et al. Severe acute kidney injury in neonates with necrotizing enterocolitis: risk factors and outcomes. Pediatr. Res. 90, 642–649 (2021).
Bell, M. J. et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann. Surg. 187, 1–7 (1978).
Jetton, J. G. & Askenazi, D. J. Acute kidney injury in the neonate. Clin. Perinatol. 41, 487–502 (2014).
Zappitelli, M. et al. Developing a neonatal acute kidney injury research definition: a report from the NIDDK neonatal AKI workshop. Pediatr. Res. 82, 569–573 (2017).
Basu, R. K. et al. Assessment of Worldwide Acute Kidney Injury, Renal Angina and Epidemiology in Critically Ill Children (AWARE): a prospective study to improve diagnostic precision. J Clin Trials 5, 222 (2015).
Garg, P. M. et al. Hematological predictors of mortality in neonates with fulminant necrotizing enterocolitis. J. Perinatol. 41, 1110–1121 (2021).
Hashem, R. H., Mansi, Y. A., Almasah, N. S. & Abdelghaffar, S. Doppler ultrasound assessment of the splanchnic circulation in preterms with neonatal sepsis at risk for necrotizing enterocolitis. J. Ultrasound 20, 59–67 (2017).
Murphy, H. J. et al. Nephrotoxic medications and acute kidney injury risk factors in the neonatal intensive care unit: clinical challenges for neonatologists and nephrologists. Pediatr. Nephrol. 35, 2077–2088 (2020).
Salerno, S. N. et al. Association between nephrotoxic drug combinations and acute kidney injury in the neonatal intensive care unit. J. Pediatr. 228, 213–219 (2021).
Rhone, E. T., Carmody, J. B., Swanson, J. R. & Charlton, J. R. Nephrotoxic medication exposure in very low birth weight infants. J. Matern. Fetal Neonatal Med. 27, 1485–1490 (2014).
Martini, S. et al. Impact of nephrotoxic drugs on urinary biomarkers of renal function in very preterm infants. Pediatr. Res. 91, 1715–1722 (2022).
Garg, P. M. et al. Clinical impact of NEC-associated sepsis on outcomes in preterm infants. Pediatr. Res. 92, 1705–1715 (2022).
Coggins, S. A. et al. Acute kidney injury associated with late-onset neonatal sepsis: a matched cohort study. J. Pediatr. 231, 185–192.e184 (2021).
Seely, K. A. et al. Hemodynamic changes in the kidney in a pediatric rat model of sepsis-induced acute kidney injury. Am. J. Physiol. Ren. Physiol. 301, F209–F217 (2011).
Geier, A., Fickert, P. & Trauner, M. Mechanisms of disease: mechanisms and clinical implications of cholestasis in sepsis. Nat. Clin. Pract. Gastroenterol. Hepatol. 3, 574–585 (2006).
Acknowledgements
The Mississippi Center for Clinical and Translational Research for supporting NEC research.
Funding
P.M.G. and W.B.H. are partially supported by the NIGMS of the NIH under Award Number 5U54GM115428. A.M.S. has funding from the NHBLI K23-HL148394, R01-HL146818, L40-HL148910-2, and R56-HL164434. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
P.M.G. designed the study. P.M.G., I.A.P., R.R., M.A.Y.A., C.W.Y., J.G.J., A.M.S., and W.B.H. collected, analyzed the data and wrote the manuscript. All authors contributed to and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Garg, P.M., Pittman, I.A., Ansari, M.A.Y. et al. Gestational age-specific clinical correlates of acute kidney injury in preterm infants with necrotizing enterocolitis. Pediatr Res 94, 2016–2025 (2023). https://doi.org/10.1038/s41390-023-02736-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02736-6
This article is cited by
-
Neurodevelopmental impairment following surgical necrotizing enterocolitis with gestational age ≥ 28 weeks: who is at risk?
Pediatric Surgery International (2024)