Abstract
Background
We identified patient characteristics associated with an increased risk of developing MIS-C.
Methods
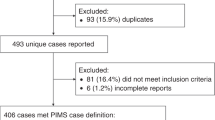
We conducted a longitudinal cohort study of 1,195,327 patients aged 0–19 years between 2006 and 2021, including the first two waves of the pandemic (February 25–August 22, 2020 and August 23, 2020-March 31, 2021). Exposures included prepandemic morbidity, birth outcomes, and family history of maternal disorders. Outcomes included MIS-C, Kawasaki disease, and other Covid-19 complications during the pandemic. We calculated risk ratios (RRs) and 95% confidence intervals (CIs) for the association between patient exposures and these outcomes using log-binomial regression models adjusted for potential confounders.
Results
Among 1,195,327 children, 84 developed MIS-C, 107 Kawasaki disease, and 330 other Covid-19 complications during the first year of the pandemic. Prepandemic hospitalizations for metabolic disorders (RR 11.3, 95% CI 5.61–22.6), atopic conditions (RR 3.34, 95% CI 1.60–6.97), and cancer (RR 8.11, 95% CI 1.13–58.3) were strongly associated with the risk of MIS-C, compared with no exposure. These same exposures were also associated with Kawasaki disease and other Covid-19 complications. However, birth characteristics and history of maternal morbidity were not associated with MIS-C development.
Conclusions
Children with pre-existing morbidity have a considerably elevated risk of MIS-C.
Impact
-
Morbidities that predispose children to multisystem inflammatory syndrome (MIS-C) are unclear.
-
In this study, prepandemic hospitalizations for metabolic disorders, atopic conditions, and cancer were associated with an elevated risk of MIS-C.
-
Birth characteristics and family history of maternal morbidity were not, however, associated with MIS-C.
-
Pediatric morbidities may play a greater role in MIS-C onset than maternal or perinatal characteristics, and may help clinicians better recognize children at risk for this complication.
Similar content being viewed by others
Introduction
Multisystem inflammatory syndrome in children (MIS-C) is a rare hyperinflammatory condition that can develop in the weeks following severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.1 Yet, predisposing risk factors are poorly understood. Systematic reviews of around 2000 children with MIS-C suggest that one-third of patients have underlying comorbidities.2,3,4 Obesity is most commonly reported, followed by asthma and chronic lung disease.2,3,4 These conditions involve immune pathology that could influence inflammatory responses leading to MIS-C.5 The role of immune dysfunction in the development of MIS-C is nevertheless unclear, as two-thirds of children are thought to be previously healthy. However, relevant morbidities in apparently healthy children may be missed, as current data are based on case series or descriptive reports that identify risk factors at the time of admission only.6,7,8,9
Studies of other inflammatory conditions support the possibility that early life exposures may be associated with MIS-C. Having a history of infant morbidity or maternal autoimmune disease is linked with the development of Kawasaki disease,10,11 a childhood vasculitis on the same clinical spectrum as MIS-C.1 Studies have shown that preterm birth increases the chance of having severe acute SARS-CoV-2 infections.12 Yet, the association of adverse birth outcomes and family history with risk of MIS-C has not been studied. Given the scarcity of data, we used a longitudinal cohort approach to identify prepandemic risk factors associated with the development of MIS-C. We used data from Quebec, the hardest hit region of Canada at the start of the pandemic. The first case of MIS-C in Quebec was detected March 15, 2020.13
Methods
Study design and population
We conducted a longitudinal cohort study of 1,195,327 children aged <20 years in Quebec, Canada between April 1, 2006 and March 31, 2021. This period includes the first (February 25, 2020 to August 22, 2020) and second (August 23, 2020 to March 31, 2021) waves of the pandemic. The first wave includes a trough between July 11, 2020 and August 22, 2020 when community transmission of coronavirus disease 2019 (Covid-19) slowed briefly.
We drew the cohort from the Maintenance and Use of Data for the Study of Hospital Clientele database of hospital discharge summaries in Quebec.14 The data are population based and include the majority of children, as approximately 98% are born in hospital. Children in the dataset are linked with their mothers. The data provide demographic characteristics, the primary reason for hospitalization, up to 40 secondary diagnoses, and 35 interventions during admission. Morbidities such as asthma, diabetes, and obesity and interventions such as cesarean section and ventilation are coded using the International Classification of Diseases and Canadian Classification of Health Interventions.
We used unique patient identifiers to track children forward through time for admissions related to birth, childhood, and the development of MIS-C. We also followed mothers through time to determine if there was a family history maternal morbidity during pregnancy or at other points in life. We included hospitalizations anywhere in the province, but excluded children with missing health insurance numbers as we could not follow them over time.
Outcomes
There were three mutually exclusive outcomes in this study: MIS-C, Kawasaki disease, and hospitalization for other Covid-19 complications during the pandemic. We expressed each outcome as a binary variable with the comparison group comprised of unaffected children who were never hospitalized for these conditions.
We identified cases of MIS-C between 0 and 19 years, following the case definition of the World Health Organization.13 The World Health Organization defines MIS-C as (1) fever lasting 3 or more days, (2) laboratory markers of systemic inflammation, (3) no other microbial cause of inflammation, and (4) at least two of the following symptoms: rash, conjunctivitis, or signs of mucocutaneous inflammation; hypotension or shock; myocardial dysfunction, pericarditis, valvulitis, or coronary abnormalities; coagulopathy; and acute gastrointestinal symptoms with onset approximately 2–6 weeks after a SARS-CoV-2 infection.13 This case definition was also followed by physicians in Quebec. We captured MIS-C using the diagnostic code U07.3, following previous research.15 Validation analyses indicate that the data have high sensitivity and specificity for MIS-C.13
We included Kawasaki disease between 0 and 19 years as a secondary outcome (diagnostic code M30.3). Kawasaki disease has clinical characteristics similar to MIS-C, including fever, mucocutaneous inflammation, and coronary artery involvement.1 Some cases of MIS-C may have been classified as Kawasaki disease at the start of the pandemic.13 To account for this possibility, we categorized patients with both Kawasaki disease and a history of Covid-19 infection as MIS-C. This situation applied to fewer than five patients.
We included Covid-19 admissions between 0 and 19 years as a tertiary outcome (diagnostic codes U07.1, U07.2, U07.4, U07.5). These children were admitted for complications of Covid-19 that required respiratory support, intensive care, or other care unrelated to MIS-C.
Prepandemic exposures
We included prepandemic childhood morbidities that were potentially associated with MIS-C based on previous cross-sectional studies.2,3,4 We considered metabolic disorders (diabetes, obesity, hypertension, errors of metabolism); circulatory disorders; respiratory disorders including pneumonia and asthma; atopic conditions; autoimmune disease; cancer; anemia; nephritis; ophthalmic or otologic disorders; skin disorders; dental caries; neurodevelopmental and mental health disorders; epilepsy; and sleep disorders.
We identified birth characteristics, including preterm birth, low birth weight, multiple birth, congenital anomaly, birth trauma, neonatal jaundice, severe neonatal morbidity,16 and admission to a neonatal intensive care unit. Using maternal data, we captured pregnancy characteristics such as maternal age, parity, gestational diabetes, preeclampsia, placental disorders, hemorrhage, premature rupture of membranes, labor complications, cesarean section, instrumental delivery, maternal transfusion, and severe maternal morbidity.14 We had birth characteristics for 1,195,117 children in the cohort (99.98%).
We further identified children who had a family history of maternal hospital admission. We followed mothers over time to identify hospitalizations before delivery or any time during the child’s life. We included maternal admissions for cardiovascular disease, metabolic disorders (diabetes type 1 and 2, obesity, and hypertension), pneumonia, other respiratory infections, asthma and obstructive lung disease, atopic conditions, autoimmune disease, cancer, anemia, mental health disorders, substance use disorders, intensive care unit admission, and any morbidity in the Charlson index.14 We had information on maternal morbidities for 1,188,781 children in the cohort (99.5%). We identified prepandemic morbidities using diagnostic and intervention codes.
Covariates
Age, sex, and socioeconomic status may be associated with the exposures and outcomes in this study and be confounders.7,17,18,19 We therefore included age at the outcome admission or at the end of the study (0–4, 5–12, 13–19 years), child sex, and degree of socioeconomic deprivation (very disadvantaged, disadvantaged, middle, advantaged, very advantaged) as potential confounders. To measure socioeconomic deprivation, we used an index of employment, high school education, and average income for small geographic areas with national census data.10
Data analysis
We examined the clinical presentation and management of patients using diagnostic and intervention codes. We calculated the proportion of patients with: organ failure; shock and hypotension; cardiovascular, respiratory, gastrointestinal, dermatologic, or ophthalmic complications; lymphadenopathy; anemia; abnormal blood cell counts; electrolyte imbalance; and death. We computed the proportion of patients that required intensive care, ventilation, or intravenous immunoglobulin, and the proportion admitted with concurrent infections, appendicitis, neurodevelopmental and mental health disorders, or injuries. We measured the length of hospital stay (1–4, 5–10, 11 days or more).
We estimated risk ratios (RRs) and 95% confidence intervals (CIs) for the association of prepandemic risk factors with MIS-C, Kawasaki disease, and other Covid-19 complications using log-binomial regression. We ran separate models for each outcome, and adjusted for age, sex, and socioeconomic deprivation.
In sensitivity analyses, we examined sex-specific associations of childhood exposures with MIS-C, Kawasaki disease, and other Covid-19 complications. We determined whether associations differed when Covid-19 was the primary versus secondary diagnosis. We assessed statistical significance using 95% CIs and conducted the analysis in SAS version 9.4 (SAS Institute Inc.). The institutional review board of the University of Montreal Hospital Research Centre deemed that this study was exempt from informed consent and ethical review, as the data were de-identified and the study conformed to requirements for analysis of administrative datasets in Canada.
Results
Among 1,195,327 children in the cohort, 84 were hospitalized for MIS-C, 107 for Kawasaki disease, and 330 for other Covid-19 complications during the first year of the pandemic (Table 1). MIS-C was more frequent between age 5 and 12 years (54.8%), whereas Kawasaki disease was more common between 0 and 4 years (74.8%). Hospitalization for other Covid-19 complications occurred more often between age 0 and 4 years (39.4%) and in adolescence (42.7%). There was a slight male predominance for MIS-C and Kawasaki disease.
Children with MIS-C had more severe clinical presentations than children with Kawasaki disease and other Covid-19 complications (Table 2). Organ failure, shock, pleural effusion, gastrointestinal complications, abnormal platelet counts, and concurrent infections were all more common in patients with MIS-C. Cardiovascular complications were common in both MIS-C and Kawasaki disease. Children with MIS-C more frequently required intensive care and mechanical ventilation than children with Kawasaki disease and other Covid-19 complications. Most children with MIS-C (86.9%) and Kawasaki disease (74.8%) were treated with intravenous immunoglobulin. Total hospital stay was longer for children with MIS-C, with 64.3% requiring 5 days or more. There were fewer than five deaths, all among children with other Covid-19 complications.
Several prepandemic morbidities were associated with the risk of MIS-C (Tables 3 and S1). Compared with no morbidity, children with prepandemic hospitalizations for metabolic disorders (RR 11.3, 95% CI 5.61–22.6), atopic conditions (RR 3.34, 95% CI 1.60–6.97), cancer (RR 8.11, 95% CI 1.13–58.3), and sleep disorders (RR 8.49, 95% CI 3.90–18.5) had considerably elevated risks of MIS-C. Except for metabolic conditions, these same morbidities were also associated with the risk of Kawasaki disease. However, a wider range of conditions, including nearly all types of prepandemic admissions, were associated with an increased risk of other Covid-19 complications.
Neonatal birth characteristics were not associated with an increased risk of MIS-C (Table 4). However, congenital anomalies and severe neonatal morbidity were associated with more than 1.8 times the risk of Kawasaki disease. Preterm birth, low birth weight, congenital anomalies, severe neonatal morbidity, and neonatal intensive care unit admission were associated with twice the risk of other Covid-19 complications. Maternal pregnancy characteristics were not associated with the risk of any outcome.
Having a family history of maternal morbidity did not influence the risk of MIS-C (Table 5). However, maternal metabolic disease was associated with an elevated risk of Kawasaki disease (RR 1.85, 95% CI 1.03–3.34). Children whose mothers had any morbidity, including cardiovascular disease, hypertension, or anemia, all had an elevated risk of other Covid-19 complications. Children whose mothers were admitted for Covid-19 during the pandemic had more than 24 times the risk of also being hospitalized for Covid-19.
In sex-stratified sensitivity analyses, prepandemic childhood hospitalizations were more strongly associated with the risk of MIS-C in girls than boys (Table S2). The association in girls was most apparent for metabolic disorders (RR 14.4, 95% CI 5.58–37.3), atopic conditions (RR 4.91, 95% CI 1.73–13.9), and cancer (RR 18.6, 95% CI 2.54–135.9). Prepandemic hospitalizations were more strongly associated with Covid-19 complications when Covid-19 was the primary reason for hospitalization (RR 3.65, 95% CI 2.38–5.60) than a secondary diagnosis (RR 1.90, 95% CI 1.39–2.59).
Discussion
In this longitudinal cohort of 1.2 million children followed from birth to the pandemic, children with prepandemic morbidity were significantly more likely to develop MIS-C. Prepandemic hospitalizations for metabolic disorders, atopic conditions, and cancer were associated with up to 11 times the risk of MIS-C compared with no history of these morbidities. Metabolic disorders, atopic conditions, and cancer were also associated with the risk of Kawasaki disease and other Covid-19 complications. However, adverse birth outcomes and family history of maternal morbidity were not associated with the development of MIS-C. Thus, pre-existing childhood metabolic disorders, atopy, and cancer may be more important risk factors for MIS-C than adverse birth outcomes or family history.
The findings align with previous literature suggesting that MIS-C is more severe than other acute inflammatory conditions.1,2,3,4,6,7,20,21 Patients with MIS-C had markedly greater organ involvement in our cohort than patients with Kawasaki disease or other Covid-19 complications. Cardiac complications, gastrointestinal involvement, and shock were common in MIS-C. These complications were less prevalent in children with Kawasaki disease, where coronary aneurysm was more common. Pneumonia was, however, more prevalent in children with other Covid-19 complications. MIS-C was also frequent in children 5 to 12 years, whereas Kawasaki disease was prevalent before 5 years and acute Covid-19 complications after 12 years. The differing age and clinical presentation of these conditions supports the likelihood that MIS-C is distinct from Kawasaki disease and acute Covid-19 complications.1,3,6,7,20,21 Despite multiorgan involvement for both conditions, no child with MIS-C or Kawasaki disease died during admission.
Risk factors for MIS-C are less understood. Cross-sectional studies have found that obesity is reported in up to 50% of patients with MIS-C.6,7,22 Some have proposed that patients with obesity have a proinflammatory state that contributes to the immune-mediated pathogenesis of MIS-C.22,23,24 Patients with obesity have elevated levels of C-reactive protein and IL-6,25 biomarkers also present in MIS-C.2,3 In analyses of case series, errors of metabolism such as glucose-6-dehydrogenase deficiency are also linked with the risk of MIS-C.26 Nevertheless, past studies have not quantified the association between metabolic disorders and MIS-C relative to a general population.6,7,8 In our cohort representative of an entire Canadian province, prepandemic hospitalizations for metabolic disorders were associated with 11 times the risk of MIS-C. Metabolic conditions may, therefore, be strong risk factors for MIS-C.
A few studies have found that asthma is common in patients with MIS-C.2,3,4,5 In one systematic review, the pooled prevalence of asthma or chronic lung disease was 14.4%.3 Investigators have proposed that imbalance in regulatory T cells may contribute to the immunopathogenesis of MIS-C.5,27 However, no epidemiologic study has yet established an association between asthma and MIS-C. In our cohort, asthma appeared to be associated with twice the risk of MIS-C, although the association was not significant owing to a low number of events. Atopic conditions overall were more strongly associated with the risk of MIS-C. Thus, it is possible that atopic diseases as a whole, and not just asthma, are risk factors for MIS-C. Better data on allergies will be needed in future studies to assess the role of atopy in the development of MIS-C.
Cancer was associated with 8 times the risk of MIS-C. Children with cancer may have underlying immune dysregulation due to chemotherapy or bone marrow transplantation.28 Several case reports have identified MIS-C in children with leukemia.29,30,31 In one report, a child with acute myelomonocytic leukemia developed MIS-C after chemotherapy.31 Fc gamma receptors (FcγR) on monocytic blasts were thought to be involved,31 as FcγR mediated activation of immune cells is implicated in MIS-C pathogenesis.1 Chemotherapy is also associated with cytokine release syndrome.29,30 Toxicity of chemotherapy can moreover be incorrectly diagnosed as MIS-C.29,30 The extent to which patients with cancer are at risk of MIS-C will require confirmation, as patients undergoing chemotherapy are usually immunosuppressed.
The same childhood morbidities implicated in MIS-C were associated with Kawasaki disease and other Covid-19 complications. Atopic conditions and cancer were associated with Kawasaki disease, whereas metabolic disorders and most childhood morbidities were associated with other Covid-19 complications. Cross-sectional reports suggest that obesity is more prevalent in children with MIS-C than Kawasaki disease or other Covid-19 complications,7,8 but our data indicate that metabolic conditions are more strongly associated with other Covid-19 complications than MIS-C. It may be that obesity increases the risk of morbidity in general, and is not specific to MIS-C.
Slightly more boys developed MIS-C than girls, which is similar to reports from other regions.2,3,4 However, childhood morbidities were more strongly associated with the risk of MIS-C in girls. Sex differences in the pathogenesis of diseases such as obesity, asthma, and cancer have been documented.32 Some data suggest that immune responses after viral infections may be greater or persist longer in females.33 Estrogen and immune-related genes on the X chromosome are thought to mediate sex differences,33 but the extent to which these factors explain our findings is unclear.
Having a history of adverse birth outcomes or maternal morbidity was not associated with the risk of MIS-C. Previous studies have not examined these risk factors in relation to MIS-C, despite evidence that perinatal complications can have long term consequences.34 There is one exception, a study showing that preterm birth was not associated with the development of MIS-C before 1 year of age.9 However, older children were not studied. In our study, preterm birth and other perinatal characteristics were not associated with MIS-C at any age. In contrast, preterm birth and congenital anomalies were associated with other Covid-19 complications, similar to what has been reported in the literature.12,35 While congenital anomalies were associated with Kawasaki disease, preterm birth was not, although prior work has found that preterm birth may be a determinant of this outcome.36
There were limitations in this study. We used hospital data which may be subject to nondifferential misclassification. We did not have information on race, ethnicity, and paternal characteristics. Quebec is a diverse province that provides universal healthcare regardless of race or socioeconomic status. Nevertheless, it is possible that factors related to race or ethnicity affected access to care, or that unmeasured economic factors influenced the results. We did not have access to laboratory test results for Covid-19 and misclassification remains possible. We did not have data on SARS-CoV-2 variants or vaccination, but all cases of MIS-C occurred before the emergence of delta and omicron and the rollout of vaccines. We included morbidities severe enough to require hospitalization, rather than mild morbidities treated on an outpatient basis that are more likely to be misclassified. Clinical features of MIS-C may be underreported. Owing to the low number of children with MIS-C, power may have been insufficient to detect weak associations. As many comparisons were made, the results of this study should be considered exploratory. Our study is representative of a multicultural population with access to universal healthcare; however, generalizability to other populations requires further study.
In this longitudinal study, prepandemic hospitalizations for metabolic disorders, atopic conditions, and cancer were associated with an increased risk of developing MIS-C. These childhood morbidities were also risk factors for Kawasaki disease and other Covid-19 complications. However, birth characteristics and family history of maternal morbidity were not associated with the development of MIS-C. The findings indicate that childhood morbidity may be more important for the development of MIS-C than birth characteristics or maternal morbidity.
Data availability
The datasets generated during and/or analysed during the current study are available in the Institut de la statistique du Québec repository, https://statistique.quebec.ca/recherche/#/accueil.
References
Sharma, C. et al. Multisystem inflammatory syndrome in children and Kawasaki disease: a critical comparison. Nat. Rev. Rheumatol. 17, 731–748 (2021).
Hoste, L., Van Paemel, R. & Haerynck, F. Multisystem inflammatory syndrome in children related to COVID-19: a systematic review. Eur. J. Pediatr. 180, 2019–2034 (2021).
Yasuhara, J., Watanabe, K., Takagi, H., Sumitomo, N. & Kuno, T. COVID-19 and multisystem inflammatory syndrome in children: a systematic review and meta-analysis. Pediatr. Pulmonol. 56, 837–848 (2021).
Santos, M. O. et al. Multisystem inflammatory syndrome (MIS-C): a systematic review and meta-analysis of clinical characteristics, treatment, and outcomes. J. Pediatr. (Rio. J.) 98, 338–349 (2022).
Soyak Aytekin, E. et al. Obesity is a risk factor for decrease in lung function after COVID-19 infection in children with asthma. Pediatr. Pulmonol. 57, 1668–1676 (2022).
Feldstein, L. R. et al. Characteristics and outcomes of US children and adolescents with multisystem inflammatory syndrome in children (MIS-C) compared with severe acute COVID-19. JAMA 325, 1074–1087 (2021).
Godfred-Cato, S. et al. Distinguishing multisystem inflammatory syndrome in children from COVID-19, Kawasaki disease and toxic shock syndrome. Pediatr. Infect. Dis. J. 41, 315–323 (2022).
Martin, B. et al. Characteristics, outcomes, and severity risk factors associated with SARS-CoV-2 infection among children in the US National COVID Cohort Collaborative. JAMA Netw. Open 5, e2143151 (2022).
Swann, O. V. et al. Clinical characteristics of children and young people admitted to hospital with covid-19 in United Kingdom: prospective multicentre observational cohort study. BMJ 370, m3249 (2020).
Belkaibech, S. et al. Maternal autoimmune disorders and risk of Kawasaki disease in offspring. J. Pediatr. 222, 240–243.e1 (2020).
Hayward, K., Wallace, C. A. & Koepsell, T. Perinatal exposures and Kawasaki disease in Washington State: a population-based, case-control study. Pediatr. Infect. Dis. J. 31, 1027–1031 (2012).
Woodruff, R. C. et al. Risk factors for severe COVID-19 in children. Pediatrics 49, e2021053418 (2021).
Veljanovic, N., Jean, S., Trépanier, P.-L. & Mazza, J. Faisabilité de la vigie et surveillance des cas du syndrome inflammatoire multisystémique de l’enfant liés ou non à la COVID-19. https://www.inspq.qc.ca/publications/3179-faisabilite-vigie-syndrome-inflammatoire-multisystemique-enfant-covid19 (2021).
Ukah, U. V., Dayan, N., Potter, B. J., Ayoub, A. & Auger, N. Severe maternal morbidity and risk of mortality beyond the postpartum period. Obstet. Gynecol. 137, 277–284 (2021).
Auger, N. et al. Multisystem inflammatory syndrome in adults: comparison with other inflammatory conditions during the Covid-19 pandemic. Respir. Med. 206, 107084 (2023).
Lebreton, E. et al. Measuring severe neonatal morbidity using hospital discharge data in France. Paediatr. Perinat. Epidemiol. 36, 190–201 (2022).
Weng, Y.-H., Yang, C.-Y. & Chiu, Y.-W. Neonatal outcomes in relation to sex differences: a national cohort survey in Taiwan. Biol. Sex. Differ. 6, 30 (2015).
Liu, N. et al. Neighbourhood family income and adverse birth outcomes among singleton deliveries. J. Obstet. Gynaecol. Can. 32, 1042–1048 (2010).
Kim, M. K. et al. Socioeconomic status can affect pregnancy outcomes and complications, even with a universal healthcare system. Int. J. Equity Health 17, 2 (2018).
Consiglio, C. R. et al. The immunology of multisystem inflammatory syndrome in children with COVID-19. Cell 183, 968.e7–981.e7 (2020).
Kabeerdoss, J. et al. Severe COVID-19, multisystem inflammatory syndrome in children, and Kawasaki disease: immunological mechanisms, clinical manifestations and management. Rheumatol. Int. 41, 19–32 (2021).
Ahmed, M. et al. Multisystem inflammatory syndrome in children: a systematic review. EClinicalMedicine 26, 100527 (2020).
Nogueira-de-Almeida, C. A. et al. COVID-19 and obesity in childhood and adolescence: a clinical review. J. Pediatr. (Rio. J.) 96, 546–558 (2020).
Kelishadi, R., Roufarshbaf, M., Soheili, S., Payghambarzadeh, F. & Masjedi, M. Association of childhood obesity and the immune system: a systematic review of reviews. Child. Obes. 13, 332–346 (2017).
Sattar, N., McInnes, I. B. & McMurray, J. J. V. Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanisms. Circulation 142, 4–6 (2020).
Almoosa, Z. A. et al. Multisystem inflammatory syndrome in children, the real disease of COVID-19 in pediatrics - a multicenter case series from Al-Ahsa, Saudi Arabia. Cureus 12, e11064 (2020).
Chen, M.-R. et al. Phenotype, susceptibility, autoimmunity, and immunotherapy between Kawasaki disease and coronavirus disease-19 associated multisystem inflammatory syndrome in children. Front. Immunol. 12, 632890 (2021).
Guilcher, G. M. T. et al. Immune function in childhood cancer survivors: a Children’s Oncology Group review. Lancet Child Adolesc. Health 5, 284–294 (2021).
Ragoonanan, D. et al. Case discussion and literature review: cancer immunotherapy, severe immune-related adverse events, multi-inflammatory syndrome, and severe acute respiratory syndrome coronavirus 2. Front. Oncol. 11, 625707 (2021).
Tekle-Yohannes, G. H., Mann, E. & Miller, M. A. Multisystem inflammatory syndrome in children during induction chemotherapy in a newly diagnosed pediatric acute myeloid leukemia and concurrent COVID-19. J. Pediatr. Hematol. Oncol. 44, e532–e536 (2022).
Pandrowala, A. et al. SARS‐CoV‐2‐related multisystem inflammatory syndrome in an immunocompromised child with leukemia. Pediatr. Blood Cancer 68, e28995 (2021).
Piccini, P., Montagnani, C. & de Martino, M. Gender disparity in pediatrics: a review of the current literature. Ital. J. Pediatr. 44, 1 (2018).
Klein, S. L. & Flanagan, K. L. Sex differences in immune responses. Nat. Rev. Immunol. 16, 626–638 (2016).
Melville, J. & Moss, T. The immune consequences of preterm birth. Front. Neurosci. 7, 79 (2013).
Kompaniyets, L. et al. Underlying medical conditions associated with severe COVID-19 illness among children. JAMA Netw. Open 4, e2111182 (2021).
Takeuchi, A. et al. Preterm birth and Kawasaki disease: a nationwide Japanese population- based study. Pediatr. Res. 92, 557–562 (2022).
Funding
This study was supported by the Canadian Institutes of Health Research (PUU-177957) and the Fonds de recherche du Québec-Santé (296785).
Author information
Authors and Affiliations
Contributions
N.A., H.K., C.Q., E.L., and T.M.L. conceived and designed the study. G.L. analyzed the data, with input from N.A., G.C.-C., J.H.-P., and É.B. All authors contributed to the interpretation of the results. N.A., G.L., and J.H.-P. drafted the initial manuscript, and G.C.-C., H.K., C.Q., E.L., É.B., and T.M.L. critically revised it for important intellectual content. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
C.Q. holds a Tier 1 Canada Research Chair in Infection Prevention. The remaining authors declare no conflict of interest.
Ethics approval and consent to participate
Patient consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Auger, N., Côté-Corriveau, G., Kang, H. et al. Multisystem inflammatory syndrome in 1.2 million children: longitudinal cohort study of risk factors. Pediatr Res 95, 325–333 (2024). https://doi.org/10.1038/s41390-023-02633-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02633-y