Abstract
Background
There is growing evidence that neonatal surgery for non-cardiac congenital anomalies (NCCAs) in the neonatal period adversely affects long-term neurodevelopmental outcome. However, less is known about acquired brain injury after surgery for NCCA and abnormal brain maturation leading to these impairments.
Methods
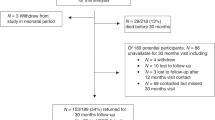
A systematic search was performed in PubMed, Embase, and The Cochrane Library on May 6, 2022 on brain injury and maturation abnormalities seen on magnetic resonance imaging (MRI) and its associations with neurodevelopment in neonates undergoing NCCA surgery the first month postpartum. Rayyan was used for article screening and ROBINS-I for risk of bias assessment. Data on the studies, infants, surgery, MRI, and outcome were extracted.
Results
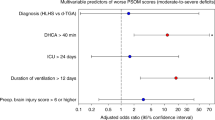
Three eligible studies were included, reporting 197 infants. Brain injury was found in n = 120 (50%) patients after NCCA surgery. Sixty (30%) were diagnosed with white matter injury. Cortical folding was delayed in the majority of cases. Brain injury and delayed brain maturation was associated with a decrease in neurodevelopmental outcome at 2 years of age.
Conclusions
Surgery for NCCA was associated with high risk of brain injury and delay in maturation leading to delay in neurocognitive and motor development. However, more research is recommended for strong conclusions in this group of patients.
Impact
-
Brain injury was found in 50% of neonates who underwent NCCA surgery.
-
NCCA surgery is associated with a delay in cortical folding.
-
There is an important research gap regarding perioperative brain injury and NCCA surgery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Rowe, M. I. & Rowe, S. A. The last fifty years of neonatal surgical management. Am. J. Surg. 180, 345–352 (2000).
Stolwijk, L. J. et al. Neurodevelopmental outcomes after neonatal surgery for major noncardiac anomalies. Pediatrics 137, 335–341.e1 (2016).
Moran, M. M. et al. Associations of neonatal noncardiac surgery with brain structure and neurodevelopment: a prospective case-control study. J. Pediatr. 212, 93–101.e2 (2019).
Radhakrishnan, R. et al. Correlation of MRI brain injury findings with neonatal clinical factors in infants with congenital diaphragmatic hernia. AJNR Am. J. Neuroradiol. 37, 1745–1751 (2016).
Walker, K. et al. Developmental outcomes at 3 years of age following major non-cardiac and cardiac surgery in term infants: a population-based study. J. Paediatr. Child Health 51, 1221–1225 (2015).
Mawlana, W. et al. Neurodevelopmental outcomes of infants with esophageal atresia and tracheoesophageal fistula. J. Pediatr. Surg. 53, 1651–1654 (2018).
Gischler, S. J. et al. Interdisciplinary structural follow-up of surgical newborns: a prospective evaluation. J. Pediatr. Surg. 44, 1382–1389 (2009).
Church, J. T. et al. Neurodevelopmental outcomes in CDH survivors: a single institution’s experience. J. Pediatr. Surg. 53, 1087–1091 (2018).
Gorra, A. S. et al. Long-term neurodevelopmental outcomes in children born with gastroschisis: the tiebreaker. J. Pediatr. Surg. 47, 125–129 (2012).
Harris, E. L. et al. The long-term neurodevelopmental and psychological outcomes of gastroschisis: a cohort study. J. Pediatr. Surg. 51, 549–553 (2016).
Bevilacqua, F. et al. Factors affecting short-term neurodevelopmental outcome in children operated on for major congenital anomalies. J. Pediatr. Surg. 50, 1125–1129 (2015).
Davidson, A. J. et al. Anesthesia and neurotoxicity to the developing brain: the clinical relevance. Paediatr. Anaesth. 21, 716–721 (2011).
Morriss, F. H. Jr. et al. Surgery and neurodevelopmental outcome of very low-birth-weight infants. JAMA Pediatr. 168, 746–754 (2014).
Wilder, R. T. et al. Is there any relationship between long-term behavior disturbance and early exposure to anesthesia? Curr. Opin. Anaesthesiol. 23, 332–336 (2010).
DiMaggio, C., Sun, L. S., Ing, C. & Li, G. Pediatric anesthesia and neurodevelopmental impairments: a Bayesian meta-analysis. J. Neurosurg. Anesthesiol. 24, 376–381 (2012).
Baak, L. M. et al. Feasibility and safety of intranasally administered mesenchymal stromal cells after perinatal arterial ischaemic stroke in the Netherlands (PASSIoN): a first-in-human, open-label intervention study. Lancet Neurol. 21, 528–536 (2022).
Benders, M. J. et al. Feasibility and safety of erythropoietin for neuroprotection after perinatal arterial ischemic stroke. J. Pediatr. 164, 481–486.e62 (2014).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J. Clin. Epidemiol. 62, 1006–1012 (2009).
Ouzzani, M., Hammady, H., Fedorowicz, Z. & Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 5, 210 (2016).
Sterne, J. A. C. et al. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ 355, i4919 (2016).
Stolwijk, L. J. et al. Neonatal surgery for noncardiac congenital anomalies: neonates at risk of brain injury. J. Pediatr. 182, 335–341.e1 (2017).
Gunn-Charlton, J. K. et al. Neonatal neuroimaging after repair of congenital diaphragmatic hernia and long-term neurodevelopment outcome. World J. Pediatr. Surg. 2, e000037 (2019).
Mongerson, C. R. L., Jaimes, C., Zurakowski, D., Jennings, R. W. & Bajic, D. Infant corpus callosum size after surgery and critical care for long-gap esophageal atresia: qualitative and quantitative MRI. Sci. Rep. 10, 6408 (2020).
Rudisill, S. S. et al. Neurologic injury and brain growth in the setting of long-gap esophageal atresia perioperative critical care: a pilot study. Brain Sci. 9, 383 (2019).
Mongerson, C. R. L. et al. Infant brain structural MRI analysis in the context of thoracic non-cardiac surgery and critical care. Front. Pediatr. 7, 315 (2019).
Mongerson, C. R. L., Jennings, R. W., Zurakowski, D. & Bajic, D. Quantitative MRI study of infant regional brain size following surgery for long-gap esophageal atresia requiring prolonged critical care. Int. J. Dev. Neurosci. 79, 11–20 (2019).
Rhee, C. J. et al. Neonatal cerebrovascular autoregulation. Pediatr. Res. 84, 602–610 (2018).
Khwaja, O. & Volpe, J. J. Pathogenesis of cerebral white matter injury of prematurity. Arch. Dis. Child. Fetal Neonatal Ed. 93, F153–F161 (2008).
Baburamani, A. A., Ek, C. J., Walker, D. W. & Castillo-Melendez, M. Vulnerability of the developing brain to hypoxic-ischemic damage: contribution of the cerebral vasculature to injury and repair? Front. Physiol. 3, 424 (2012).
Mader, I., Schöning, M., Klose, U. & Küker, W. Neonatal cerebral infarction diagnosed by diffusion-weighted MRI: pseudonormalization occurs early. Stroke 33, 1142–1145 (2002).
Hirtz, D. & Ment, L. R. Cerebellar hemorrhage in the premature infant-time for a balanced approach. J. Pediatr. 178, 9–10 (2016).
Dudink, J., Jeanne Steggerda, S. & Horsch, S. State-of-the-art neonatal cerebral ultrasound: technique and reporting. Pediatr. Res. 87, 3–12 (2020).
Kubota, A. et al. Psychosocial and cognitive consequences of major neonatal surgery. J. Pediatr. Surg. 46, 2250–2253 (2011).
Peetsold, M. G. et al. Psychological outcome and quality of life in children born with congenital diaphragmatic hernia. Arch. Dis. Child. 94, 834–840 (2009).
Frisk, V., Jakobson, L. S., Unger, S., Trachsel, D. & O’Brien, K. Long-term neurodevelopmental outcomes of congenital diaphragmatic hernia survivors not treated with extracorporeal membrane oxygenation. J. Pediatr. Surg. 46, 1309–1318 (2011).
Jakobson, L. S., Frisk, V., Trachsel, D. & O’Brien, K. Visual and fine-motor outcomes in adolescent survivors of high-risk congenital diaphragmatic hernia who did not receive extracorporeal membrane oxygenation. J. Perinatol. 29, 630–636 (2009).
Hamrick, S. E., Strickland, M. J., Shapira, S. K., Autry, A. & Schendel, D. Use of special education services among children with and without congenital gastrointestinal anomalies. Am. J. Intellect. Dev. Disabil. 115, 421–432 (2010).
Cheong, J. L. et al. Association between moderate and late preterm birth and neurodevelopment and social-emotional development at age 2 years. JAMA Pediatr. 3, e164805 (2017).
Apai, C., Shah, R., Tran, K. & Pandya Shah, S. Anesthesia and the developing brain: a review of sevoflurane-induced neurotoxicity in pediatric populations. Clin. Ther. 43, 762–778 (2021).
Warner, D. O. et al. Neuropsychological and behavioral outcomes after exposure of young children to procedures requiring general anesthesia: the Mayo Anesthesia Safety in Kids (MASK) Study. Anesthesiology 129, 89–105 (2018).
Useinovic, N., Maksimovic, S., Near, M., Quillinan, N. & Jevtovic-Todorovic, V. Do we have viable protective strategies against anesthesia-induced developmental neurotoxicity? Int. J. Mol. Sci. 23, 1128 (2022).
Davidson, A. J. et al. Neurodevelopmental outcome at 2 years of age after general anaesthesia and awake-regional anaesthesia in infancy (GAS): an international multicentre, randomised controlled trial. Lancet 387, 239–250 (2016).
McCann, M. E. et al. Neurodevelopmental outcome at 5 years of age after general anaesthesia or awake-regional anaesthesia in infancy (GAS): an international, multicentre, randomised, controlled equivalence trial. Lancet 393, 664–677 (2019).
Ibrahim, J., Mir, I. & Chalak, L. Brain imaging in preterm infants <32 weeks gestation: a clinical review and algorithm for the use of cranial ultrasound and qualitative brain MRI. Pediatr. Res. 84, 779–806 (2018).
Volpe, J. J. Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol. 8, 110–124 (2009).
Hinojosa-Rodríguez, M. et al. Clinical neuroimaging in the preterm infant: diagnosis and prognosis. Neuroimage Clin. 14, 355–368 (2017).
Volpe, J. J. Dysmaturation of premature brain: importance, cellular mechanisms, and potential interventions. Pediatr. Neurol. 95, 42–66 (2019).
Chorna, O., Hamm, E., Cummings, C., Fetters, A. & Maitre, N. L. Speech and language interventions for infants aged 0 to 2 years at high risk for cerebral palsy: a systematic review. Dev. Med. Child Neurol. 59, 355–360 (2017).
Perinatal arterial stroke treated with stromal cells intranasally. ClinicalTrials.gov identifier: NCT03356821.
Darbepoetin for ischemic neonatal stroke to augment regeneration (DINOSAUR) ClinicalTrials.gov identifier: NCT03171818.
Novak, I. et al. Early, accurate diagnosis and early intervention in cerebral palsy: advances in diagnosis and treatment. JAMA Pediatr. 171, 897–907 (2017).
Author information
Authors and Affiliations
Contributions
Each author has met the Pediatric Research authorship requirements. M.A., M.L.T., J.D., P.M.A.L., M.J.N.L.B.: substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; and final approval of the version to be published. M.Y.A.L.: drafting the article or revising it critically for important intellectual content; and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aalten, M., Tataranno, M.L., Dudink, J. et al. Brain injury and long-term outcome after neonatal surgery for non-cardiac congenital anomalies. Pediatr Res 94, 1265–1272 (2023). https://doi.org/10.1038/s41390-023-02629-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02629-8