Abstract
Background
MRI is the gold standard test to define brain injury in infants with neonatal encephalopathy(NE). As imaging findings evolve considerably over the first week, early imaging may not fully reflect the final nature of the injury. This study aimed to compare day 4 versus second week MRI in infants with NE.
Methods
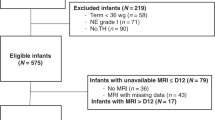
Retrospective cohort study including infants who received therapeutic hypothermia(TH) for NE and had two MRIs: early (≤7days) and late (>7days). MRIs were clinically reported and also reviewed by study investigators.
Results
94infants with NE were included (40mild,49moderate,5severe). Twenty-four infants(26%) had a normal early scan of which 3/24(13%) had injury noted on repeat MRI. Seventy infants(74%) had abnormal findings noted on early MRI, of which 4/70(6%) had further evolution of injury while 11/70(16%) had complete resolution of findings. Applying a grading system resulted in a change of grade in 7 infants.
Conclusion
In infants who received TH for NE, 19% had changes noted between their early and late MRIs. While the impact on predicting neurodevelopmental outcome was not studied, relying solely on early MRI may overestimate injury in a proportion of infants and miss injury in others. Combining early and late MRI allows for better characterization of injury.
Impact
-
MRI is the gold standard tool to define brain injury in infants with NE, however, imaging findings evolve considerably over the first week of life.
-
Most centers perform a single MRI on day 4 after rewarming.
-
In our cohort, 19% of infants had a notable change in their MRI findings between early (within the first week) and late (beyond the first week) scans.
-
Relying solely on early MRI may overestimate injury in a proportion of infants and miss injury in others.
-
Combining early and late MRI following hypothermia allows for better characterization of brain injury.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Kurinczuk, J. J., White-Koning, M. & Badawi, N. Epidemiology of neonatal encephalopathy and hypoxic-ischaemic encephalopathy. Early Hum. Dev. 86, 329–338 (2010).
Conway, J. M., Walsh, B. H., Boylan, G. B. & Murray, D. M. Mild hypoxic ischaemic encephalopathy and long term neurodevelopmental outcome - A systematic review. Early Hum. Dev. 120, 80–87 (2018). May.
van Kooij, B. J. et al. Serial MRI and neurodevelopmental outcome in 9- to 10-year-old children with neonatal encephalopathy. J. Pediatr. 157, 221–227.e2 (2010).
Jacobs, S. E. et al. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst Rev. 2013, CD003311 (2013).
Barkovich, A. J. et al. Prediction of neuromotor outcome in perinatal asphyxia: evaluation of MR scoring systems. AJNR 19, 143–149 (1998).
Weeke, L. C. et al. A Novel Magnetic Resonance Imaging Score Predicts Neurodevelopmental Outcome After Perinatal Asphyxia and Therapeutic Hypothermia. J. Pediatr. 192, 33–40.e2 (2018).
Rutherford, M., Pennock, J., Schwieso, J., Cowen, F. & Dubowitz, L. Hypoxic-ischaemic encephalopathy: early and late magnetic resonance imaging findings in relation to outcome. Arch. Dis. Child Fetal Neonatal Ed. 75, F145–F151 (1996).
Rutherford, M. A. et al. Abnormal magnetic resonance signal in the internal capsule predicts poor neurodevelopmental outcome in infants with hypoxic-ischemic encephalopathy. Pediatrics 102, 323–328 (1998).
Hayes, B. C. et al. Brain magnetic resonance imaging and outcome after hypoxic ischaemic encephalopathy. J. Matern Fetal Neonatal Med 29, 777–782 (2016).
Mercuri, E. et al. Head growth in infants with hypoxic-ischemic encephalopathy: correlation with neonatal magnetic resonance imaging. Pediatrics 106, 235–243 (2000).
Steinman, K. J. et al. Neonatal Watershed Brain Injury on MRI Correlates with Verbal IQ at Four Years. Pediatrics 123, 1025–1030 (2009).
Miller, S. P. et al. Patterns of brain injury in term neonatal encephalopathy. J. Pediatr. 146, 453–460 (2005).
Shankaran, S. et al. Brain injury following trial of hypothermia for neonatal hypoxic-ischaemic encephalopathy. Arch. Dis. Child Fetal Neonatal Ed. 97, F398–F404 (2012).
Ferrari, F. et al. General movements in full-term infants with perinatal asphyxia are related to Basal Ganglia and thalamic lesions. J. Pediatr. 158, 904–911 (2011).
Wisnowski, J. L. et al. Neuroimaging in the term newborn with neonatal encephalopathy. Semin Fetal Neonatal Med 26, 101304 (2021).
Rutherford, M. et al. Magnetic resonance imaging in perinatal brain injury: clinical presentation, lesions and outcome. Pediatr. Radio. 36, 582–592 (2006).
Douglas-Escobar, M. & Weiss, M. D. Hypoxic-Ischemic Encephalopathy: A Review for the Clinician. JAMA Pediatr. 169, 397–403 (2015).
Chakkarapani, E. et al. Reliability of Early Magnetic Resonance Imaging (MRI) and Necessity of Repeating MRI in Noncooled and Cooled Infants With Neonatal Encephalopathy. J. Child Neurol. 31, 553–559 (2016).
Skranes, J. H. et al. Brain imaging in cooled encephalopathic neonates does not differ between four and 11 days after birth. Acta Paediatr. 104, 752–758 (2015).
McKinstry, R. C. et al. A prospective, longitudinal diffusion tensor imaging study of brain injury in newborns. Neurology 59, 824–833 (2002).
Barkovich, A. J. et al. MR imaging, MR spectroscopy, and diffusion tensor imaging of sequential studies in neonates with encephalopathy. AJNR 27, 533–547 (2006).
Executive summary: Neonatal encephalopathy and neurologic outcome, second edition. Report of the American College of Obstetricians and Gynecologists’ Task Force on Neonatal Encephalopathy. Obstet. Gynecol. 123, 896–901 (2014).
Walsh, B. H. et al. Differences in standardized neonatal encephalopathy exam criteria may impact therapeutic hypothermia eligibility. Pediatr Res. 92, 791–798 (2022).
Finelli, P. F. Diagnostic approach to restricted-diffusion patterns on MR imaging. Neurol. Clin. Pr. 2, 287–93 (2012).
Lo, L., Tan, A. C., Umapathi, T. & Lim, C. C. Diffusion-weighted MR imaging in early diagnosis and prognosis of hypoglycemia. AJNR 27, 1222–1224 (2006).
Schaefer, P. W., Grant, P. E. & Gonzalez, R. G. Diffusion-weighted MR imaging of the brain. Radiology 217, 331–345 (2000).
Lawrence, R. K. & Inder, T. E. Anatomic changes and imaging in assessing brain injury in the term infant. Clin. Perinatol. 35, 679–693 (2008).
Bednarek, N. et al. Impact of therapeutic hypothermia on MRI diffusion changes in neonatal encephalopathy. Neurology 78, 1420–1427 (2012).
Al Amrani, F. et al. Prediction of outcome in asphyxiated newborns treated with hypothermia: Is a MRI scoring system described before the cooling era still useful? Eur. J. Paediatr. Neurol. 22, 387–95 (2018).
Shankaran, S. et al. Neonatal Magnetic Resonance Imaging Pattern of Brain Injury as a Biomarker of Childhood Outcomes following a Trial of Hypothermia for Neonatal Hypoxic-Ischemic Encephalopathy. J. Pediatr. 167, 987–993.e3 (2015).
O’Kane, A. et al. Early Versus Late Brain Magnetic Resonance Imaging after Neonatal Hypoxic Ischemic Encephalopathy Treated with Therapeutic Hypothermia. J. Pediatr. 232, 73–9.e2 (2021).
Wintermark, P. et al. Early versus late MRI in asphyxiated newborns treated with hypothermia. Arch. Dis. Child Fetal Neonatal Ed. 96, F36–F44 (2011).
Ouwehand, S. et al. Predictors of Outcomes in Hypoxic-Ischemic Encephalopathy following Hypothermia: A Meta-Analysis. Neonatology 117, 411–27. (2020).
Charon, V. et al. Early MRI in neonatal hypoxic-ischaemic encephalopathy treated with hypothermia: Prognostic role at 2-year follow-up. Eur. J. Radio. 85, 1366–1374 (2016).
Moss, H. G., Jenkins, D. D., Yazdani, M. & Brown, T. R. Identifying the translational complexity of magnetic resonance spectroscopy in neonates and infants. NMR Biomed. 32, e4089 (2019).
Acknowledgements
All of the infants and families included in this study. Staff of the Brigham and Women’s Hospital.
Author information
Authors and Affiliations
Contributions
A.G., T.I., M.E.-D. made substantial contributions to the conception and design of the study. A.G. and H.E.-S. made substantial contributions to the acquisition of data. A.G., E.Y. and M.E.-D. made significant contributions to the analysis and interpretation of the data. All authors were involved in drafting and revising of the manuscript and approve the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate
Patient consent was not required. This was a retrospective data study and institutional review board approval waived consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Garvey, A.A., El-Shibiny, H., Yang, E. et al. Differences between early and late MRI in infants with neonatal encephalopathy following therapeutic hypothermia. Pediatr Res 94, 1011–1017 (2023). https://doi.org/10.1038/s41390-023-02580-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02580-8
This article is cited by
-
Do we need a brain MRI once or twice in infants treated with hypothermia?
Pediatric Research (2023)