Abstract
Background
The current study evaluated the hypothesis that the COVID-19 pandemic is associated with higher stillbirth but lower neonatal mortality rates.
Methods
We compared three epochs: baseline (2016–2019, January–December, weeks 1–52, and 2020, January–February, weeks 1–8), initial pandemic (2020, March–December, weeks 9–52, and 2021, January–June, weeks 1–26), and delta pandemic (2021, July–September, weeks 27–39) periods, using Alabama Department of Public Health database including deliveries with stillbirths ≥20 weeks or live births ≥22 weeks gestation. The primary outcomes were stillbirth and neonatal mortality rates.
Results
A total of 325,036 deliveries were included (236,481 from baseline, 74,076 from initial pandemic, and 14,479 from delta pandemic period). The neonatal mortality rate was lower in the pandemic periods (4.4 to 3.5 and 3.6/1000 live births, in the baseline, initial, and delta pandemic periods, respectively, p < 0.01), but the stillbirth rate did not differ (9 to 8.5 and 8.6/1000 births, p = 0.41). On interrupted time-series analyses, there were no significant changes in either stillbirth (p = 0.11 for baseline vs. initial pandemic period, and p = 0.67 for baseline vs. delta pandemic period) or neonatal mortality rates (p = 0.28 and 0.89, respectively).
Conclusions
The COVID-19 pandemic periods were not associated with a significant change in stillbirth and neonatal mortality rates compared to the baseline period.
Impact
-
The COVID-19 pandemic could have resulted in changes in fetal and neonatal outcomes.
-
However, only a few population-based studies have compared the risk of fetal and neonatal mortality in the pandemic period to the baseline period.
-
This population-based study identifies the changes in fetal and neonatal outcomes during the initial and delta COVID-19 pandemic period as compared to the baseline period.
-
The current study shows that stillbirth and neonatal mortality rates were not significantly different in the initial and delta COVID-19 pandemic periods as compared to the baseline period.
Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has severely affected health and healthcare systems worldwide,1,2 with unanticipated reductions in emergency room visits,3,4,5 delayed presentation of non-COVID critical diseases,5 and increased morbidity and mortality.6 The pandemic has also led to worse pregnancy-related outcomes, including higher stillbirth and maternal mortality rates.7 Pandemic-related decreases in access to care could lead to a higher stillbirth rate for critically ill fetuses and subsequent paradoxically lower neonatal mortality rate, but this has not been proven.
The current study is a population-based perinatal study with individual participant data that covers the longest duration of the pandemic, including up to the delta pandemic period (September 2021), and is the first to compare the risk of fetal and neonatal mortality in the initial and delta pandemic periods to the baseline period.7 By analyzing the changes in the epidemiology of adverse fetal and neonatal outcomes with demographic and pandemic severity variables, this study may help identify fetuses and neonates at higher risk for adverse outcomes and inform health policy and response-preparedness for the present pandemic and future health care disruptions. This study tested the hypothesis that the COVID-19 pandemic is associated with higher stillbirth but lower neonatal mortality rates.
Methods
Study design and participants
The study was conducted using the Alabama Department of Public Health Center for Health Statistics (ADPH) database, a population-based state vital registry. We compared pregnancies from the following epochs: baseline (2016–2019, January–December, weeks 1–52, with week 1 defined as starting on the first Sunday of the year, and 2020, January–February, weeks 1–8), initial pandemic (2020, March–December, weeks 9–52, and 2021, January–June, week 1–26), and delta pandemic (2021, July–September, weeks 27–39).
All pregnant Alabama state resident women who delivered in Alabama with stillbirths ≥20 weeks or live births ≥22 weeks gestational age were included. The ADPH tabulates health-related statistical data received from healthcare providers from the State and releases yearly data in the second half of the subsequent year. The database definitions were used to define variables and outcomes in the following subsection.8
Outcomes and variable definitions
The primary outcomes were the stillbirth rate and the neonatal mortality rate. Stillbirth was defined as death (no evidence of life) before birth beyond the 20th week of gestation, excluding induced pregnancy termination. Neonatal mortality was defined as the death of a liveborn infant within the first 27 days after birth.8 The adequacy of prenatal care was assessed by Kessner and Kotelchuck indices, which include gestational age at the beginning of prenatal care and the percentage of achieved/expected number of prenatal care visits for gestational age as recommended by the American College of Obstetricians and Gynecologists.8 The race and ethnicity are reported by the parents/health providers that are recorded in the birth/death certificates. The race/ethnicity categories were as per the National Center for Health Statistics classification, and for presentation, the categories were consolidated into four groups: Black, Hispanic, White, and Other.8 The database definitions were used to define other variables and outcomes.8 Centers for Disease Control and Prevention (CDC) daily cases for Alabama9 were used to identify variations in the rate of stillbirth and neonatal mortality by frequency of new COVID-19 cases.
Statistical analysis
Descriptive analyses were used to describe demographics, clinical characteristics, and outcomes. Chi-square, Mann–Whitney U, or Student’s t tests were used, as appropriate, to compare characteristics between the baseline and pandemic periods. CDC daily cases for Alabama9 were used to identify variations in outcomes by frequency of new COVID-19 cases. We performed an interrupted time-series analysis for the outcomes of stillbirths per 1000 births and neonatal mortality per 1000 live births for the monthly data from March 2016 to September 2021.10 We employed Box and Jenkins’s autoregressive integrated moving average (ARIMA) models to identify and model any possible seasonality and trend of the monthly outcomes.11 For both the stillbirths and neonatal mortality, we used 50 baseline month periods from January 2016 to February 2020, to identify and model autocorrelations using “Proc ARIMA” procedure from SAS. We then performed the ARIMA model (with fixed estimated parameters those obtained for the 50 baseline month periods) for the 69 months of data and added a categorical pandemic onset variable (coded as 0 for the baseline period, 1 for the initial pandemic period, and 2 for the delta pandemic period, which is equivalent to defining two dummy binary variables: one for the initial pandemic period and the other for the delta pandemic period) as a predictor to the best fitting ARIMA model to estimate the pandemic onset effects on the outcomes. We estimated expected monthly outcomes with their 95% prediction interval, and any observed outcome outside of the interval can be considered unusual. The residuals of the final models satisfy the auto-correlational test of independence of monthly observations, and the expected value of zero. We also correlated the change in the incidence of stillbirths and neonatal mortality over time with social distancing as measured by Alabama’s state-specific social distancing index (SDI, available for the year 2020), defined as the extent to which residents of the state practiced social distancing, computed from six mobility metrics (including % staying home, % reduction of all trips compared to pre-COVID-19 benchmark, % reduction of work trips, % reduction of non-work trips, % reduction of travel distance, and % reduction of out-of-county trips, available from https://data.covid.umd.edu).12 In addition, multivariable logistic regression analyses were performed to identify risk factors associated with stillbirth, adjusting for socio-demographic variables (maternal race, age, education, and prenatal care) and their interactions with the pandemic period. All hypotheses were two-tailed, and a p value <0.05 was used to indicate statistical significance. All analyses were performed in SAS (version 9.4, Cary, NC). The study was approved by the institutional review board and is reported using the STROBE guidelines for reporting observational studies.13
Results
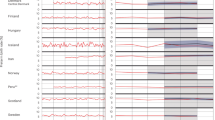
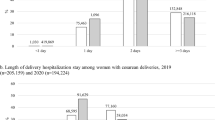
All 325,036 pregnancies were included: 236,481 were from the baseline period, 74,076 were from the initial pandemic period, and 14,479 were from the delta pandemic period (Table 1). The neonatal mortality rate was lower in the pandemic periods (4.4 to 3.5 and 3.6/1000 live births in the baseline, initial pandemic, and delta pandemic periods, respectively, p < 0.01), but the stillbirth rate did not differ (9 to 8.5 and 8.6/1000 births, in the baseline, initial pandemic, and delta pandemic periods, respectively, p = 0.41, Table 1, Fig. 1, and Supplementary Fig. 1). The pandemic periods were associated with changes in important clinical characteristics like a higher percentage of prenatal steroid coverage in preterm live births (<34 weeks gestational age at delivery), and a higher percentage of infants needing neonatal intensive care unit (NICU) admission (Table 1).
On ARIMA model analysis, there were no significant changes in either stillbirth (p = 0.11 for baseline vs. initial pandemic period, and p = 0.67 for baseline vs. delta pandemic period) or neonatal mortality rates (p = 0.28 for baseline vs. initial pandemic period, and p = 0.89 for baseline vs. delta pandemic period). The ARIMA model (Table 2) shows that all of the observed monthly stillbirth rates (19/19 months) and all except one neonatal mortality rate (18/19 months) fell within the 95% prediction interval of the expected rate.
The SDI was not significantly cross-correlated with the percent change of stillbirths (coefficient = 0.12, 95% CI = −0.32 to 0.51, p = 0.60) and neonatal mortality (coefficient = −0.09, 95% CI = −0.50 to 0.34, p = 0.69, Fig. 2). On multivariable logistic regression (adjusting for socio-demographic variables), only maternal age was found to be associated with stillbirths (Supplementary Table 1).
Discussion
The current population-based study shows that considering the outcome trends over the study period, there was no change in the stillbirth and neonatal mortality rates in the COVID-19 pandemic periods. This finding could possibly be reflective of the resiliency of the perinatal healthcare system and the public health interventions during the pandemic period, including improved hand hygiene, social distancing, masking, and others.
No significant change in the stillbirth rate was also found in a meta-analysis of shorter duration studies from high-income countries that reported perinatal outcomes in the pandemic period.7 In this meta-analysis, there was a single study from a high-income country (UK) that used population-based data and compared the stillbirth rate in the pandemic to the baseline period14, similar to the findings of the current study, the population-based study from the UK reported no significant change in stillbirth rate in the pandemic to baseline period.
In contrast to the current study findings, of an increase in moderately preterm births, other shorter duration population-based studies have shown a decrease15,16 or no change17 in the rates of preterm birth. To our knowledge, there are no population-based studies and only one single-center study from a high-income country (Ireland) that has reported the outcome of neonatal mortality comparing the pandemic to the baseline period18. This relatively small sample size study also found no difference in the neonatal mortality rate in the pandemic compared to the baseline period. In contrast to the current study showing an increase in the NICU admission rate, the meta-analysis of single-center studies showed no significant change in NICU admission rate in the pandemic compared to the baseline period.7 As the studies that have assessed NICU admission rates are single-center studies of shorter duration, the meta-analysis of these studies may have limited generalizability.
To our knowledge, the current study is the first to analyze the association of state-specific SDI, which combines several factors indicating the severity of pandemic-related mobility restrictions and population-level behavioral changes, with the changes in stillbirth and neonatal mortality percentages. Similar studies with in-depth analyses of pandemic-related objective measures can help identify interventions that can be further studied for reducing the risk of adverse fetal and neonatal outcomes as possible mitigation measures during and beyond the current pandemic.
The limitations of the current study include first that it is based on single-state data and second, that COVID-19 test results for individual participants were not available in the database, so we were unable to compare the fetal and neonatal outcomes in COVID-19 infected and non-infected pregnancies. The current study findings address important knowledge gaps and complement the evidence from previously published studies. As the study is population-based, covers the longest duration of the pandemic, and is the first to compare initial and delta pandemic periods to the baseline period, the current study will have better generalizability.
Conclusions
The current population-based study showed that there was no significant change in the stillbirth and neonatal mortality rates in the COVID-19 pandemic periods. The findings from the current study may inform strategies to mitigate the effects of the current pandemic on this vulnerable population.
Data availability
Data from the study are available at request from the Alabama Department of Public Health: www.alabamapublichealth.gov.
References
White, D. B. & Lo, B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. JAMA 323, 1773–1774 (2020).
Blumenthal, D., Fowler, E. J., Abrams, M. & Collins, S. R. Covid-19 - implications for the health care system. N. Engl. J. Med. 383, 1483–1488 (2020).
Rosenbaum, L. Facing Covid-19 in Italy - ethics, logistics, and therapeutics on the epidemic’s front line. N. Engl. J. Med. 382, 1873–1875 (2020).
Hartnett, K. P. et al. Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019-May 30, 2020. MMWR Morb. Mortal. Wkly Rep. 69, 699–704 (2020).
Lange, S. J. et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions - United States, January-May 2020. MMWR Morb. Mortal. Wkly Rep. 69, 795–800 (2020).
Rosenbaum, L. The untold toll - the pandemic’s effects on patients without Covid-19. N. Engl. J. Med. 382, 2368–2371 (2020).
Chmielewska, B. et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob. Health 9, e759–e772 (2021).
Shen, X. Alabama vital statistics 2018. https://www.alabamapublichealth.gov/healthstats/assets/AVS2018.pdf (2018).
CDC. Trends in number of COVID-19 cases and deaths in the US reported to CDC, by state/territory. https://covid.cdc.gov/covid-data-tracker/#trends_dailycases (2021).
Bernal, J. L., Cummins, S. & Gasparrini, A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int. J. Epidemiol. 46, 348–355 (2017).
Box, G., Jenkins, G. & Reinsel, G. Time Series Analysis: Forecasting and Control 4th edn (Wiley, 2008).
Zhang, L. et al. An interactive covid-19 mobility impact and social distancing analysis platform. Transportation Res. Rec. https://doi.org/10.1177/03611981211043813 (2021).
von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370, 1453–1457 (2007).
Stowe, J. et al. Stillbirths during the COVID-19 pandemic in England, April-June 2020. JAMA 325, 86–87 (2021).
Been, J. V. et al. Impact of COVID-19 mitigation measures on the incidence of preterm birth: a national quasi-experimental study. Lancet Public Health 5, e604–e611 (2020).
Hedermann, G. et al. Danish premature birth rates during the COVID-19 lockdown. Arch. Dis. Child. Fetal Neonatal Ed. 106, 93–95 (2021).
Main, E. K. et al. Singleton preterm birth rates for racial and ethnic groups during the coronavirus disease 2019 pandemic in California. Am. J. Obstet. Gynecol. 224, 239–241 (2021).
McDonnell, S., McNamee, E., Lindow, S. W. & O’Connell, M. P. The impact of the Covid-19 pandemic on maternity services: a review of maternal and neonatal outcomes before, during and after the pandemic. Eur. J. Obstet. Gynecol. Reprod. Biol. 255, 172–176 (2020).
Acknowledgements
We would like to thank the Perinatal Health and Human Development Research Program of the University of Alabama at Birmingham and the Children’s of Alabama Centennial Scholar Fund for support.
Author information
Authors and Affiliations
Contributions
V.V.S. conceptualized the study, developed the initial study protocol, conducted the analyses, drafted the initial manuscript, and participated in manuscript editing and revision. A.K.M.F.R. and X.S. developed the initial study protocol, conducted the analyses, and participated in manuscript editing and revision. A.B., C.Z., N. A., and W.A.C. conceptualized the study, developed the initial study protocol, and participated in manuscript editing and revision. N.A., C.V.L., E.F.B., and A.N. developed the initial study protocol and participated in manuscript editing and revision. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
W.A.C. is on the board of directors of MEDNAX Services, Inc. All other authors have indicated that they have no conflicts of interest relevant to this article to disclose.
Ethics approval and consent to participate
This study was reviewed and approved by University of Alabama at Birmingham Institutional. Review Board and was granted a waiver of informed consent as the study was based on a deidentified public health database (IRB-300006594).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shukla, V.V., Rahman, A.K.M.F., Shen, X. et al. Trends in fetal and neonatal outcomes during the COVID-19 pandemic in Alabama. Pediatr Res 94, 756–761 (2023). https://doi.org/10.1038/s41390-023-02533-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02533-1
This article is cited by
-
ECI Bio-commentary: Vivek V. Shukla
Pediatric Research (2023)