Abstract
Background
The aim of the study was to determine whether prolonged exposure to a moderate/large patent ductus arteriosus left-to-right shunt (PDA) increases the risk of late (beyond 36 weeks) pulmonary hypertension (BPD-PH) and pulmonary vascular disease (BPD-PVD) during the neonatal hospitalization in preterm infants (<28 weeks’ gestation) with bronchopulmonary dysplasia (BPD).
Methods
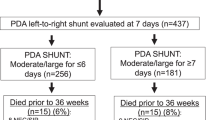
All infants requiring respiratory support ≥36 weeks had systematic echocardiographic evaluations for BPD-PH at planned intervals. Infants were classified as having either flow-associated BPD-PH (BPD-flow-PH) or BPD-PVD.
Results
256 infants survived ≥36 weeks: 105 had NO BPD (were off respiratory support by 36 weeks); 151 had BPD. 22/151 had BPD-PH (12/22 had BPD-flow-PH from a PDA that persisted beyond 36 weeks; 10/22 had BPD-PVD). Moderate/large PDA shunts that persisted beyond 36 weeks were significantly associated with an increased incidence of BPD-PH due to BPD-flow-PH. We found no association between the duration of PDA exposure and the incidence of BPD-PVD.
Conclusions
Moderate/large PDA shunts increase the risk of flow-associated BPD-PH when present beyond 36 weeks. Although term infants with PDA-congenital heart disease can develop pulmonary vascular remodeling and PVD after months of PDA exposure, we found no echocardiographic evidence in preterm infants that prolonged PDA exposure increases the incidence of BPD-PVD during the neonatal hospitalization.
Impact
-
In our study, preterm infants (<28 weeks’ gestation) with bronchopulmonary dysplasia (BPD) had a 15% incidence of pulmonary hypertension (PH) beyond 36 weeks’ postmenstrual age as a comorbidity.
-
Moderate/large patent ductus arteriosus (PDA) shunts increased the risk of flow-associated PH when present beyond 36 weeks.
-
Although months of prolonged PDA exposure can cause pulmonary vascular remodeling and pulmonary vascular disease (PVD) in term infants with PDA-congenital heart disease, we found no echocardiographic evidence for an association between the duration of PDA exposure and the incidence of late PVD during the neonatal hospitalization in preterm infants with BPD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Ehrenkranz, R. A. et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics 116, 1353–1360 (2005).
Walsh, M. C. et al. Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics 114, 1305–1311 (2004).
Shennan, A. T., Dunn, M. S., Ohlsson, A., Lennox, K. & Hoskins, E. M. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics 82, 527–532 (1988).
Jensen, E. A. et al. The diagnosis of bronchopulmonary dysplasia in very preterm infants. an evidence-based approach. Am. J. Respir. Crit. Care Med. 200, 751–759 (2019).
Khemani, E. et al. Pulmonary artery hypertension in formerly premature infants with bronchopulmonary dysplasia: clinical features and outcomes in the surfactant era. Pediatrics 120, 1260–1269 (2007).
Bhat, R., Salas, A. A., Foster, C., Carlo, W. A. & Ambalavanan, N. Prospective analysis of pulmonary hypertension in extremely low birth weight infants. Pediatrics 129, e682–e689 (2012).
Bland, R. D. et al. Chronic lung injury in preterm lambs: abnormalities of the pulmonary circulation and lung fluid balance. Pediatr. Res. 48, 64–74 (2000).
Hocq, C. et al. Early diagnosis and targeted approaches to pulmonary vascular disease in bronchopulmonary dysplasia. Pediatr. Res. 91, 804–815 (2022).
Pierro, M. et al. Association of the dysfunctional placentation endotype of prematurity with bronchopulmonary dysplasia: a systematic review, meta-analysis and meta-regression. Thorax 77, 268–275 (2022).
Parker, T. A. & Abman, S. H. The pulmonary circulation in bronchopulmonary dysplasia. Semin. Neonatol. 8, 51–61 (2003).
Nagiub, M., Kanaan, U., Simon, D. & Guglani, L. Risk factors for development of pulmonary hypertension in infants with bronchopulmonary dysplasia: systematic review and meta-analysis. Paediatr. Respir. Rev. 23, 27–32 (2017).
Chen, Y. et al. Risk factors and outcomes of pulmonary hypertension in infants with bronchopulmonary dysplasia: a meta-analysis. Front. Pediatr. 9, 695610 (2021).
Arjaans, S. et al. Identification of gaps in the current knowledge on pulmonary hypertension in extremely preterm infants: a systematic review and meta-analysis. Paediatr. Perinat. Epidemiol. 32, 258–267 (2018).
Clyman, R. I., Mauray, F., Heymann, M. A. & Roman, C. Cardiovascular effects of a patent ductus arteriosus in preterm lambs with respiratory distress. J. Pediatr. 111, 579–587 (1987).
Alpan, G., Scheerer, R., Bland, R. D. & Clyman, R. Patent ductus arteriosus increases lung fluid filtration in preterm lambs. Pediatr. Res. 30, 616–621 (1991).
Diller, G. P. & Gatzoulis, M. A. Pulmonary vascular disease in adults with congenital heart disease. Circulation 115, 1039–1050 (2007).
D'Alto, M. & Mahadevan, V. S. Pulmonary arterial hypertension associated with congenital heart disease. Eur. Respir. Rev. 21, 328–337 (2012).
Liebowitz, M. & Clyman, R. I. Prophylactic indomethacin compared with delayed conservative management of the patent ductus arteriosus in extremely preterm infants: effects on neonatal outcomes. J. Pediatr. 187, 119–126 (2017).
Jhaveri, N., Moon-Grady, A. & Clyman, R. I. Early surgical ligation versus a conservative approach for management of patent ductus arteriosus that fails to close after indomethacin treatment. J. Pediatr. 157, 381–387 (2010).
El Hajjar, M., Vaksmann, G., Rakza, T., Kongolo, G. & Storme, L. Severity of the ductal shunt: a comparison of different markers. Arch. Dis. Child. Fetal Neonatal Ed. 90, F419–F422 (2005).
Koch, J. et al. Prevalence of spontaneous closure of the ductus arteriosus in neonates at a birth weight of 1000 grams or less. Pediatrics 117, 1113–1121 (2006).
Clyman, R. I. et al. PDA-TOLERATE Trial: an exploratory randomized controlled trial of treatment of moderate-to-large patent ductus arteriosus at 1 week of age. J. Pediatr. 205, 41–48 (2019).
Abman, S. H. et al. Pediatric pulmonary hypertension: guidelines from the American Heart Association and American Thoracic Society. Circulation 132, 2037–2099 (2015).
Krishnan, U. et al. Evaluation and management of pulmonary hypertension in children with bronchopulmonary dysplasia. J. Pediatr. 188, 24.e1–34.e1 (2017).
Berkelhamer, S. K., Mestan, K. K. & Steinhorn, R. An update on the diagnosis and management of bronchopulmonary dysplasia (BPD)-associated pulmonary hypertension. Semin. Perinatol. 42, 432–443 (2018).
Hansmann, G. et al. Pulmonary hypertension in bronchopulmonary dysplasia. Pediatr. Res. 89, 446–455 (2021).
Nawaytou, H. et al. Clinical utility of echocardiography in former preterm infants with bronchopulmonary dysplasia. J. Am. Soc. Echocardiogr. 33, 378.e1–388.e1 (2020).
Fenton, T. R. & Kim, J. H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 13, 59 (2013).
Papile, L. A., Burstein, J., Burstein, R. & Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weight <1500 grams. J. Pediatr. 92, 529–534 (1978).
Bell, M. J. et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann. Surg. 187, 1–7 (1978).
Mourani, P. M., Sontag, M. K., Younoszai, A., Ivy, D. D. & Abman, S. H. Clinical utility of echocardiography for the diagnosis and management of pulmonary vascular disease in young children with chronic lung disease. Pediatrics 121, 317–325 (2008).
McCrary, A. W. et al. Agreement of an echocardiogram-based diagnosis of pulmonary hypertension in infants at risk for bronchopulmonary dysplasia among masked reviewers. J. Perinatol. 39, 248–255 (2019).
Ge, Z. M. et al. Reliability and accuracy of measurement of transductal gradient by Doppler ultrasound. Int. J. Cardiol. 40, 35–43 (1993).
Groh, G. K. et al. Doppler echocardiography inaccurately estimates right ventricular pressure in children with elevated right heart pressure. J. Am. Soc. Echocardiogr. 27, 163–171 (2014).
Acknowledgements
We would like to thank Dr. Mark Cocalis, Dr. Michael Brook, Dr. Anita Moon-Grady, Dr. Shabnam Peyvandi, Dr. Nicole Cresalia, Dr. Kavitha Pundi, Dr. Shafkat Anwar, and Dr. Emilio Quezada for their expert help in reading and interpreting the echocardiograms and to the neonatal faculty, fellows, nurses, respiratory therapists, and dieticians for their excellent care and their commitment to the nursery’s quality improvement projects and its consensus-driven protocols.
Funding
This work was supported by a grant from U.S. Public Health Service NHLBI (HL109199) and by gifts from the Clyman Family Foundation.
Author information
Authors and Affiliations
Contributions
The following authors have made the following contributions: (1) H.N., N.K.H., and R.I.C. made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; (2) H.N., N.K.H., and R.I.C. have drafted the article or revised it critically for important intellectual content; and (3) H.N., N.K.H., and R.I.C. have given final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The requirement for individual Research HIPAA Authorization was waived by the Institutional Review Board of the University of California San Francisco.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nawaytou, H., Hills, N.K. & Clyman, R.I. Patent ductus arteriosus and the risk of bronchopulmonary dysplasia-associated pulmonary hypertension. Pediatr Res 94, 547–554 (2023). https://doi.org/10.1038/s41390-023-02522-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02522-4