Abstract
Objective
To demonstrate the association between the duration of significant patent ductus arteriosus (PDA) and bronchopulmonary dysplasia (BPD) in extremely preterm infants.
Methods
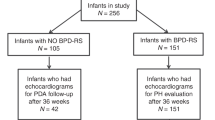
All extremely preterm infants (<29 weeks) treated in our Neonatal Intensive Care Unit from January 2013 to March 2016 were included if their PDA status was confirmed at <7 days of life. Infants with genetic syndromes, complex congenital anomalies and insignificant PDAs were excluded. Total duration of significant PDA was estimated by reviewing serial echocardiograms. Significant PDA was diagnosed using our scoring system that was based upon echocardiographic parameters and clinical status of the infants. Study cohort was divided into four groups based on the duration of significant PDA. Group A-No PDA, Group B-PDA <1-week, Group C- PDA 1–2 weeks, and Group D-PDA >2 weeks. ANOVA and multivariate analysis were performed to compare the groups.
Results
There were 147 infants with no PDA (Group A), 50, 35, and 41 infants were enrolled in Groups B, C, and D, respectively. There were no differences in maternal and neonatal variables among groups except for the following: maternal smoking, chorioamnionitis, antenatal indomethacin, gestation, birth weight, mode of delivery and incidence of death or BPD. Logistic regression analysis showed that longer duration of significant PDA was associated with higher risk for death or BPD (adjusted OR 1.37, 95% CI 1.03–1.82).
Conclusion
Longer duration of significant PDA is associated with the higher risk for BPD/death in extremely preterm infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Schena F, Francescato G, Cappelleri A, Picciolli I, Mayer A, Mosca F, et al. Association between hemodynamically significant patent ductus arteriosus and bronchopulmonary dysplasia. J Pediatr. 2015;166:1488–92.
Hermes-DeSantis ER, Clyman RI. Patent ductus arteriosus: pathophysiology and management. J Perinatol. 2006;26(Suppl 1):S14–18.
Tsui I, Ebani E, Rosenberg JB, Lin J, Angert RM, Mian U. Patent ductus arteriosus and indomethacin treatment as independent risk factors for plus disease in retinopathy of prematurity. J Pediatr Ophthalmol strabismus. 2013;50:88–92.
Mirea L, Sankaran K, Seshia M, Ohlsson A, Allen AC, Aziz K, et al. Treatment of patent ductus arteriosus and neonatal mortality/morbidities: adjustment for treatment selection bias. J pediatrics. 2012;161:689–94 e681.
Madan JC, Kendrick D, Hagadorn JI, Frantz ID,3rd, National Institute of Child Health and Human Development Neonatal Research Networ Patent ductus arteriosus therapy: impact on neonatal and 18-month outcome. Pediatrics. 2009;123:674–81.
Clyman R, Cassady G, Kirklin JK, Collins M, Philips JB 3rd. The role of patent ductus arteriosus ligation in bronchopulmonary dysplasia: reexamining a randomized controlled trial. J pediatrics. 2009;154:873–6.
Abdel-Hady H, Nasef N, Shabaan AE, Nour I. Patent ductus arteriosus in preterm infants: do we have the right answers? BioMed Res Int. 2013;2013:676192.
Letshwiti JB, Semberova J, Pichova K, Dempsey EM, Franklin OM, Miletin J. A conservative treatment of patent ductus arteriosus in very low birth weight infants. Early Hum Dev. 2017;104:45–49.
McNamara PJ, Sehgal A. Towards rational management of the patent ductus arteriosus: the need for disease staging. Arch Dis Child Fetal Neonatal Ed. 2007;92:F424–427.
Sehgal A, Paul E, Menahem S. Functional echocardiography in staging for ductal disease severity: role in predicting outcomes. Eur J pediatrics. 2013;172:179–84.
Fink D, El-Khuffash A, McNamara PJ, Nitzan I, Hammerman C. Tale of two patent ductus arteriosus severity scores: similarities and differences. Am J Perinatol. 2018;35:55–58.
El-Khuffash A, James AT, Corcoran JD, Dicker P, Franklin O, Elsayed YN, et al. A patent ductus arteriosus severity score predicts chronic lung disease or death before discharge. J Pediatr. 2015;167:1354–61 e1352.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
Kliegman RM, Walsh MC. Neonatal necrotizing enterocolitis: pathogenesis, classification, and spectrum of illness. Curr Probl Pediatr. 1987;17:213–88.
Liebowitz M, Clyman RI. Prophylactic indomethacin compared with delayed conservative management of the patent ductus arteriosus in extremely preterm infants: effects on neonatal outcomes. J Pediatr. 2017;187:119–26 e111.
Youn Y, Moon CJ, Lee JY, Lee C, Sung IK. Timing of surgical ligation and morbidities in very low birth weight infants. Med (Baltim). 2017;96:e6557.
Yeh TF, Raval D, Luken J, Thalji A, Lilien L, Pildes RS. Clinical evaluation of premature infants with patent ductus arteriosus: a scoring system with echocardiogram, acid-base, and blood gas correlations. Crit Care Med. 1981;9:655–7.
Taylor GA. Effect of scanning pressure on intracranial hemodynamics during transfontanellar duplex US. Radiology. 1992;185:763–6.
Couture A, Veyrac C. Transfontanellar Doppler imaging in neonates. Berlin, New York: Springer; 2001.
Deeg KH, Worle K, Wolf A. [Doppler sonographic estimation of normal values for flow velocity and resistance indices in renal arteries of healthy infants]. Ultraschall der Med. 2003;24:312–22.
Harkin P, Marttila R, Pokka T, Saarela T, Hallman M. Morbidities associated with patent ductus arteriosus in preterm infants. Nationwide cohort study J Matern Fetal Neonatal Med. 2018;31:2576–83.
Chock VY, Punn R, Oza A, Benitz WE, Van Meurs KP, Whittemore AS, et al. Predictors of bronchopulmonary dysplasia or death in premature infants with a patent ductus arteriosus. Pediatr Res. 2014;75:570–5.
Funding
AdventHealth for Children.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mirza, H., Garcia, J., McKinley, G. et al. Duration of significant patent ductus arteriosus and bronchopulmonary dysplasia in extremely preterm infants. J Perinatol 39, 1648–1655 (2019). https://doi.org/10.1038/s41372-019-0496-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0496-5
This article is cited by
-
Impact of patent ductus arteriosus on non-invasive assessments of lung fluids in very preterm infants during the transitional period
European Journal of Pediatrics (2023)
-
Comparison of lung ultrasound scores with clinical models for predicting bronchopulmonary dysplasia
European Journal of Pediatrics (2023)
-
Effects of prophylactic indomethacin on morbidity and mortality in infants <25 weeks’ gestation: a protocol driven intention to treat analysis
Journal of Perinatology (2022)
-
Patent ductus arteriosus, tracheal ventilation, and the risk of bronchopulmonary dysplasia
Pediatric Research (2022)
-
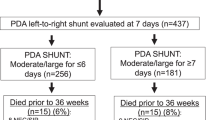
Impact of patent ductus arteriosus shunt size and duration on risk of death or severe respiratory morbidity in preterm infants born in China
European Journal of Pediatrics (2022)