Abstract
Background
Tobacco smoke exposure increases the risk and severity of lower respiratory tract infections in children, yet the mechanisms remain unclear. We hypothesized that tobacco smoke exposure would modify the lower airway microbiome.
Methods
Secondary analysis of a multicenter cohort of 362 children between ages 31 days and 18 years mechanically ventilated for >72 h. Tracheal aspirates from 298 patients, collected within 24 h of intubation, were evaluated via 16 S ribosomal RNA sequencing. Smoke exposure was determined by creatinine corrected urine cotinine levels ≥30 µg/g.
Results
Patients had a median age of 16 (IQR 568) months. The most common admission diagnosis was lower respiratory tract infection (53%). Seventy-four (20%) patients were smoke exposed and exhibited decreased richness and Shannon diversity. Smoke exposed children had higher relative abundances of Serratia spp., Moraxella spp., Haemophilus spp., and Staphylococcus aureus. Differences were most notable in patients with bacterial and viral respiratory infections. There were no differences in development of acute respiratory distress syndrome, days of mechanical ventilation, ventilator free days at 28 days, length of stay, or mortality.
Conclusion
Among critically ill children requiring prolonged mechanical ventilation, tobacco smoke exposure is associated with decreased richness and Shannon diversity and change in microbial communities.
Impact
-
Tobacco smoke exposure is associated with changes in the lower airways microbiome but is not associated with clinical outcomes among critically ill pediatric patients requiring prolonged mechanical ventilation.
-
This study is among the first to evaluate the impact of tobacco smoke exposure on the lower airway microbiome in children.
-
This research helps elucidate the relationship between tobacco smoke exposure and the lower airway microbiome and may provide a possible mechanism by which tobacco smoke exposure increases the risk for poor outcomes in children.
Similar content being viewed by others
Introduction
Tobacco smoke exposure (TSE) contributes to an estimated 168,000 pediatric deaths per year worldwide, primarily attributed to increasing the incidence and severity of lower respiratory tract infections (LRTI).1,2 In the United States, 38.1% of children are exposed to tobacco smoke.3 TSE is associated with increased healthcare utilization and the risk of LRTI, otitis media, sinusitis, asthma, and obesity.4,5,6,7 Tobacco smoke exposed children with influenza are more likely to require intubation and admission to the pediatric intensive unit (PICU) with increased lengths of stay compared to those without TSE.8 TSE is associated with increased hospitalization and severity of illness in children with respiratory syncytial virus (RSV).9
The association between TSE and increased risk of critical illness has been recognized in adults. Among adult patients with non-pulmonary sepsis, current smokers were twice as likely to develop acute respiratory distress syndrome (ARDS). Despite being younger with fewer comorbidities and lower severity of disease than patients without TSE, patients with TSE had similar severity of lung injury, suggesting that TSE may increase the risk of ARDS in younger, healthier patients.10,11
The molecular basis of TSE-associated health risks includes broad effects on lung inflammation, immune response, infection response, and tissue damage.12 Recent studies suggest that these effects may in part be mediated by or result in changes in the respiratory tract microbiome.13,14,15 Among critically ill adults with severe blunt trauma, those with TSE had increased relative abundance of Haemophilus spp., Streptococcus spp., and Fusobacterium spp. in the lower airways, which persisted after 48 h of invasive mechanical ventilation. Furthermore, microbial changes associated with TSE, specifically enrichment of Enterobacteriaceae, were associated with development of ARDS.16
Children most often experience secondary exposure from inhalation of smoke from someone else using cigarettes or tertiary smoke exposure from clothing and other surfaces. Therefore, investigations of the relationship between TSE and critical illness are warranted in this population.
In a secondary analysis of a prospective multicenter cohort of critically ill children requiring prolonged ventilation, we evaluated the association between TSE, the lower respiratory tract microbiome, and clinical outcomes. We hypothesized that children with TSE would have a microbiome characterized by higher bacterial burden, decreased bacterial diversity, and increased relative abundance of pathogenic bacteria, and worse clinical outcomes.
Methods
Data and specimens for this study were collected as part of a prospective cohort study of mechanically ventilated children admitted to eight PICUs in the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s Collaborative Pediatric Critical Care Research Network from 2015 to 2017.17 Children 31 days to 18 years requiring endotracheal intubation and mechanical ventilation for >72 h were eligible. For this study, we analyzed data from patients who had a urine sample collected and 16 S rRNA sequencing data from a tracheal aspirate obtained the day of intubation.
The study was approved by the University of Utah central Institutional Review Board. Full details of the consent process, study methodology, and data collection have been previously published.17
Tracheal aspirates were collected within 24 h of intubation according to a standardized protocol and frozen at −80 °C until analyzed.17 Urine was collected within 96 h of intubation from an indwelling foley catheter, bed pans, other urine receptacles, or cotton balls. After collection, samples were frozen at −80 °C.
Laboratory analysis
Tracheal aspirates underwent 16 S rRNA gene sequencing to evaluate the lower airway microbiome; full methods have been previously described.17,18,19,20 The relative abundance of each taxon was calculated (number of sequences for specific taxon/total number of sequences*100). Shannon diversity and evenness indices were used to characterize the bacterial community.
To determine TSE, urine was analyzed for total urinary cotinine content through the Human Health Exposure Analysis Resource21 via liquid chromatography-tandem mass spectrometry assay as previously described.22 The lower limit of detection was 0.1 ng/mL. To account for urinary dilution and changes in glomerular filtration across age and critical illness severity, raw cotinine levels were corrected for creatinine concentration using the following formula: cotinine (ng/mL)/creatinine (mg/dL).23 To account for a right skew, creatinine-corrected cotinine was log2 transformed and is reported as µg cotinine/g creatinine.
Statistical analysis
The main exposure, creatinine corrected cotinine level, was defined two ways: (1) binary variable using a threshold of ≥30 µg/g24,25,26,27,28,29 and (2) continuous variable adjusted for time of collection from hospital admission. Log linear regression assessed the relationship between TSE and total bacterial load, richness, and Shannon diversity. For subgroup analyses, patients were classified based on clinical data and laboratory results as bacterial LRTI, viral LRTI (either viral only or combined viral and bacterial), clinical LRTI (pathogen not identified), or non-infectious etiology of respiratory failure (additional details in online supplement). Relative abundance from 16 S rRNA gene sequencing for known pathogens30 between TSE and no TSE groups was assessed using Wilcoxon rank sums. Species-level data were available for a subset of organisms; otherwise, taxa are reported at the genus level, the most specific taxonomic rank available.
Log linear regression and logistic regression models evaluated the association of clinical outcomes for continuous and binary outcome TSE variables, respectively. Clinical outcomes of interest were diagnosis of ARDS based on Berlin criteria,31 duration of invasive mechanical ventilation, ventilator free days to day 28, PICU length of stay (LOS), hospital LOS, and mortality. Covariates chosen a priori for the final model were Pediatric Risk of Mortality (PRISM) Score III,32 comorbidities, and baseline dependence on non-invasive ventilation.
A sensitivity analysis was performed excluding the 88 patients that had parental or self-reported TSE but urine creatinine corrected cotinine levels <30 µg/g (additional details in online supplement).
Results
Of the 454 analyzable patients in the parent study, 362 (80%) had urine samples obtained. All 362 patients had tracheal aspirate samples from the day of intubation that were evaluated for total bacterial load. However, only 298 (66%) patients had tracheal aspirate samples with sufficient bacterial load to generate 16 S rRNA gene sequencing data for analysis of richness and Shannon diversity.17,33 The median age was 16 months (IQR 5–68) and 59% were male (Table 1). The most common primary diagnosis was LRTI (53%) and the median PRISM III score was 5 (IQR 1–10). Antibiotics were administered to 36% of patients in the seven days prior to admission, and 99.7% of patients received antibiotics on the day of intubation. There was no significant difference among patients with TSE and no TSE comparing clinical microbiology results available within the first 48 h of admission (Supplementary Table 1). Urine creatinine corrected cotinine levels ranged from 0.1 to 663 µg/g (median 5, IQR: 1, 22 µg/g) and median time to collection was 1.78 days from admission (IQR 1.04, 2.74 days). Seventy-four (20%) patients had urinary cotinine levels ≥30 µg/g, a threshold established to represent TSE.24,25,26,27,34 Based on parental reporting, 138 (38%) of the cohort had passive TSE (97.1%) or the patient actively smoked cigarettes (2.9%). Twenty-four (11%) patients who had no parental report of TSE had evidence of TSE based on creatinine corrected urine cotinine levels. In contrast, 88 (64%) of the patients who had parental reporting of TSE, had no evidence of TSE based on cotinine measurement. The median length of intubation was 7 days (IQR 5–10 days), median PICU LOS was 10 days (IQR 7–15 days), and median hospital LOS was 17 days (IQR 12–29 days). Ninety-seven (27%) developed ARDS and 7 (6%) patients died.
Cotinine and lower respiratory tract microbiome
Among the entire cohort, binary analysis, defining TSE using a creatinine corrected cotinine cutoff of levels ≥30 µg/g, demonstrated that those with TSE had a greater, but not statistically significant, bacterial load (p = 0.06). However, urine cotinine levels were not associated with total bacterial load on continuous cotinine designation (Fig. 1A, D). TSE, based on the binary definition, was associated with significantly lower (p < 0.01) richness but showed no association with richness in the analysis based on the continuous cotinine measurements (Fig. 1B, E). Patients with TSE defined as a binary variable had on average 31.1% less richness than those who were not smoke exposed (Table 2). Shannon diversity was significantly lower among children with TSE in the binary (p < 0.01) and the continuous measure (p = 0.02) analyses (Fig. 1C, F). Patients with TSE had on average 52.7% decrease in Shannon diversity than those without TSE (Table 2).
Box plot a–c compare total bacterial load, richness and Shannon diversity between patients with TSE defined as creatinine adjusted urine cotinine level ≥30 µg/g creatinine to patients without TSE. Scatter plot d–f evaluate the respective metrics using creatinine adjusted urine cotinine as a continuous measure accounting for time of sample collection. Age of individual patients in months is denoted by color of symbol. TSE tobacco smoke exposure.
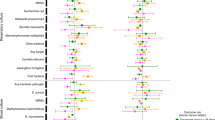
On average, patients with TSE had higher relative abundance of Serratia spp, Moraxella spp., Haemophilus spp, and Staphylococcus aureus while patients without TSE were found to have higher relative abundance of Mycoplasma spp., Fusobacterium spp., Escherichia spp., Streptococcus pyogenes, Streptococcus mitis group, Streptococcus anginous, and Pseudomonas aeruginosa (Fig. 2).
Among patients diagnosed with a bacterial LRTI (n = 43), there was no difference in total bacterial load between the patients with and without TSE. However, patients with bacterial LRTI and TSE had significantly lower richness (p = 0.03) and Shannon diversity (p = 0.02) (Fig. 3, n = 33). Patients with bacterial LRTI and TSE demonstrated higher relative abundance of Moraxella spp. Those with a diagnosis of bacterial LRTI without TSE had an increase in Streptococcus spp. For taxa identified at the species level, those with TSE had a higher relative abundance of S. aureus. Non TSE patients had higher relative abundance of S. pyogenes, S. mitis group, S. anginous, and P. aeruginosa (Fig. 4).
Box plots comparing total bacterial load (a), Richness (b), and Shannon diversity (c) between patients with bacterial LRTI, viral LRTI, clinically diagnosed LRTI, and non-infectious diagnosis based on TSE status in each group using binary comparison of urine cotinine level ≥ 30 µg/g creatinine. Numbers of patients included in each comparison are listed below each box plot. LRTI lower respiratory tract infection, TSE tobacco smoke exposure.
Patients with viral LRTI (n = 117) demonstrated no differences in total bacterial load based on TSE. However, patients with viral LRTI and TSE had significantly lower richness (p = 0.03) and Shannon diversity (p = 0.02) (Fig. 3). Those with viral LRTI without TSE demonstrated a higher relative abundance of Moraxella spp. compared to those with TSE. In contrast to the entire cohort and non-smoke exposed patients with bacterial LRTI, non-smoke exposed patients with viral LRTI had a higher relative abundance of S. aureus, although the difference was small (Fig. 4).
Patients with clinically defined LRTI (no pathogen identified on bacterial or viral testing; n = 52) had no differences in total bacterial load, richness, or Shannon diversity based on TSE status (Fig. 3). However, patients with no TSE and clinically defined LRTI did demonstrate a higher relative abundance of Mycoplasma spp. At the species level, those without TSE had a higher relative abundance of S. mitis group and S. aureus. (Fig. 4).
There were no differences in total bacterial load, richness, or Shannon diversity between those with and without TSE among patients with a non-infectious reason for respiratory failure (n = 99) (Fig. 3). However, those with TSE had higher relative abundance of Moraxella spp. Serratia spp., S. aureus, and S. mitis group whereas those without TSE had higher relative abundance of Haemophilus spp. and Fusobacterium spp (Fig. 4).
Cotinine and clinical outcomes
TSE was not associated with diagnosis of ARDS within 48 h, duration of mechanical ventilation, ventilator free days to day 28, PICU length of stay (LOS), hospital LOS, or mortality (Table 3). There were no differences in clinical outcomes when comparing patients with and without TSE based on LRTI subgroup classification.
Discussion
This prospective, multicenter study evaluated the association between creatinine corrected urine cotinine levels, the lower airway microbiome, and clinical outcomes of critically ill children requiring prolonged mechanical ventilation. TSE was associated with lower richness, and lower Shannon diversity. In patients with TSE, the lower airway bacterial microbiome was represented by higher relative abundance of Moraxella spp., Haemophilus spp., and S. aureus. These changes were largely driven by differences observed among patients with bacterial and viral LRTI. TSE was not associated with clinical outcomes.
Overall, in critically ill children requiring prolonged mechanical ventilation, our findings demonstrate that TSE is associated with changes in the lower airway microbiome, yet the clinical implications of these differences were not readily discernable. Given the emerging role of the lung microbiome in modifying inflammatory signaling and acute lung injury,35 our findings highlight the need for ongoing investigations evaluating the mechanistic effects of TSE on the respiratory tract response to acute respiratory failure, especially in the setting of LRTI.
The TSE-related changes identified in richness and Shannon diversity within this cohort were largely driven by differences observed in patients with bacterial and viral LRTI. Changes in bacterial microbiome characteristics were not observed based on TSE status in the subgroups of patients with clinically diagnosed LRTI or non-infectious respiratory failure when sampled at the time of intubation. One potential explanation for this finding is that TSE may not be, in itself, responsible for changes in the lower airway microbiome, but may alter the host and immunologic response to infection leading to downstream changes in the microbiome in those with infectious LRTI. Alternatively, TSE may alter the baseline microbiome in such a way that makes children more susceptible to infection and pathogen expansion. TSE induced changes in interferon and interleukin expression, alveolar macrophage function, and T-cell response may contribute to changes in the microbiome in the setting of infection.12 The use of host transcriptomics and metagenomic next generation sequencing to evaluate both the microbiome, viral copy number, and host response in the setting of TSE may offer more insight.
Patients with a creatinine corrected urine cotinine level of ≥30 µg/g had a greater predominance of S. aureus, Haemophilus spp., and Moraxella spp. compared to non-TSE patients. S. aureus is a well described pulmonary pathogen in both community-acquired and hospital-acquired pneumonia.36,37 Haemophilus spp. have also been implicated in ventilator-associated pneumonia in children.37 While we did find statistically significant differences in the taxa, the clinical relevance is unclear given the small size of the difference and the sample size. Like the alterations seen with richness and Shannon diversity, these changes were largely found in patients with infectious LRTI. Patients with bacterial LRTI, viral LRTI, clinically diagnosed LRTI, and non-infectious respiratory failure all demonstrated variable patterns of relative abundance at the genera and species level based on TSE status.
These findings suggest that disease context may determine the influence of TSE on lower airway microbial communities, and that other factors may contribute to changes in the relative abundance of bacterial species. For example, Panzer et al. evaluated the microbiome at the time of intubation in adult trauma patients and compared active and passive smokers to non-smoke exposed patients. They observed increased relative abundance of Haemophilus spp., Streptococcus spp., and Fusobacterium spp. in patients who smoked or were smoke exposed.16 In our pediatric cohort, we similarly found an increase in Fusobacterium spp. and S. mitis group among TSE patients who were intubated for non-infectious causes. Future research focusing on larger, specific subgroups of patients with ARDS or bacterial LRTI may better delineate the potential impact of TSE on the lower airway microbiome.
Urine cotinine levels were not associated with the measured clinical outcomes in this cohort of severely critically ill children as participation required at least 72 h of mechanical ventilations support. These results are contrary to previously published pediatric and adult studies that evaluated the impact of TSE on clinical outcomes.4,10,11,16 In a study by Wilson et al., hospitalized pediatric patients with influenza and TSE were more likely to subsequently require intensive care, had longer hospital LOS, and were more likely to require intubation compared with non-TSE patients with influenza.8 Outcomes in this severely ill cohort are likely driven by patient and clinical course characteristics whereas patients of lower illness severity may have outcomes that are more affected by environmental exposures such as tobacco smoke. The effect of TSE on a population of hospitalized children that spans all severity levels will be essential to more accurately determine the impact of TSE on outcomes across a broader range of clinical presentations.
The most accurate way to determine TSE in children remains unclear. In our cohort, 38% of parents reported that their child had some degree of TSE. However, using a creatinine corrected urine cotinine cutoff of ≥30 µg/g, only 20% of our cohort met the criteria for TSE. This discrepancy may be related to the interval time difference between the patient’s last TSE and the urine collection for cotinine analysis. The average time to urine collection was 42.72 h after admission to the hospital and the half-life of urine cotinine is 16–24 h.26 It is, therefore, likely that the levels of cotinine were underestimating the exposure level in some smoke-exposed patients and may have contributed to misclassification. However, 24 children whose parents reported no history of TSE, did in fact, have creatinine corrected cotinine levels ≥30 µg/g. The discrepancy between parental reporting and urine cotinine measurements are in concordance with studies that have demonstrated that parental report is not sufficient in determining TSE.38,39
The results of this study are strengthened by the prospective, multi-center design. However, there are also several limitations of our study. First, patients in our study were intubated greater than 72 h, making the results less generalizable to less severely ill populations. Second, while we attempted to correct for time of collection (from time of hospital admission) in our continuous urine cotinine analysis, it may not have adequately corrected for the period from the last exposure, and we may have underestimated the number of patients who were smoke exposed. Thirdly, the TSE group was significantly younger and had significant differences in ethnicity. These findings are consistent with what has been found on the population level in the United States.3 It is difficult, however, to know whether or not these differences contributed to the findings of this study. Fourth, there were significant differences between the two groups among those who received antibiotics prior to hospitalization. However, nearly all of the patients enrolled in this study received antibiotics at the time of intubation and a single dose of antibiotics has been shown to alter the microbiome of other body compartments and may impact our ability to evaluate the lower airways microbiome via tracheal aspirates.40,41 Fifth, tracheal aspirates specimens may not adequately reflect lower lung bacteria. However, other methods such bronchiolar alveolar lavage are not frequently performed in children. Finally, this was an ancillary study that may have not been adequately powered to effectively evaluate differences between groups.
Conclusion
In conclusion, among critically ill children admitted to the PICU requiring prolonged mechanical ventilation, creatinine corrected urine cotinine levels were associated with increased total bacterial load, decreased richness and Shannon diversity of the lower airway microbiome, especially among patients with bacterial and viral LRTI. Specifically, patients with TSE had higher relative abundance of Haemophilus spp. Moraxella spp., and S. aureus. There were no identified associations between TSE and clinical outcomes. Additional prospective studies will be required to evaluate the implications of TSE on the severity and outcomes of critically ill children and whether the alteration of the airway microbiome could be a possible mechanism by which TSE conveys increased risk of poor outcomes. Future studies should focus on evaluating TSE earlier in the course of illness and obtaining airway microbiome specimens prior to antibiotic administration and in conjunction with measures of the host response to better understand the impact of TSE on this patient population.
Data availability
Deidentified data is publicly available at: https://hheardatacenter.mssm.edu/Search/Study. Microbiome data are available via: PRJNA533819 (data generated from methods development PRJNA436139 were also used for this study).
References
Oberg, M., Jaakkola, M. S., Woodward, A., Peruga, A. & Pruss-Ustun, A. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet 377, 139–146 (2011).
Liu, L. et al. Global, regional, and national causes of under-5 mortality in 2000-15: an updated systematic analysis with implications for the sustainable development goals. Lancet 388, 3027–3035 (2016).
Merianos, A. L., Jandarov, R. A., Choi, K. & Mahabee-Gittens, E. M. Tobacco smoke exposure disparities persist in U.S. children: Nhanes 1999–2014. Prev. Med. 123, 138–142 (2019).
Merianos, A. L., Jandarov, R. A. & Mahabee-Gittens, E. M. Secondhand smoke exposure and pediatric healthcare visits and hospitalizations. Am. J. Prev. Med. 53, 441–448 (2017).
Hur, K., Liang, J. & Lin, S. Y. The role of secondhand smoke in sinusitis: a systematic review. Int. Forum Allergy Rhinol. 4, 22–28 (2014).
Zhang, X., Johnson, N., Carrillo, G. & Xu, X. Decreasing trend in passive tobacco smoke exposure and association with asthma in U.S. children. Environ. Res. 166, 35–41 (2018).
Moore, B. F. et al. Interactions between diet and exposure to secondhand smoke on the prevalence of childhood obesity: results from Nhanes, 2007-2010. Environ. Health Perspect. 124, 1316–1322 (2016).
Wilson, K. M., Pier, J. C., Wesgate, S. C., Cohen, J. M. & Blumkin, A. K. Secondhand tobacco smoke exposure and severity of influenza in hospitalized children. J. Pediatr. 162, 16–21 (2013).
DiFranza, J. R., Masaquel, A., Barrett, A. M., Colosia, A. D. & Mahadevia, P. J. Systematic literature review assessing tobacco smoke exposure as a risk factor for serious respiratory syncytial virus disease among infants and young children. BMC Pediatr. 12, 81 (2012).
Calfee, C. S. et al. Cigarette smoke exposure and the acute respiratory distress syndrome. Crit. Care Med. 43, 1790–1797 (2015).
Hsieh, S. J. et al. Prevalence and impact of active and passive cigarette smoking in acute respiratory distress syndrome. Crit. Care Med. 42, 2058–2068 (2014).
Strzelak, A., Ratajczak, A., Adamiec, A. & Feleszko, W. Tobacco smoke induces and alters immune responses in the lung triggering inflammation, allergy, asthma and other lung diseases: a mechanistic review. Int. J. Environ. Res. Public Health 15, 1033 (2018).
Jette, M. E., Dill-McFarland, K. A., Hanshew, A. S., Suen, G. & Thibeault, S. L. The human laryngeal microbiome: effects of cigarette smoke and reflux. Sci. Rep. 6, 35882 (2016).
Stewart, C. J. et al. Effects of tobacco smoke and electronic cigarette vapor exposure on the oral and gut microbiota in humans: a pilot study. PeerJ 6, e4693 (2018).
Charlson, E. S. et al. Disordered microbial communities in the upper respiratory tract of cigarette smokers. PLoS One 5, e15216 (2010).
Panzer, A. R. et al. Lung microbiota is related to smoking status and to development of acute respiratory distress syndrome in critically Ill trauma patients. Am. J. Respir. Crit. Care Med. 197, 621–631 (2018).
Mourani, P. M. et al. Temporal airway microbiome changes related to ventilator-associated pneumonia in children. Eur. Respir. J. 57, 2001829 (2021).
Zemanick, E. T. et al. Airway microbiota across age and disease spectrum in cystic fibrosis. Eur. Respir. J. 50, 1700832 (2017).
Hara, N. et al. Prevention of virus-induced type 1 diabetes with antibiotic therapy. J. Immunol. 189, 3805–3814 (2012).
Markle, J. G. et al. Sex differences in the gut microbiome drive hormone-dependent regulation of autoimmunity. Science 339, 1084–1088 (2013).
Balshaw, D. M., Collman, G. W., Gray, K. A. & Thompson, C. L. The children’s health exposure analysis resource: enabling research into the environmental influences on children’s health outcomes. Curr. Opin. Pediatr. 29, 385–389 (2017).
Murphy, S. E. et al. Nicotine N-Glucuronidation relative to N-Oxidation and C-Oxidation and Ugt2b10 genotype in five ethnic/racial groups. Carcinogenesis 35, 2526–2533 (2014).
Benowitz, N. L. et al. Urine nicotine metabolite concentrations in relation to plasma cotinine during low-level nicotine exposure. Nicotine Tob. Res. 11, 954–960 (2009).
Benowitz, N. L. et al. Urine 4-(Methylnitrosamino)-1-(3) Pyridyl-1-Butanol and cotinine in alaska native postpartum women and neonates comparing smokers and smokeless tobacco users. Int J. Circumpolar Health 77, 1528125 (2018).
Benowitz, N. L. et al. Urine cotinine screening detects nearly ubiquitous tobacco smoke exposure in urban adolescents. Nicotine Tob. Res. 19, 1048–1054 (2017).
Torres, S., Merino, C., Paton, B., Correig, X. & Ramirez, N. Biomarkers of exposure to secondhand and thirdhand tobacco smoke: recent advances and future perspectives. Int. J. Environ. Res. Public Health 15, 2693 (2018).
Fried, P. A., Perkins, S. L., Watkinson, B. & McCartney, J. S. Association between creatinine-adjusted and unadjusted urine cotinine values in children and the mother’s report of exposure to environmental tobacco smoke. Clin. Biochem. 28, 415–420 (1995).
Henderson, F. W. et al. Home air nicotine levels and urinary cotinine excretion in preschool children. Am. Rev. Respir. Dis. 140, 197–201 (1989).
Zhang, C. et al. Unintentional tobacco smoke exposure in children. Int. J. Environ. Res. Public Health 19, 7076 (2022).
Langelier, C. et al. Integrating host response and unbiased microbe detection for lower respiratory tract infection diagnosis in critically Ill adults. Proc. Natl Acad. Sci. USA 115, E12353–E12362 (2018).
Force, A. D. T. et al. Acute respiratory distress syndrome: the berlin definition. JAMA 307, 2526–2533 (2012).
Pollack, M. M., Patel, K. M. & Ruttimann, U. E. Prism Iii: an updated pediatric risk of mortality score. Crit. Care Med. 24, 743–752 (1996).
Williamson, K. M. et al. Modified Pcr protocol to increase sensitivity for determination of bacterial community composition. Microbiome 9, 90 (2021).
Keskinoglu, P., Cimrin, D. & Aksakoglu, G. Which cut-off level of urine cotinine:creatinine ratio (Ccr) should be used to determine passive smoking prevalence in children in community based studies? Tob. Control 16, 358–359 (2007).
Dickson, R. P. The lung microbiome and ards. it is time to broaden the model. Am. J. Respir. Crit. Care Med. 197, 549–551 (2018).
Fritz, C. Q. et al. Prevalence, risk factors, and outcomes of bacteremic pneumonia in children. Pediatrics 144, e20183090 (2019).
Srinivasan, R., Asselin, J., Gildengorin, G., Wiener-Kronish, J. & Flori, H. R. A prospective study of ventilator-associated pneumonia in children. Pediatrics 123, 1108–1115 (2009).
Avila-Tang, E. et al. Assessing secondhand smoke exposure with reported measures. Tob. Control 22, 156–163 (2013).
McCarville, M., Sohn, M. W., Oh, E., Weiss, K. & Gupta, R. Environmental tobacco smoke and asthma exacerbations and severity: the difference between measured and reported exposure. Arch. Dis. Child 98, 510–514 (2013).
Larsson Wexell, C. et al. Antimicrobial effect of a single dose of amoxicillin on the oral microbiota. Clin. Implant Dent. Relat. Res. 18, 699–706 (2016).
Buffie, C. G. et al. Profound alterations of intestinal microbiota following a single dose of clindamycin results in sustained susceptibility to clostridium difficile-induced colitis. Infect. Immun. 80, 62–73 (2012).
Acknowledgements
This study was supported by NICHD Collaborative Pediatric Critical Care Research Network.
Funding
Supported in part, by the following cooperative agreements from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), and Heart Lung Blood Institute (NHLBI), National Institutes of Health (NIH): UG1HD083171 (P.M.M.), 1R01HL124103 (P.M.M. and M.K.S.), UG1HD049983 (J.C.), UG01HD049934 (R. Reeder, C. Locandro), UG1HD050096 (K.L.M.), UG1HD083166 (P.S.M.), UG1HD049981 (M.M.P.), and K23HL138461-01A1 (C.L.). NIH/NIEHS funded Human Heath Exposure Analysis Resource (HHEAR) under grant numbers U2CES026555, U2CES026560, and U2CES026553.
Author information
Authors and Affiliations
Contributions
M.K.L., K.M.W., P.C.C., B.D.W., L.A., M.B., S.A.B., S.E.M., L.A.P., K.R.V., C.J.S., E.A.T., J.K.H., A.B.M., C.M.O. and P.M.M. contributed to the design of the study, data analysis and interpretation of the data. K.M.W., M.K.S., B.D.W., J.K.H., R.W.R., C.L., T.C.C., E.A.F.S., C.E.R., C.L., J.A.C., K.L.M., M.M.P., P.S.M., and P.M.M. contributed to data and sample acquisition and conduct of primary study. M.K.L. was responsible for primary authorship of the manuscript. All authors contributed to revision of the content and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
M.K.L. has nothing to disclose. K.M.W. has nothing to disclose. P.C.C. reports grants from NIH during the conduct of the study. M.K.S. reports grants from NIH NHLDI during the conduct of the study. L.A. reports grant funding from Pfizier Inc. outside the submitted work. M.B. has nothing to disclose. S.A.B. has nothing to disclose. S.E.M. has nothing to disclose. L.A.P. has nothing to disclose. J.K.H. has nothing to disclose. R.W.R. has nothing to disclose. C.L. has nothing to disclose. T.C.C. reports grants from NIH NHLBI during the conduct of the study. A.B.M. reports a grant from Parker B. Francis Foundation and NIH NICHD, outside the submitted work. E.A.F.S. reports grants from Astra Zeneca Inc, Merck & Co, Regeneron Inc, Pfizer Inc, Roche Inc, Johnson and Johnson, and Novavax Inc; consulting fees from Merck & Co, Pfizer Inc, Alere Inc, Cidara Therapeutics, and Sanofi Pasteur; support from travel from Merck & Co and Pfizer Inc; participation on Data Safety and Monitoring Boards with Abbvie, Glasco Smith Klein and the Bill and Melinda Gates Foundation all outside of the submitted work. C.M.O. has nothing to disclose. C.E.R. has nothing to disclose. C.L. has nothing to disclose. J.A.C. has nothing to disclose. K.L.M. has nothing to disclose. M.M.P. reports grants from the NIH during the conduct of the study. P.S.M. has nothing to disclose. P.M.M. reports grants from NIH NIHLBI and NIH NICHD during the conduct of the study.
Consent to publish/participate
The study was approved by the University of Utah central Institutional Review Board and consent was obtained from all patients.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Leroue, M.K., Williamson, K.M., Curtin, P.C. et al. Tobacco smoke exposure, the lower airways microbiome and outcomes of ventilated children. Pediatr Res 94, 660–667 (2023). https://doi.org/10.1038/s41390-023-02502-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02502-8
This article is cited by
-
Oxidative stress and inflammation: elucidating mechanisms of smoking-attributable pathology for therapeutic targeting
Bulletin of the National Research Centre (2024)