Abstract
Background
A common first-line treatment for supporting cardiovascular function in preterm infants is volume expansion using saline, but this does not improve outcomes. This study aimed to determine if volume expansion with saline increases blood volume, blood pressure and cerebral oxygenation; and if volume expansion with packed red blood cells (RBC) is more effective. We hypothesized that RBC infusion is more effective than saline for increasing blood volume and maintaining cardiovascular function and cerebral oxygenation.
Methods
Five groups of preterm piglets (98/115d gestation) were infused with saline (10 or 20 mL/kg) or RBC (10 or 20 mL/kg) or no treatment. Blood volume, blood pressure, central venous pressure, heart rate, carotid flow, cerebral oxygenation, arterial pH, base excess, and lactate levels were assessed for 6 h after treatment started.
Results
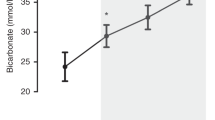
Both RBC groups had significant increases in blood volume, and improved measures of cardiovascular function, cerebral oxygenation and metabolic acidosis. Saline infusion did not increase blood volume or measures of cardiovascular function, cerebral oxygenation or metabolic acidosis.
Conclusions
The results suggest that the deteriorating cardiovascular function in the hours after birth in preterm piglets, and possibly in premature babies, may be reversed or halted by more effective support of blood volume.
Impact
-
Blood volume decreases after birth in preterm piglets and this decrease is associated with deteriorating cardiovascular function and cerebral oxygenation.
-
Infusion of saline does not increase blood volume nor prevent deterioration in cardiovascular function.
-
Infusion of packed red blood cells results in an increase in blood volume and improvements in cardiovascular function and cerebral oxygenation.
-
Deteriorating cardiovascular function in the hours after birth in preterm piglets, and possibly in human preterm neonates, may be reversed or halted by more effective support of blood volume.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Hee Chung, E., Chou, J. & Brown, K. A. Neurodevelopmental outcomes of preterm infants: a recent literature review. Transl. Pediatr. 9, S3–S8 (2020).
Eiby, Y. A. et al. Endogenous angiotensins and catecholamines do not reduce skin blood flow or prevent hypotension in preterm piglets. Physiol. Rep. 2, e12245 (2014).
Batton, B. et al. Early blood pressure, antihypotensive therapy and outcomes at 18-22 months’ corrected age in extremely preterm infants. Arch. Dis. Child Fetal Neonatal Ed. 101, F201–F206 (2016).
Osborn, D. A. & Evans, N. J. Early volume expansion for prevention of morbidity and mortality in very preterm infants. Cochrane Database Syst. Rev. 2004, CD002055 (2004).
Osborn, D. A., Paradisis, M. & Evans, N. The effect of inotropes on morbidity and mortality in preterm infants with low systemic or organ blood flow. Cochrane Database Syst. Rev. 2007, CD005090 (2007).
Eiby, Y. A. et al. Inotropes do not increase cardiac output or cerebral blood flow in preterm piglets. Pediatr. Res. 80, 870–879 (2016).
Osborn, D. A. & Evans, N. Early volume expansion for prevention of morbidity and mortality in very preterm infants. Cochrane Database Syst. Rev. CD002055 (2001).
Eiby, Y. A., Lumbers, E. R., Headrick, J. P. & Lingwood, B. E. Left ventricular output and aortic blood flow in response to changes in preload and afterload in the preterm piglet heart. Am. J. Physiol. Regul. Integr. Comp. Physiol. 303, R769–R777 (2012).
Eiby, Y. A. et al. Reduced blood volume decreases cerebral blood flow in preterm piglets. J. Physiol. 596, 6033–6041 (2018).
Eiby, Y. A., Lingwood, B. E. & Wright, I. M. R. Plasma leak from the circulation contributes to poor outcomes for preterm infants: a working hypothesis. Front Neurol. 12, 636740 (2021).
Eiby, Y. A. et al. A pig model of the preterm neonate: anthropometric and physiological characteristics. PLoS One 8, e68763 (2013).
National Blood Authority, Australia. Patient Blood Management Guidelines Module 6 62 (2016)..
Eiby, Y. A., Bakrania, B. A., Morwood, H. K., Wright, I. M. R. & Lingwood, B. E. A new method for measuring blood volume in preterm piglets using fluorescently labelled dextrans: clinical applicability in preterm infants. Pediatr. Res. (submitted 2022).
Cincović, M., Mirkov, M., Radović, I., Belić, B. & Lakić, I. Reference values of hematological, biochemical and endocrinological parameters in the blood of piglets aged 1 and 21 days. Contemp. Agric. 69, 34–40 (2020).
Brace, R. A. Fetal blood volume responses to intravenous saline solution and dextran. Am. J. Obstet. Gynecol. 147, 777–781 (1983).
Brace, R. A. & Gold, P. S. Fetal whole-body interstitial compliance, vascular compliance, and capillary filtration coefficient. Am. J. Physiol. Regul. Integr. Comp. Physiol. 247, R800–R805 (1984).
Harake, B. & Power, G. Thoracic duct lymph flow: a comparative study in newborn and adult sheep. J. Dev. Physiol. 8, 87–95 (1986).
Blumberg, N. et al. 0.9% NaCl (normal saline) – perhaps not so normal after all? Transfus. Apher. Sci. 57, 127–131 (2018).
Bakshi, S., Koerner, T., Knee, A., Singh, R. & Vaidya, R. Effect of fluid bolus on clinical outcomes in very low birth weight infants. J. Pediatr. Pharmacol. Ther. 25, 437–444 (2020).
Synnes, A. R., Chien, L. Y., Peliowski, A., Baboolal, R. & Lee, S. K. Variations in intraventricular hemorrhage incidence rates among Canadian Neonatal Intensive Care Units. J. Pediatr. 138, 525–531 (2001).
Keir, A. K. et al. International, multicentre, observational study of fluid bolus therapy in neonates. J. Paediatr. Child Health 55, 632–639 (2019).
Aladangady, N., McHugh, S., Aitchison, T. C., Wardrop, C. A. & Holland, B. M. Infants’ blood volume in a controlled trial of placental transfusion at preterm delivery. Pediatrics 117, 93–98 (2006).
Aladangady, N. et al. Is it possible to predict the blood volume of a sick preterm infant? Arch. Dis. Child Fetal Neonatal Ed. 89, F344–F347 (2004).
Stark, M. J., Clifton, V. L. & Wright, I. M. Microvascular flow, clinical illness severity and cardiovascular function in the preterm infant. Arch. Dis. Child Fetal Neonatal Ed. 93, F271–F274 (2008).
Wallenstein, M. B. et al. Red blood cell transfusion is not associated with necrotizing enterocolitis: a review of consecutive transfusions in a tertiary neonatal intensive care unit. J. Pediatr. 165, 678–682 (2014).
Davies, M. W. Partial Liquid Ventilation and Cerebral Blood Flow: The Effects of the Administration of a Dose of Perfluorocarbon Liquid, When Starting Partial Liquid Ventilation, on Cerebral Blood Flow. PhD thesis, The University of Queensland (2010).
Acknowledgements
The authors would like to express their appreciation to Dr Elliot Teo for his assistance with preparation of the manuscript.
Funding
This study was funded by the National Health and Medical Research Council of Australia (APP1127142).
Author information
Authors and Affiliations
Contributions
Y.E., I.W., M.S. and B.L. conceptualized and designed the study. Y.E., I.W. and B.L. collected, analyzed and interpreted the data. Y.E. drafted the initial manuscript. All authors reviewed and approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Eiby, Y.A., Wright, I.M.R., Stark, M.J. et al. Red cell infusion but not saline is effective for volume expansion in preterm piglets. Pediatr Res 94, 112–118 (2023). https://doi.org/10.1038/s41390-022-02403-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02403-2