Abstract
Objective
Decrease the incidence of inadequate diuresis (ID, loss of <6% of birth weight) in extremely preterm neonates (EPT, <28 weeks of gestation at birth) during the first week of life by 50% in 1 year.
Study design
Quality improvement project in a level IV neonatal intensive care unit. A fluid management protocol was implemented, including the use of a fluid guide sheet and closer monitoring of hydration parameters. Seventy-nine baseline EPT neonates were compared to 83 post intervention. The incidence of ID was tracked monthly, along with prespecified morbidities and complications. Statistical data analyses also compared the pre- and post-intervention periods.
Results
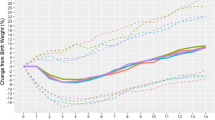
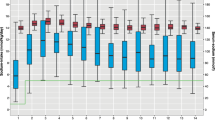
Fluid volumes in the first week were decreased (p < 0.001). ID decreased from 43 to 29% (p = 0.061). Tracked morbidities and complications were not statistically different.
Conclusion
Intentional and individualized adjustment of fluids led to decreased ID without increased hypernatremia and dehydration, or a change in tracked morbidities.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Bhatia J. Fluid and electrolyte management in the very low birth weight neonate. J Perinatol. 2006;26:19–21.
Verma RP, Shibli S, Fang H, Komaroff E. Clinical determinants and utility of early postnatal maximum weight loss in fluid management of extremely low birth weight infants. Early Hum Dev. 2009;85:59–64.
O’Brien F, Walker IA. Fluid homeostasis in the neonate. Paediatr Anaesth. 2014;24:49–59.
Oh W, Poindexter BB, Perritt R, Lemons JA, Bauer CR, Ehrenkranz RA, et al. Association between fluid intake and weight loss during the first ten days of life and risk of bronchopulmonary dysplasia in extremely low birth weight Infants. J Pediatr. 2005;147:786–90.
Bell EF, Warburton D, Stonestreet BS, Oh W. Effect of fluid administration on the development of symptomatic patent ductus arteriosus and congestive heart failure in premature infants. N Engl J Med. 1980;302:598–604.
Stephens BE, Gargus RA, Walden RV, Mance M, Nye J, McKinley L, et al. Fluid regimens in the first week of life may increase risk of patent ductus arteriosus in extremely low birth weight infants. J Perinatol. 2008;28:123–8.
Martin R, Fanaroff A, Walsh M. Fluids, electrolytes, and acid-base homeostasis. In: Fanaroff and Martin’s neonatal-perinatal medicine. 9th ed. St. Louis: Elsevier Mosby; c2010, pp. 669–83.
Lorenz JM, Kleinman LI, Kotagal UR, Reller MD. Water balance in very low-birth-weight infants: relationship to water and sodium intake and effect on outcome. J Pediatr. 1982;101:423–32.
Oh W. Fluid and electrolyte management of very low birth weight infants. Pediatr Neonatol. 2012;53:329–33.
Hartnoll G, Bétrémieux P, Modi N. Randomised controlled trial of postnatal sodium supplementation on body composition in 25 to 30 week gestational age infants. Arch Dis Child Fetal Neonatal Ed. 2000;82:24–8.
Verma RP, Shibli S, Komaroff E. Postnatal transitional weight loss and adverse outcomes in extremely premature neonates. Pediatr Rep. 2017;9:6962.
Wadhawan R, Oh W, Perritt R, Laptook AR, Poole K, Wright LL, et al. Association between early postnatal weight loss and death or BPD in small and appropriate for gestational age extremely low-birth-weight infants. J Perinatol. 2007;27:359–64.
Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for Quality Improvement Reporting Excellence) revised publication guidelines from a detailed consensus process. AMJ Crit Care. 2015;24:466–73.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Jobe A, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Aksoy HT, Güzoğlu N, Eras Z, Gökçe İK, Canpolat FE, Uraş N, et al. The association of early postnatal weight loss with outcome in extremely low birth weight infants. Pediatr Neonatol. 2019;60:192–6.
Guo MM, Chung CH, Chen FS, Chen CC, Huang HC, Chung MY. Severe bronchopulmonary dysplasia is associated with higher fluid intake in very low-birth-weight infants: a retrospective study. Am J Perinatol. 2015;30:155–62.
Bell EF, Acarregui MJ. Restricted versus liberal water intake for preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev. 2014;12:1465–858.
Van Marter LJ, Leviton A, Allred EN, Pagano M, Kuban KC. Hydration during the first days of life and the risk of bronchopulmonary dysplasia in low birth weight infants. J Pediatr. 1990;116:942–9.
Costarino AT, Gruskay JA, Corcoran L, Polin RA, Baumgart S. Sodium restriction versus daily maintenance replacement in very low birth weight premature neonates: a randomized, blind therapeutic trial. J Pediatr. 1992;120:99–106.
Lim W-H, Lien R, Chiang M-C, Fu R-H, Lin J-J, Chu S-M. Hypernatremia and grade III/IV intraventricular hemorrhage among extremely low birth weight infants. J Perinatol. 2011;31:193–8.
Spahr R, Klein A, Brown D, Holzman I, MacDonald H. Fluid administration and bronchopulmonary dysplasia: The lack of an association. Am J Dis Child. 1980;134:958–60.
Kavvadia V, Greenough A, Dimitriou G, Hooper R. Comparison of the effect of two fluid input regimens on perinatal lung function in ventilated infants of very low birth weight. Eur J Pediatr. 1999;158:917–22.
Author information
Authors and Affiliations
Contributions
JH: conceptualization and implementation of project, authorship of the discussion section, compiled the first draft of the paper, and critically reviewed the final paper, AW: conceptualization and implementation of project, authorship of the introduction, and revision of paper, NH: conceptualization and implementation of project, authorship of the discussion section, and revision of paper, SM: conceptualization and implementation of project, authorship of the methods section, and review of paper, ED: conceptualization and implementation of project, authorship of the introduction, and review of paper. DT: statistical analysis, authorship of the results section, and revision of paper. UA: conceptualization and implementation of project, authorship of the methods section, compiled the second draft of the paper, and revision of paper. JH and AW contributed equally to the conception and implementation of the project as well as authorship and are co-first authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The Institutional Review Board at our institution deemed this project exempt from review as it was considered a QI project.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Havinga, J., Williams, A., Hassan, N. et al. Individualized fluid management in extremely preterm neonates to ensure adequate diuresis without increasing complications. J Perinatol 41, 240–246 (2021). https://doi.org/10.1038/s41372-020-00789-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-00789-7