Abstract
Background
Low birth weight (LBW) followed by a rapid postnatal catch-up in weight predisposes individuals to a central distribution of body fat, which is reverted by metformin. Growth-and-differentiation-factor-15 (GDF15) plays an important role in the regulation of energy homeostasis, reducing food intake and body weight. We assessed whether GDF15 concentrations are raised by long-term metformin treatment in LBW/catch-up girls with precocious pubarche (PP, pubic hair <8 years), and whether they relate to changes in endocrine-metabolic variables, body composition, and abdominal fat partitioning.
Methods
Circulating GDF15 was determined in 30 LBW/catch-up girls with PP randomly assigned to receive metformin for 4 years (n = 15; 425 mg/d for 2 years, then 850 mg/d for 2 years) or to remain untreated (n = 15). Endocrine-metabolic variables, body composition (by absorptiometry), and abdominal fat partitioning (by MRI) were assessed at the start and yearly during follow-up.
Results
Circulating GDF15 concentrations increased significantly in LBW-PP girls only after 3 and 4 years on metformin. GDF15 levels associated negatively with insulin, HOMA-IR, androgens, body fat, and visceral fat.
Conclusion
Prepubertal intervention with metformin reduces central adiposity and insulin resistance in girls with reduced prenatal growth. GDF15 could be among the mediators of such effects, especially over the long term.
Impact
-
Low birth weight followed by a rapid postnatal catch-up in weight predisposes individuals to a central distribution of body fat, which is reverted by metformin.
-
Growth-and-differentiation-factor-15 (GDF15) is a peptide hormone that reduces food intake and lowers body weight; metformin is an exogenous GDF15 secretagogue.
-
Serum GDF15 concentrations increase after 3 and 4 years on metformin and associate negatively with insulin, androgens, body fat, and visceral fat.
-
Prepubertal intervention with metformin reduces central adiposity and insulin resistance in girls with low birth weight. GDF15 could mediate these effects, especially over the long term.
Similar content being viewed by others
Introduction
Low birth weight (LBW) followed by a rapid postnatal catch-up in weight—the so-called “mismatch” or imbalance between the early capacity to store lipids and the later need for lipid storage1—predisposes individuals to overweight/obesity with a predominantly central (hepato-visceral) distribution of body fat, that may initiate the cascade of events leading to metabolic disturbances.2
In prepubertal girls, the ectopic accumulation of lipids induces hyperinsulinism, and a decrease in circulating sex hormone-binding globulin and high-molecular-weight (HMW) adiponectin levels, and may lead to an early and amplified adrenarche, with or without precocious pubarche (PP, pubic hair before age 8 years).3,4 This sequence may be followed by an early and rapidly progressive puberty with early menarche (<12 years), adult height below the target level, ovarian androgen excess, and features of polycystic ovary syndrome (PCOS).1,5 Early metformin treatment (at age 8–12 years) slows down the rapid maturation of LBW-PP girls, delays menarche by approximately 1 year, increases adult height and reduces insulin resistance and central fat and thus prevents the progression to PCOS.6,7
Growth-and-differentiation-factor-15 (GDF15) is a peptide hormone that belongs to the transforming factor β superfamily of proteins. GDF15 is expressed in multiple tissues and is strongly increased in the circulation during pregnancy, after tissue injury, and in diverse disease states, including cancer, cardiovascular, and kidney disease, where it often correlates with a poorer prognosis.8 GDF15 also plays an important role in the regulation of energy homeostasis, reducing food intake and lowering body weight through the activation of the specific brainstem receptor glial-derived neurotrophic factor receptor alpha-like (GFRAL).8 Metformin is an exogenous GDF15 secretagogue, and recent evidence suggests that GDF15 may mediate the effects of metformin on energy balance.9,10,11
Here, we assessed whether circulating GDF15 concentrations are raised by long-term metformin treatment in so-called “mismatch” prepubertal girls with the sequence of reduced prenatal weight gain followed by excessive postnatal weight gain and PP, and whether GDF15 concentrations relate to changes in endocrine-metabolic and body composition parameters and in abdominal fat distribution across the intervention.
Research design and methods
Subjects, study design and ethics
The study population consisted of 32 girls with PP and a history of LBW/catch-up in weight who were enrolled in a longitudinal, long-term prospective study assessing the effects of early and prolonged metformin treatment (over 4 years) on puberty, menarche, body composition, abdominal fat partitioning and PCOS markers (starting in prepuberty, at age 8 years) (Supplementary Fig. S1, flow chart).6,7,12,13,14
The main outcomes of metformin treatment on these girls have been previously published.6,7,12,13,14 As formerly described, the specific inclusion criteria were: (1) PP due to exaggerated adrenarche, as judged by high serum dehydroepiandrosterone-sulfate (DHEA-S) and/or androstenedione levels;15 (2) weight <2.9 kg at term birth (38–41 weeks) or below –1 SD for gestational age at preterm birth (33–37 weeks) that is the level of prenatal growth restraint in our population that is subsequently associated with the development of PP and followed by PCOS in adolescence;16 (3) BMI < 22 kg/m2, which corresponds to the +2 SD cut-off in girls aged 8 years; and (4) prepuberty (Tanner breast stage I).17 Exclusion criteria were 21-hydroxylase deficiency, glucose intolerance, diabetes, evidence for thyroid, liver or kidney dysfunction, and prior use of medications known to affect the gonadal function or carbohydrate metabolism. Girls were randomly assigned to remain untreated or to receive metformin for 4 years at dinner time (425 mg/d for 2 years, then 850 mg/d for 2 years). The increase in metformin dose after 2 years was based on previous pharmacokinetic studies performed in girls with LBW-PP showing that a metformin dose between 20 and 30 mg/Kg/d is safe and effective.18 The original study included n = 19 girls in each study arm; the present report includes only those girls with complete longitudinal data in whom the remaining serum sample was sufficiently abundant to measure GDF15 (n = 32; n = 16 out of 19 in each study arm; ∼84% of the initial study population; Supplementary Fig. S1). Basal outlier values for GDF15 concentrations were sought according to the interquartile range (IQR) method.19 Values that fell below Q1 – 1.5 IQR or above Q3 + 1.5 IQR were excluded from analyses (n = 2; one 1 in each study arm). Thus, a total of n = 30 patients were included in the final analysis (n = 15 in each study arm).
Serum GDF15 was also measured cross-sectionally in 15 age-matched healthy control girls [age, 8.0 ± 0.2 years; BMI Z-score, –0.4 ± 0.3 (mean ± SEM)]. These girls were selected according to sample availability among those recruited at birth into an observational study assessing FSH and inhibin levels in early infancy and subsequently followed up at the Barcelona hospital until age 8 years. All were born appropriate-for-gestational age (AGA, between –1 SD and +1 SD) after a term pregnancy and were apparently healthy.20
The study was registered as ISRCTN84749320 and was approved by the Institutional Review Board of Barcelona University, Hospital of Sant Joan de Déu. Informed consent was obtained from the parents and assent from the girls.
Assessments
Gestational age, birth weight, and birth length were retrieved from medical records, and Z-scores were derived according to country and sex-specific references.21 Height and weight were measured and BMI was calculated and transformed into Z-score, as described.6,7,21 Tanner stage was assessed by the same investigator (L.I.) throughout the study.
Blood samples were obtained in the morning after an overnight fast. Serum glucose was measured by the glucose oxidase method. Insulin, IGF-I, DHEA-S, testosterone, and androstenedione were assayed by immunochemiluminiscence (DPC IMMULITE 2500, Siemens, Erlangen, Germany); intra- and inter-assay coefficients of variation (CVs) were <10%; HDL-cholesterol, LDL-cholesterol, and triglycerides were assessed by an enzymatic method (Architect c8000 autoanalyzer, Abbott laboratories, North Chicago, IL). Homeostasis model assessment for insulin resistance (HOMA-IR) was calculated as fasting insulin (mU/L) × fasting glucose (mmol/L)/22.5. Circulating HMW-adiponectin was measured with a specific human ELISA (R&D Systems, Minneapolis, MN); the intra- and inter-assay CVs were <9%. GDF15 was assessed by ELISA (R&D Systems, Minneapolis, MN); the intra- and inter-assay CVs were <6%.
Body composition was assessed by dual-energy X-ray absorptiometry with a Lunar prodigy coupled to Lunar software (Lunar Corp., Madison, WI). Abdominal fat partitioning (subcutaneous and visceral fat areas) was assessed by magnetic resonance imaging (Signa LX Echo Speed Plus Excite; General Electric, Milwaukee, WI). Patients were scanned using a T1-weighed spin-echo sequence with 360 msec repetition time, 21 msec echo time, 40 cm field of view, and 256 × 224 matrix. To obtain abdominal fat values, transverse slices of 10-mm thickness were acquired beginning at the L4–L5 intervertebral space. Subcutaneous and visceral fat areas were measured by fitting a spline curve to points on the border of the subcutaneous and visceral regions selected by the same operator, blinded to treatment allocation. Nonfat regions within the visceral region were also outlined with a spline fit and subtracted from the total visceral region. The visceral fat region was subdivided into retroperitoneal and intraperitoneal areas, as described, and the visceral fat area was calculated by subtracting the organ areas from the intraperitoneal area.22 Liver fat was quantified by comparing the relative intensity of the liver to that of subcutaneous fat and spleen, assuming that the latter is fat-free; the formula used (expressing hepatic fat in %) was 100 × (AI liver – AI spleen)/(AI adipose – AI spleen), where AI is average intensity.23
Statistics
Statistical analyses were performed using SPSS software 22.0 (SPSS Inc. Chicago, IL) and GraphPad Prism 6.01. Results are expressed as mean ± SEM. All variables were checked for normality using the Kolmogorov–Smirnov test prior to analyses. Comparisons within and between groups at each time point were performed using unpaired t-test or Mann–Whitney U test for non-parametric variables. Two-way ANOVA with post-hoc Bonferroni correction was performed to assess simultaneously the influence of treatment and time on GDF15 concentrations. Correlation analysis was used to study the associations between GDF15 concentrations and auxological, endocrine-metabolic, and body composition parameters. The level of significance was set at p < 0.05.
Results
Supplementary Table S1 summarizes selected longitudinal variables of the study population. No differences between LBW-PP subgroups were observed at the start. Three girls in the untreated subgroup were premature, and three were small-for-gestational age (SGA).24 Within the treated subgroup, three girls were premature and four were SGA. After 4 years, metformin-treated girls had comparable BMI Z-scores vs untreated girls, tended to be less insulin resistant, had a healthier lipid profile, and normalized testosterone levels. In metformin-treated girls, the net gain of body fat was about 50% lower than in untreated girls due to a decrease in visceral fat. Moreover, circulating HMW-adiponectin concentrations throughout follow-up showed a significant decrease only in untreated girls.
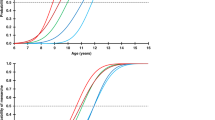
Figure 1 depicts the longitudinal changes in GDF15 concentrations. No differences were observed in GDF15 circulating levels at baseline between LBW-PP and control girls. Metformin treatment was accompanied by a marked increase in circulating GDF15 concentrations after 3 and 4 years (47 and 43%, respectively, vs untreated girls). In year 3, which was the first year wherein metformin was dosed at 850 mg/d, GDF15 concentrations increased from 313 ± 22 pg/mL in untreated girls to 462 ± 50 pg/mL in metformin-treated girls (p < 0.01 for between-group difference). Two-way ANOVA disclosed that treatment had a significant effect on GDF15 levels (p = 0.0001).
The study girls were randomized to remain untreated (n = 15, white dots), or to receive metformin for 4 years (n = 15, gray dots; 425 mg/d the first 2 years, then 850 mg/d for the subsequent 2 years).Data are mean ± SEM, #p = 0.0001 by two-way ANOVA.The dashed line and the upper and lower limits of the gray zone correspond, respectively, to the mean value and to a Z-score of +1 and −1, in healthy prepubertal girls (n = 15; age, 8.0 ± 0.2 years; body mass index Z-score, –0.4 ± 0.3; GDF15, 378 ± 28 pg/mL).
Table 1 shows the correlations between serum GDF15 concentrations and endocrine-metabolic and body composition parameters. GDF15 concentrations correlated negatively with insulin and HOMA-IR at 2 years and at 3 years, with testosterone at 1 year, 2 years, and at 4 years, with total and abdominal fat at 3 and at 4 years, and with visceral fat and visceral-to-subcutaneous fat ratio after 4 years.
Discussion
Here, we report for the first time the effects of prolonged metformin intervention on circulating GDF15 concentrations in a cohort of “mismatch” prepubertal girls with PP and with the sequence of reduced prenatal weight gain followed by marked postnatal catch-up in weight, and disclose that circulating GDF15 concentrations display a significant increase at distinct time points of metformin treatment. Moreover, GDF15 concentrations were found to associate negatively with markers of insulin resistance, androgen levels, and with total and visceral fat.
Pre-treatment concentrations of GDF15 were comparable in “mismatch” LBW-PP girls and in age-matched healthy control girls; however, in the former, insulin levels were more than two-fold higher. As insulin is an endogenous GDF15 secretagogue,25 it can be hypothesized that “mismatch” LBW-PP girls have a relative GDF15 deficit which, in turn, could be among the mechanisms accounting for the higher risks for overweight/obesity in this population. A comparable scenario was recently reported in adolescents with PCOS, an entity frequently preceded by a similar “mismatch” sequence.10
Circulating GDF15 concentrations remained unchanged during the first 2 years of intervention when the girls were receiving a metformin dose of 425 mg/d; however, GDF15 concentrations raised significantly from the third year of treatment onwards concomitant with the doubling in metformin dose, suggesting that metformin effects in children may be dose- and probably even more time-dependent. Along these lines, in patients with dysglycemia, GDF15 concentrations have been shown to be a reflection of the dose of metformin received and serve as a biomarker for the use of metformin in this population.26 Also, studies in mice suggest that GDF15 induction in response to metformin is less evident in the absence of obesity.27
It is well recognized that puberty is a state of insulin resistance,28,29 and this physiological event may have influenced metformin’s effects. Nevertheless, pubertal progression, particularly after the second year of follow-up, when GFD15 concentrations started to diverge between subgroups, was significantly slower in metformin-treated girls and was accompanied by a lesser decrease in circulating HMW-adiponectin, as compared with the untreated girls. Interestingly, GDF15 treatment in mice increases adiponectin levels and improves insulin sensitivity,30 so it is tempting to speculate that GDF15 could have mediated metformin’s metabolic benefits.
LBW-PP girls did not show a clear weight-reducing effect of metformin despite the increase in circulating GDF15 concentrations and a striking reduction in total and visceral fat after 4 years of treatment. Metformin reduces food intake and body mass in mice fed a high-fat diet in a GDF15-dependent manner, as those effects are reverted in mice lacking GDF15 or its receptor GFRAL.9,31,32 The role of GDF15 in weight regulation is further supported by the observation that transgenic mice overexpressing GDF15 are protected against obesity whereas GDF15-knockout mice gain more weight when placed on a high-fat diet.33,34 In LBW-PP girls, the insulin-driven relative deficit of GDF15 could have been enhanced by the co-presence of increased androgen levels, and thus, despite the apparent reduction of hyperinsulinemia, longer exposure to metformin and relatively higher GDF15 concentrations may have been required to neutralize androgen effects on central GDF15 signaling and thus to trigger the hypothalamic GDF15-GFRA-RET receptor signaling necessary for weight loss.8
Indeed, androgen excess is known to decrease thermogenesis in brown adipose tissue (BAT),35 and metformin is capable of reducing androgen levels and enhancing BAT activity without causing changes in body weight.36,37 Moreover, GDF15 enhances thermogenesis,33 and brown adipocytes secrete GDF15 in response to thermogenic activation.38 Thus, in LBW-PP girls, both metformin-induced decrease in androgen levels and combined metformin and GDF15 activation of thermogenesis could account for the favorable changes in abdominal fat partitioning without necessarily encompassing a reduction in body weight. This hypothesis is strengthened by the fact that BAT is especially abundant in children and its activation during adolescence results in a lesser net gain in adiposity and body weight.39
Circulating GDF15 concentrations associated negatively with markers of insulin resistance, with total and visceral fat, and with androgen levels. These results are in line with recent evidence pointing to GDF15 as a mediator of metformin actions in energy metabolism.31 Recombinant GDF15 administration has been shown to improve glucose tolerance in mice and it has been postulated that GDF15 could be a protective factor for developing diabetes, regardless of former assumptions pointing to GDF15 as a marker of glucose intolerance.40 However, it is still unclear whether GDF15 improves glucose homeostasis exclusively by reducing adiposity or whether it has a direct action to favorably modulate glucose metabolism.40 The relationships between GDF15 and androgens remain poorly understood. The negative association between circulating GDF15 concentrations and androgen levels in LBW-PP girls fits with in vitro studies showing that testosterone is capable to decrease GDF15 secretion through an androgen receptor-mediated pathway.41 Moreover, metformin treatment reduces androgen levels in adolescents and young women with PCOS with and without obesity.42,43 Therefore, the combined effects of metformin on each circulating GDF15 and androgen levels could explain the described associations.
Study limitations include the relatively small number of patients studied, the lack of a placebo group for comparison, and the lack of information regarding early feeding and current dietary intake as well as weight gain during the first years of life. The strengths are the longitudinal nature of the study as well as the co-availability of clinical, endocrine-metabolic, and imaging data.
In conclusion, prepubertal intervention with metformin in “mismatch” prepubertal girls with the sequence of reduced prenatal weight gain and increased postnatal catch-up in weight and PP improves insulin resistance and reduces central adiposity. GDF15 could be thus among the mediators of such metformin effects, especially over the long term.
Data availability
Data corresponding to the original contributions presented in the study are included in the article/Supplementary material. Further inquiries related to raw data will be available from the corresponding authors upon request.
References
de Zegher, F., López-Bermejo, A. & Ibáñez, L. Central obesity, faster maturation, and ‘PCOS’ in girls. Trends Endocrinol. Metab. 29, 815–818 (2018).
Sebastiani, G. et al. The sequence of prenatal growth restraint and post-natal catch-up growth leads to a thicker intima-media and more pre-peritoneal and hepatic fat by age 3-6 years. Pediatr. Obes. 11, 251–257 (2016).
Ong, K. K. et al. Opposing influences of prenatal and postnatal weight gain on adrenarche in normal boys and girls. J. Clin. Endocrinol. Metab. 89, 2647–2651 (2004).
Ibáñez, L., Lopez-Bermejo, A., Díaz, M., Suárez, L. & de Zegher, F. Low-birth weight children develop lower sex hormone binding globulin and higher dehydroepiandrosterone sulfate levels and aggravate their visceral adiposity and hypoadiponectinemia between six and eight years of age. J. Clin. Endocrinol. Metab. 94, 3696–3699 (2009).
Ibáñez, L., Jiménez, R. & de Zegher, F. Early puberty-menarche after precocious pubarche: relation to prenatal growth. Pediatrics 117, 117–121 (2006).
Ibáñez, L., López-Bermejo, A., Díaz, M., Marcos, M. V. & de Zegher, F. Metformin treatment for four years to reduce total and visceral fat in low birth weight girls with precocious pubarche. J. Clin. Endocrinol. Metab. 93, 1841–1845 (2008).
Ibáñez, L., Lopez-Bermejo, A., Diaz, M., Marcos, M. V. & de Zegher, F. Early metformin therapy to delay menarche and augment height in girls with precocious pubarche. Fertil. Steril. 95, 727–730 (2011).
Mullican, S. E. et al. GFRAL is the receptor for GDF15 and the ligand promotes weight loss in mice and nonhuman primates. Nat. Med. 23, 1150–1157 (2017).
Coll, A. P. et al. GDF15 mediates the effects of metformin on body weight and energy balance. Nature 578, 444–448 (2020).
de Zegher, F. et al. The relative deficit of GDF15 in adolescent girls with PCOS can be changed into an abundance that reduces liver fat. Sci. Rep. 11, 7018 (2021).
Glossmann, H. H. & Lutz, O. M. D. Pharmacology of metformin – an update. Eur. J. Pharmacol. 865, 172782 (2019).
Ibáñez, L. et al. Metformin treatment to prevent early puberty in girls with precocious pubarche. J. Clin. Endocrinol. Metab. 91, 2888–2891 (2006).
Ibáñez, L., Lopez-Bermejo, A., Diaz, M., Marcos, M. V. & de Zegher, F. Pubertal metformin therapy to reduce total, visceral, and hepatic adiposity. J. Pediatr. 156, 98–102.e1 (2010).
Ibáñez, L., López-Bermejo, A., Díaz, M., Marcos, M. V. & de Zegher, F. Early metformin therapy (age 8-12 years) in girls with precocious pubarche to reduce hirsutism, androgen excess, and oligomenorrhea in adolescence. J. Clin. Endocrinol. Metab. 96, E1262–E1267 (2011).
Rosenfield, R. L. Normal and almost normal precocious variations in pubertal development premature pubarche and premature thelarche revisited. Horm. Res. 41(Suppl 2), 7–13 (1994).
Ibáñez, L., Potau, N., Francois, I. & de Zegher, F. Precocious pubarche, hyperinsulinism and ovarian hyperandrogenism in girls: relation to reduced fetal growth. J. Clin. Endocrinol. Metab. 83, 3558–3562 (1998).
Marshall, W. A. & Tanner, J. M. Variations in pattern of pubertal changes in girls. Arch. Dis. Child. 44, 291–303 (1969).
Sánchez-Infantes, D. et al. Pharmacokinetics of metformin in girls aged 9 years. Clin. Pharmacokinet. 50, 735–738 (2011).
Schwertmana, N. C., Owens, M. A. & Adnan, R. A simple more general boxplot method for identifying outliers. Computational Stat. Data Anal. 47, 165–174 (2004).
Ibáñez, L., Ong, K., Dunger, D. B. & de Zegher, F. Early development of adiposity and insulin resistance after catch-up weight gain in small-for-gestational-age children. J. Clin. Endocrinol. Metab. 91, 2153–2158 (2006).
Ferrández-Longas, A. et al. Estudio longitudinal de crecimiento y desarrollo. Centro Andrea Prader. Zaragoza 1980-2002. In: Patrones de crecimiento y desarrollo en España (eds Garcia-Dihinx, A., Romo. A. & Ferrandez-Longas, A.) 61–115 (Madrid, Ergon, 2004).
Ibáñez, L. et al. Combined low-dose pioglitazone, flutamide, and metformin for women with androgen excess. J. Clin. Endocrinol. Metab. 92, 1710–1714 (2007).
Díaz, M., Bassols, J., López-Bermejo, A., de Zegher, F. & Ibáñez, L. Metformin treatment to reduce central adiposity after prenatal growth restraint: a placebo-controlled pilot study in prepubertal children. Pediatr. Diabetes 16, 538–545 (2015).
Clayton, P. E. et al. Management of the child born small for gestational age through to adulthood: a consensus statement of the International Societies of Pediatric Endocrinology and the Growth Hormone Research Society. J. Clin. Endocrinol. Metab. 92, 804–810 (2007).
Schernthaner-Reiter, M. H. et al. Growth differentiation factor 15 increases following oral glucose ingestion: effect of meal composition and obesity. Eur. J. Endocrinol. 175, 623–631 (2016).
Gerstein, H. C. et al. Growth Differentiation Factor 15 as a novel biomarker for metformin. Diabetes Care. 40, 280–283 (2017).
Lockhart, S. M., Saudek, V. & O’Rahilly, S. GDF15: a hormone conveying somatic distress to the brain. Endocr. Rev. 41, 610–642 (2020).
Amiel, S. A., Sherwin, R. S., Simonson, D. C., Lauritano, A. A. & Tamborlane, W. V. Impaired insulin action in puberty. A contributing factor to poor glycemic control in adolescents with diabetes. N. Engl. J. Med. 315, 215–219 (1986).
Kelsey, M. M. & Zeitler, P. S. Insulin resistance of puberty. Curr. Diab Rep. 16, 64 (2016).
Tsai, V. W. et al. Treatment with the TGF-b superfamily cytokine MIC-1/GDF15 reduces the adiposity and corrects the metabolic dysfunction of mice with diet-induced obesity. Int J. Obes. (Lond.) 42, 561–571 (2018).
Day, E. A. et al. Metformin-induced increases in GDF15 are important for suppressing appetite and promoting weight loss. Nat. Metab. 1, 1202–1208 (2019).
Yang, M. et al. Inhibition of mitochondrial function by metformin increases glucose uptake, glycolysis and GDF-15 release from intestinal cells. Sci. Rep. 11, 2529 (2021).
Chrysovergis, K. et al. NAG-1/GDF-15 prevents obesity by increasing thermogenesis, lipolysis and oxidative metabolism. Int. J. Obes. (Lond.). 38, 1555–1564 (2014).
Tran, T., Yang, J., Gardner, J. & Xiong, Y. GDF15 deficiency promotes high fat diet-induced obesity in mice. PLoS. One 13, e0201584 (2018).
Lerner, A. et al. Androgen reduces mitochondrial respiration in mouse brown adipocytes: a model for disordered energy balance in polycystic ovary syndrome. Int. J. Mol. Sci. 22, 243 (2020).
Viollet, B. et al. Cellular and molecular mechanisms of metformin: an overview. Clin. Sci. (Lond.) 122, 253–270 (2012).
Karise, I., Bargut, T. C., Del Sol, M., Aguila, M. B. & Mandarim-de-Lacerda, C. A. Metformin enhances mitochondrial biogenesis and thermogenesis in brown adipocytes of mice. Biomed. Pharmacother. 111, 1156–1165 (2019).
Campderrós, L. et al. Brown adipocytes secrete GDF15 in response to thermogenic activation. Obesity (Silver Spring) 27, 1606–1616 (2019).
Gilsanz, V., Hu, H. H. & Kajimura, S. Relevance of brown adipose tissue in infancy and adolescence. Pediatr. Res. 73, 3–9 (2013).
Breit, S. N., Brown, D. A. & Tsai, V. W. The GDF15-GFRAL pathway in health and metabolic disease: friend or foe? Annu. Rev. Physiol. 83, 127–151 (2021).
Liu, H., Dai, W., Cui, Y., Lyu, Y. & Li, Y. Potential associations of circulating growth differentiation factor-15 with sex hormones in male patients with coronary artery disease. Biomed. Pharmacother. 114, 108792 (2019).
Ibáñez, L. et al. An International Consortium Update: pathophysiology, diagnosis, and treatment of polycystic ovarian syndrome in adolescence. Horm. Res. Paediatr. 88, 371–395 (2017).
Li, Y. et al. Comparing the individual effects of metformin and rosiglitazone and their combination in obese women with polycystic ovary syndrome: a randomized controlled trial. Fertil. Steril. 113, 197–204 (2020).
Acknowledgements
M.D. and L.I. are clinical investigators of CIBERDEM (www.ciberdem.org); G.C.-B. is an Investigator of the Sara Borrell Fund of Scientific Research from Carlos III National Institute of Health /CD19-00172); J.V., A.G.-N., and F.V. are investigators of CIBEROBN (www.ciberobn.org); A.L.-B. is a clinical investigator of the I3 Fund for Scientific Research (Ministry of Science and Innovation, Spain).
Funding
This work was supported by a PERIS-SLT006/17/00140 grant from the AQU, Generalitat de Catalunya, Spain.
Author information
Authors and Affiliations
Contributions
M.D. and G.C.-B. equally contributed to literature search, design of figures and tables, data collection, data analysis and interpretation, and wrote the manuscript. J.V. and A.G-N. researched data and contributed to data interpretation. F.d.Z. contributed to data interpretation and reviewed/edited the manuscript. A.L.-B. and J.B. reviewed/edited the manuscript. L.I. and F.V. equally contributed to study design, literature search, data analysis and interpretation, wrote the manuscript, and reviewed/edited the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate
Informed consent was obtained from the parents and assent from the children included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Díaz, M., Carreras-Badosa, G., Villarroya, J. et al. Circulating GDF15 concentrations in girls with low birth weight: effects of prolonged metformin treatment. Pediatr Res 93, 964–968 (2023). https://doi.org/10.1038/s41390-022-02175-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02175-9