Abstract
Background
The rates, outcomes, and long-term trends of stroke complicating the use of extracorporeal membrane oxygenation (ECMO) have been inconsistently reported. We compared the outcomes of pediatric ECMO patients with and without stroke and described the frequency trends between 2000 and 2017.
Methods
Using the National Inpatient Sample (NIS) database, pediatric patients (age ≤18 years) who received ECMO were identified using ICD-9&10 codes. Binary, regression, and trend analyses were performed to compare patients with and without stroke.
Results
A total of 114,477,997 records were reviewed. Overall, 28,695 (0.025%) ECMO patients were identified of which 2982 (10.4%) had stroke, which were further classified as hemorrhagic (n = 1464), ischemic (n = 1280), or combined (n = 238). Mortality was higher in the hemorrhagic and combined groups compared to patients with ischemic stroke and patients without stroke. Length of stay (LOS) was significantly longer in stroke vs. no-stroke patients. Hypertension and septicemia were more encountered in the hemorrhagic group, whereas the combined group demonstrated higher frequency of cardiac arrest and seizures.
Conclusions
Over the years, there is an apparent increase in the diagnosis of stroke. All types of stroke in ECMO patients are associated with increased LOS, although mortality is increased in hemorrhagic and combined stroke only.
Impact
-
Stroke is a commonly seen complication in pediatric patients supported by ECMO.
-
Understanding the trends will help in identifying modifiable risk factors that predict poor outcomes in this patient population.
Similar content being viewed by others
Introduction
Extracorporeal membrane oxygenation (ECMO) is a potentially lifesaving intervention that can be used in patients with respiratory failure and/or severe cardiovascular failure that can be secondary to a myriad of disease processes. ECMO is associated with several complications, some of which can be very debilitating with profound impact on the mortality and morbidity of patients. Indeed, ECMO is often utilized when a catastrophic event happens, and therefore mortality and majority of morbidities are attributed to the underlying degree of illness and to the events patients’ experience prior to ECMO cannulation. While on ECMO, children often have severely abnormal electroencephalogram background with or without electrographic seizures.1 A recent systematic review demonstrated a wide range of disabilities in children who have received ECMO.2 The exposure of blood to the extracorporeal circuit can incite the coagulation cascade, thus substantially increasing the possibility of clots that can lead to thromboembolic stroke. There is a need for systemic anticoagulation for patients on ECMO to prevent clots; this in effect can cause bleeding. Therefore, patients are at risk for having both ischemic and hemorrhagic strokes. Of note, the use of anticoagulants within therapeutic range does not necessarily cause stroke. Nonetheless, stroke is likely to develop in the brain after a catastrophic event with associated anoxic, ischemia, and reperfusion injury. The increased intracranial venous pressure due to cannulation of the internal jugular vein may contribute to the development of subdural and subarachnoid hemorrhages in ECMO patients. Children with all types of stroke have persistent neurologic deficits, developmental problems, learning disabilities, or long-term seizure disorder in up to 66% of cases, sometimes persisting into adulthood.3,4 This potential lifelong disability underscores the importance of studying the contributory factors of pediatric stroke. The incidence and outcomes of stroke complicating pediatric ECMO has been inconsistently reported. An understanding of set-up and attributes can help to identify modifiable factors. Multiple studies have reported the incidence of stroke in pediatric ECMO patients as ranging between 5 and 27.7%.5,6 These reported rates are alarmingly high when compared to the incidence of pediatric arterial ischemic stroke in non-ECMO patients, which is 25–40 per 100,000 live births and 1.2–8 per 100,000 in older children.7,8,9,10 The majority of pediatric ischemic stroke patients will leave the hospital with neurologic deficits.6,11,12,13,14,15 The increased mortality might be attributed to iatrogenic with diversion of management plan to comfort after diagnosing stroke in ECMO patients.
The objective of this study is to assess the prevalence of each type of stroke in pediatric ECMO patients, including ischemic, hemorrhagic, and combined stroke. Analysis of mortality, comorbidities, length of hospital stay (LOS), and hospital cost associated with stroke are performed using a large national inpatient sample.
Methods
Data
Data were obtained from the National Inpatient Sample (NIS), which is part of the Healthcare Cost and Utilization Project (HCUP), sponsored by the Agency for Healthcare Research and Quality (AHRQ). This is the largest publicly available all-payer inpatient care database in the United States (US), containing data from more than seven million hospital stays each year. The NIS database randomly samples 20% of the discharges from participating hospitals in 47 US states and the District of Columbia. The study population was identified using the International Classification of Diseases, Ninth and Tenth Revisions, Clinical Modification (ICD-9&10-CM). Data were queried from the years of 2000 to 2017. HCUP data are publicly available and de-identified. It does not require Institutional Review Board approval as confirmed by AHRQ.
Patient selection
Pediatric patients (≤18 years of age) who had ECMO during their in-hospital stay between 1 January, 2000 and 31 December, 2017 were included in the study. ECMO utilization was defined using ICD-9&10-CM procedure codes 39.65, 39.66, 5A15223, 5A1522F, 5A1522G, 5A1522H, 5A15A2F, 5A15A2G, and 5A15A2H. Patients were divided into two groups, stroke and no-stroke, using ICD-9&10-CM diagnosis codes for both ischemic, hemorrhagic, and combined (ischemic & hemorrhagic) stroke. Supplementary Table 1 (Table S1) includes all used codes for stroke. Patient demographics collected include age at admission, sex, ethnicity, and bed size of the hospital. Outcomes measured were in-hospital mortality, LOS, and cost of hospitalization. In addition, we identified a list of procedures and complications before the primary analysis using ICD-9&10-CM codes, and these included respiratory intubation and mechanical ventilation, ventricular assist device (VAD), tracheostomy, cardiac catheterization, acute kidney injury (AKI), hemodialysis, vasopressor use, and heart transplantation.
Data analysis
Continuous variables were described using median and interquartile range (IQR). Categorical variables were described using frequencies and percentages. Demographics, clinical characteristics, and outcomes were compared using Mann–Whitney U test for continuous variables and chi-square or Fisher’s exact tests for categorical variables. Regression analyses were performed to identify significant factors associated with stroke and to assess the association of stroke with mortality after controlling for these confounding variables. All comparisons were two tailed and statistical significance was set at p < 0.05. Cochrane–Armitage trend test was used to study the trends for ECMO, stroke, and mortality. Statistical analysis was performed by the SPSS software, version 25 (SPSS Inc., Chicago, IL).
Results
Demographics
A total of 114,477,997 records were obtained. Of them, 28,695 (0.025%) were identified as pediatric ECMO patients. Demographics of the stusy population are presented in Table 1. The majority of pediatric ECMO population was in the neonatal age group that contributed 14,485 (50.1%) of the total pediatric ECMO cases. Figure 1 demonstrates the frequency distribution of pediatric ECMO patients in different age groups. Within the ECMO population, 2982 (10.4%) had stroke. The types of stroke were hemorrhagic (n = 1464, 49%), ischemic (n = 1280, 43%), and combined (n = 238, 8%). The demographic characteristics of this cohort is presented in Supplemental Table 1. Patients were categorized by age, sex, and ethnicity. The number of infants (<1 year old) were 21,203 (73.9%) vs. 7492 (26.1%) patients between ages 1 and 18 years. More than half of the population (50.5%) were neonates (n = 14,485). The frequency of stroke was more common in 1–18-year-old patients as compared to patients <1 year of age (15.4 vs. 8.6%, p < 0.001). There was no difference in the frequency of stroke in females compared to males (10.7% vs. 10.1%, p = 0.102). There was no significant difference in frequency of stroke when compared by ethnicity (p = 0.213).
Clinical characteristics of patients with stroke
When compared to patients without stroke, patients with stroke while on ECMO had higher mortality (46.6% vs. 40.8%, odds ratio (OR) = 1.27, 95% confidence interval (CI): 1.18–1.37, p < 0.001), longer median LOS (33 days vs. 27 days, p < 0.001), and higher median hospital costs ($692,475 vs. $465,513, p < 0.001). Further, among the subgroups, mortality was the highest in the hemorrhagic group (53.8%) and lowest in the ischemic group (38.6%). The combined group had the longest median LOS (60 days), along with highest median hospital costs ($879,816) compared to the hemorrhagic and ischemic groups (Table 2).
Pediatric patients supported by ECMO frequently have comorbidities. Patients with all types of stroke were found to have higher frequency of cardiac comorbidities when compared with patients without stroke on ECMO. These differences, as illustrated in Table 2, include hypertension (10.8 vs. 7.3%, p < 0.001), cardiac arrest (32.3 vs. 18.5%, p < 0.001), myocarditis (6.3 vs. 2.8%, p < 0.001), congenital heart disease (58.4 vs. 57.3%, p < 0.001), AKI (42.7 vs. 27.1%, p < 0.001), VAD (6.5 vs. 1.4%, p < 0.001), heart failure (34.6 vs. 19.0%, p < 0.001), and cardiomyopathy (13.8 vs. 6.0%, p < 0.001). Within the subgroups, the hemorrhagic group had higher frequency of hypertension (12.3%) and septicemia (36.7%), whereas the ischemic group demonstrated higher frequency of myocarditis (7.6%) and shock (36.8%). The combined group showed higher prevalence of cardiac arrest (52.1%), heart failure (52.7%), cardiomyopathy (14.9%), seizures (16.8%), acute renal failure (52.6%), and VAD (14.9%). When using regression analysis, stroke was associated with increased mortality (adjusted OR (aOR) = 1.20, 95% CI: 1.11–1.30, p < 0.001). Other variables associated with mortality included congenital heart disease (aOR = 1.31, CI: 1.24–1.38, p < 0.001), cardiac arrest (aOR = 1.68, CI: 1.58–1.79, p < 0.001), and shock (aOR = 1.34, CI: 1.26–1.42, p < 0.001). There were less observed mortality in patients with hypertension (aOR = 0.49, CI: 0.44–0.54, p < 0.001) and cardiomyopathy (aOR = 0.71, CI: 0.64–0.78, p < 0.001). Additional regression analyses were performed for associated morbidities in patients with hemorrhagic stroke and ischemic stroke (Table 3). Factors associated with mortality in hemorrhagic stroke and ischemic stroke patients are shown in the regression analysis in Table 4. In the neonatal ECMO population (n = 14,485), hemorrhagic stroke was associated with mortality (aOR = 1.95, CI: 1.58–2.41), whereas ischemic stroke did not associate with mortality. Factors associated with mortality in the neonatal ECMO population are presented in Table S2.
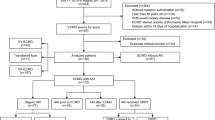
Trend analysis showed significant increase in ECMO utilization over the years of the study period (p < 0.001, Fig. 2). The mortality rate in ECMO patients significantly decreased over the years of the study period (p < 0.001, Fig. 2), whereas the diagnosis of stroke in pediatric ECMO patients had significantly increased from 3.2% in 2000 to 13.7% in 2017. The trends for apparent increase in stroke diagnosis over the study years were significant for both hemorrhagic stroke and ischemic stroke (p < 0.001, Fig. 2).
Panel a demonstrates ECMO utilization during the study period (2000–2017). Panel b represents stroke diagnosis for pediatric ECMO patients (solid line), including hemorrhagic stroke (dashed line) and ischemic stroke (dotted line). Panel c represents mortality trends during the study period. There were significant trends for increased ECMO utilization (p < 0.001), increased diagnosis of overall stroke and its two subtypes in pediatric ECMO patients (p < 0.001), and decreased ECMO mortality (p < 0.001).
Discussion
Pediatric stroke is uncommon, but the impact on the developing brain can be severe with potential lifelong neurologic injury. The prevalence of pediatric stroke has been reported as between 2 and 13 per 100,000.16,17,18 ECMO is a potentially live-saving device that is used in patients with respiratory failure and/or cardiovascular failure. Patients receiving ECMO are at an increased risk for stroke related to the thrombogenic extracorporeal circuit, and the need for anticoagulation, in addition to underlying hypoxic ischemic events they often experience before starting ECMO. The overall prevalence of stroke in pediatric ECMO patients has been reported as between 3 and 6% according to the Extracorporeal Life Support Organization (ELSO) registry. However, a number of other studies have reported higher prevalence of stoke in pediatric patients receiving ECMO, one study reported a prevalence of 27.7%.5 The prevalence of stroke in pediatric ECMO patients who underwent ECMO cardiopulmonary resuscitation (ECPR) was 9% as reported by ELSO. This study to our knowledge is the first to analyze associated outcomes and trend of the prevalence of stroke in pediatric ECMO patients vs. pediatric patients on ECMO without stroke.
We found the diagnosis of stroke to be significantly higher in older children (1–18 years) than in infants (<1 year). The reason for this is unclear but maybe related to the indication for ECMO use, which according to ELSO registry is mainly cardiac (60%) for patients aged >28 days to 18 years with about 30% being ECPR vs. mostly respiratory indication (55%) for patients aged <28 days. The prevalence of stroke on venoarterial (VA) ECMO is higher than in patients placed on venovenous (VV) ECMO.19
Pediatric patients with hemorrhagic stroke while on ECMO had a higher mortality rate than those without stroke, although ischemic stroke was not associated with increased mortality. The apparent increased mortality in stroke patients could be iatrogenic; managing team along with family may decide diverting management to palliative care after identifying stroke in ECMO patients. The published outcomes in ELSO showed increased mortality in stroke patients and highlighted the need for meticulous monitoring of anticoagulation for patients on ECMO and prompt identification of clots in the ECMO circuit. This concern for need of reliable anticoagulation has resulted in the increasing use of direct thrombin inhibitors for anticoagulation.20,21 However, the rational for decreased mortality in ECMO patients with ischemic stroke is unclear. We speculate that the diagnosis of ischemic stroke in many patients could have been incidental, that is, made in follow-up imaging studies in ECMO survivors, whereas it could have been missed in patients who died.
Pediatric patients with stroke on ECMO have significantly longer LOS than in those without stroke. The increased LOS substantially increases hospital cost. There is additional cost of rehabilitation for some of these patients after discharge, and the added cost of potential lifelong disability.22,23
We found a significantly higher prevalence of stroke in pediatric ECMO patients with congenital heart disease mostly beyond the first year of life. This is consistent with prior study by Brunetti et al. with a stroke incidence of 11% in multi-institutional pediatric cardiac intensive care units.24,25 This higher incidence is insightful because it heightens the awareness of the risk and need for meticulous anticoagulation monitoring in these patients. Pediatric patients on VAD are at an increased risk for stroke.26,27 This is consistent with our findings of higher stroke rates in pediatric patients on ECMO with VAD compared to those without VAD. Pediatric heart failure and cardiomyopathy are well-established risk factors for stroke secondary to poor heart function and diminished left ventricular ejection, with resultant stasis of blood. Our study found a significant increase in stroke in pediatric patients on ECMO with heart failure and cardiomyopathy as comorbidities.
This study reported stroke in 10.4% of pediatric ECMO patients, that is, significantly higher than 3–6% reported by ELSO. The current study is inclusive to the entire nation reflecting the real rate of stroke in the United States. ELSO is the largest known registry for ECMO patients; however, it is not inclusive to all ECMO centers. Stroke was hemorrhagic in 49%, ischemic in 43%, and combined in 8% of patients in the current study. Both types of stroke were more frequently encountered in ECMO patients with associated diagnoses of dysrhythmia, cardiac arrest, cardiomyopathy, sepsis, and shock. It is plausible that these diagnoses directly attribute to hemodynamic instability that leads to stroke. However, the dataset does not provide temporal relationship of these factors with stroke; therefore, the role of these variables in the development of stroke should be interpreted with caution and a cause-and-effect link cannot be systematically assumed. In addition to these factors, hemorrhagic stroke was associated with hypertension and congenital heart diseases, whereas ischemic stroke was associated with gastrointestinal hemorrhage. The risk for seizures was significantly increased in both hemorrhagic and ischemic stroke. Stroke was associated with increased mortality (aOR = 1.20, 95%CI: 1.11–1.30) that was mainly driven from hemorrhagic stroke (aOR = 1.66, CI: 1.49–1.86). In fact, ischemic stroke was associated with decreased mortality (aOR = 0.82, CI: 0.73–0.92). The presence of seizures does not influence mortality in either hemorrhagic or ischemic stroke patients.
The mortality rate of pediatric patients on ECMO has decreased over the years of the study period despite an increased use of ECMO during that period. This could be as a result of better understanding and improvement of the management of patients on ECMO. The prevalence of AKI in patients on ECMO increased significantly over the study period. This is likely because of better identification of pediatric AKI, especially following a more formalized definition of pediatric AKI with the PRIFLE criteria.28,29
The diagnosis of stroke in pediatric patients receiving ECMO has significantly increased over the study period. The apparent increase in stroke could be a reflection of increased survival of ECMO patients with potentially longer ECMO duration or it may be attributed to increased detection of stroke with improved bedside imaging. Nonetheless, the apparent increase in stroke may be related to the willingness to place more complex patients on ECMO, and enhanced reporting of complications related to ECMO. In addition, improved bedside imaging technologies could have contributed to the increased ability to identify brain lesions.
The study utilized NIS dataset that represents the entire nation, thereby providing an accurate national estimate of ECMO survival and stroke diagnosis. Having multiple years in the analysis allowed to examine trends for diagnoses and survivals. However, the study inherited some limitations as a retrospective observational study that is dependent on reporting by hospitals to a database. The functional implication of the reported strokes could not be determined based on the reporting system. The dataset does not provide the duration of ECMO that certainly contribute to the risk for stroke, nor does it include information on anticoagulant use and coagulation profiles. The relationship of the prevalence and type of stroke with ECMO type (VV vs. VA) was not achievable. Nonetheless, previous studies demonstrated wide variation in stroke rate and could not associate specific ECMO type or cannulation site with stroke.30 In addition, long-term follow-up are not available in the inpatient setting.
In conclusion, stroke in pediatric patients can lead to debilitating lifelong disability. An understanding of the contributing risk factors can enhance our knowledge on how to manage these patients and potentially modify some of these factors to ultimately decrease the incidence of strokes in these critically ill children. While the mortality of pediatric EMCO patients has decreased over the years, stroke is an increasingly recognized complication in pediatric ECMO patients and has important implications for patient outcomes. Further efforts need to be directed toward preventing, recognizing, and treating stroke in this population.
Data availability
Data for this research were extracted from the publically available Healthcare Cost and Utilization Project (HCUP), sponsored by the Agency for Healthcare Research and Quality (AHRQ).
References
Sansevere, A. J. et al. EEG features of brain injury during extracorporeal membrane oxygenation in children. Neurology 95, e1372–e1380 (2020).
Boyle, K. et al. Neurologic outcomes after extracorporeal membrane oxygenation: a systematic review. Pediatr. Crit. Care Med. 19, 760–766 (2018).
Goldenberg, N. A. et al. Antithrombotic treatments, outcomes, and prognostic factors in acute childhood-onset arterial ischaemic stroke: a multicentre, observational, cohort study. Lancet Neurol. 8, 1120–1127 (2009).
Bembea, M. M. et al. Neurologic outcomes in a two-center cohort of neonatal and pediatric patients supported on extracorporeal membrane oxygenation. ASAIO J. 66, 79–88 (2020).
Pinto, V. L. et al. Brain magnetic resonance imaging findings in pediatric patients post extracorporeal membrane oxygenation. ASAIO J. 63, 810–814 (2017).
Hervey-Jumper, S. L. et al. Neurological complications of extracorporeal membrane oxygenation in children. J. Neurosurg. Pediatr. 7, 338–344 (2011).
Agrawal, N., Johnston, S. C., Wu, Y. W., Sidney, S. & Fullerton, H. J. Imaging data reveal a higher pediatric stroke incidence than prior US estimates. Stroke 40, 3415–3421 (2009).
Felling, R. J. et al. Predicting recovery and outcome after pediatric stroke: results from the International Pediatric Stroke Study. Ann. Neurol. 87, 840–852 (2020).
Kleindorfer, D. et al. Temporal trends in the incidence and case fatality of stroke in children and adolescents. J. Child Neurol. 21, 415–418 (2006).
Fullerton, H. J., Wu, Y. W., Zhao, S. & Johnston, S. C. Risk of stroke in children: ethnic and gender disparities. Neurology 61, 189–194 (2003).
Goeggel Simonetti, B. et al. Long-term outcome after arterial ischemic stroke in children and young adults. Neurology 84, 1941–1947 (2015).
Steinlin, M., Roellin, K. & Schroth, G. Long-term follow-up after stroke in childhood. Eur. J. Pediatr. 163, 245–250 (2004).
deVeber, G. A., MacGregor, D., Curtis, R. & Mayank, S. Neurologic outcome in survivors of childhood arterial ischemic stroke and sinovenous thrombosis. J. Child Neurol. 15, 316–324 (2000).
Elbers, J., deVeber, G., Pontigon, A. M. & Moharir, M. Long-term outcomes of pediatric ischemic stroke in adulthood. J. Child Neurol. 29, 782–788 (2014).
deVeber, G. A. et al. Epidemiology and outcomes of arterial ischemic stroke in children: The Canadian Pediatric Ischemic Stroke Registry. Pediatr. Neurol. 69, 58–70 (2017).
Cooper, A. N. et al. Trajectories of motor recovery in the first year after pediatric arterial ischemic stroke. Pediatrics 140, e20163870 (2017).
Kirton, A., Westmacott, R. & deVeber, G. Pediatric stroke: rehabilitation of focal injury in the developing brain. Neurorehabilitation 22, 371–382 (2007).
Felling, R. J., Sun, L. R., Maxwell, E. C., Goldenberg, N. & Bernard, T. Pediatric arterial ischemic stroke: epidemiology, risk factors, and management. Blood Cells Mol. Dis. 67, 23–33 (2017).
Maslach-Hubbard, A. & Bratton, S. L. Extracorporeal membrane oxygenation for pediatric respiratory failure: history, development and current status. World J. Crit. Care Med. 2, 29–39 (2013).
Sanfilippo, F. et al. Bivalirudin for alternative anticoagulation in extracorporeal membrane oxygenation: a systematic review. J. Intensive Care Med. 32, 312–319 (2017).
Netley, J. et al. Bivalirudin anticoagulation dosing protocol for extracorporeal membrane oxygenation: a retrospective review. J. Extra Corpor. Technol. 50, 161–166 (2018).
Lo, W. et al. The cost of pediatric stroke care and rehabilitation. Stroke 39, 161–165 (2008).
Hamilton, W., Huang, H., Seiber, E. & Lo, W. Cost and outcome in pediatric ischemic stroke. J. Child Neurol. 30, 1483–1488 (2015).
Brunetti, M. A. et al. Characteristics, risk factors, and outcomes of extracorporeal membrane oxygenation use in pediatric cardiac ICUs: a report from the Pediatric Cardiac Critical Care Consortium Registry. Pediatr. Crit. Care Med. 19, 544–552 (2018).
Werho, D. K. et al. Epidemiology of stroke in pediatric cardiac surgical patients supported with extracorporeal membrane oxygenation. Ann. Thorac. Surg. 100, 1751–1757 (2015).
Stowe, R. C., Kan, P., Breen, D. B. & Agarwal, S. Mechanical thrombectomy for pediatric acute stroke and ventricular assist device. Brain Dev. 40, 81–84 (2018).
Huang, J. Y. et al. Bleeding and thrombotic events occur early in children on durable ventricular assist devices. Thromb. Res. 173, 65–70 (2019).
Akcan-Arikan, A. et al. Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int. 71, 1028–1035 (2007).
Thomas, M. E. et al. The definition of acute kidney injury and its use in practice. Kidney Int. 87, 62–73 (2015).
Sorokin, V., MacLaren, G., Vidanapathirana, P. C., Delnoij, T. & Lorusso, R. Choosing the appropriate configuration and cannulation strategies for extracorporeal membrane oxygenation: the potential dynamic process of organ support and importance of hybrid modes. Eur. J. Heart Fail 19(Suppl. 2), 75–83 (2017).
Funding
No funding was secured for this study.
Author information
Authors and Affiliations
Contributions
C.E. and O.B. conceptualized the study, drafted initial manuscript, and reviewed and revised the manuscript. H.F.O. analyzed the data and reviewed the manuscript. S.L. and V.N. critically reviewed the manuscript. H.A. conceptualized the study and critically reviewed the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
No patient consent was required for the purpose of this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ezetendu, C., Baloglu, O., Othman, H.F. et al. Stroke in pediatric ECMO patients: analysis of the National Inpatient Sample (NIS) database. Pediatr Res 92, 754–761 (2022). https://doi.org/10.1038/s41390-022-02088-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02088-7
This article is cited by
-
Neurophysiologic Features Reflecting Brain Injury During Pediatric ECMO Support
Neurocritical Care (2024)
-
Stroke in pediatric ECMO: a target for prevention and improvement
Pediatric Research (2022)