Abstract
Background
Extremely preterm infants are prone to hyperbilirubinemia and its sequelae. Currently recommended thresholds for initiating phototherapy in these newborns are consensus-based (CB).
Methods
A multi-site retrospective cohort study of 642 infants born at 240/7 to 286/7 weeks’ gestation, between January 2013 and June 2017, was conducted at three NICUs in Canada. Pre-phototherapy TSB percentile levels at 24 h of age were generated and contrasted with published CB thresholds.
Results
Among infants born 240/7 to 256/7 weeks’ gestation, the differences between our TSB percentiles vs. the CB threshold of 85.0 µmol/L were 10.0 µmol/L (95% CI, 6.0–16.0) at the 75th percentile and 35.3 µmol/L (95% CI, 26.1–42.8) at the 95th percentile. Respectively, among infants born at 260/7 to 276/7 weeks, differences were 19.4 µmol/L (95% CI, 16.8–23.4) and 43.3 µmol/L (95% CI, 34.7–46.9). Born at 280/7 to 286/7 weeks’ gestation, differences between our 75th and 95th TSB percentiles and the CB threshold of 103 µmol/L were 6.9 µmol/L (95% CI, 3.2–12.0) and 36.0 µmol/L (95% CI, 31.0–44.3), respectively.
Conclusions
We provide statistically derived pre-phototherapy TSB levels that may clarify patterns of pre-phototherapy TSB levels in extremely preterm infants.
Impact
-
We present statistically derived pre-phototherapy total serum bilirubin levels in a cohort of extremely preterm infants.
-
Most of these preterm infants received phototherapy—some at below currently published thresholds.
-
There are notable differences between our statistically derived pre-phototherapy TSB levels and currently published lower limit TSB thresholds for phototherapy.
-
Our study results assist in the understanding of pre-phototherapy TSB levels in extremely preterm infants.
Similar content being viewed by others
Introduction
Infants born extremely preterm at 24–28 weeks’ gestation are at higher risk of bilirubin-induced neurological dysfunction (BIND). BIND can arise in preterm infants in the absence of acute bilirubin encephalopathy (ABE) and at a total serum bilirubin (TSB) concentrations lower than those in term or near-term infants.1,2,3,4
In an attempt to prevent BIND in extremely preterm infants, TSB levels are monitored more frequently than in term infants, and at-risk infants are typically treated at lower TSB levels than their term and moderate preterm infant counterparts.1,3,4 Although pre-phototherapy TSB levels have been established among term and near-term infants, less is known about the pattern of pre-phototherapy TSB levels in extremely preterm infants. Rather, TSB treatment thresholds that are currently in use were primarily derived from expert opinion, consensus guidelines, and small cohort studies, potentially impacting hyperbilirubinemia management in extremely preterm infants.5,6,7,8
In 2012, Maisels et al. introduced recommendations to manage and treat hyperbilirubinemia in preterm infants born at <35 weeks’ gestation, largely based on expert opinion.6 A lack of evidence regarding the appropriateness of these recommendations has led to different adaptations and variations in their use across neonatal intensive care units (NICUs), potentially resulting in an increase use of phototherapy in this population.9 In addition, phototherapy use among extremely preterm infants in Canada has not yet been reported.
The primary objective of the current study was to first generate percentile-based pre-phototherapy TSB levels in a cohort of extremely preterm infants born at 240/7 to 286/7 weeks’ gestation. The secondary objective of this study was to compare this cohort’s TSB percentiles with Maisels’ consensus-based published thresholds for phototherapy initiation.6 Additionally, the proportion of infants who were started on phototherapy below Maisels’ published threshold,6 overall, and by hours of age of phototherapy initiation was also calculated.
Methods
A multi-site retrospective cohort study of extremely preterm infants born or transferred to Sinai Health (January 2015 to June 2017) and St. Michael’s Hospital (January 2013 to June 2017) in Toronto, Ontario, as well as at Hamilton Health Sciences Centre (January 2014 to June 2017) in Hamilton, Ontario was conducted. Research ethics board approval was obtained at all three participating sites; Mount Sinai Hospital Research Ethics Board, Unity Health Toronto Research Ethics Board, and Hamilton Integrated Research Ethics Board. Informed consent was not required for this study as this was a retrospective chart review.
Extremely preterm infants born at 240/7 to 286/7weeks gestational age were included in the study. Excluded were infants who had Rh disease or those who did not have a recorded TSB level in their electronic medical chart. Infants with Rh disease are usually diagnosed and managed prenatally by monitoring maternal antibody levels, surveillance fetal sonography and offering selective interventions. National and provincial databases, the Canadian Neonatal Network (CNN)10 and Better Outcomes Registry & Network (BORN),11 respectively, were used to identify eligible infants born during the study period. Eligible infants’ medical records were reviewed at their respective hospitals of admission to obtain pre-phototherapy TSB levels. As previously defined, pre-phototherapy TSB levels included TSB levels prior to the initiation of phototherapy, among those administered phototherapy, or any TSB level among those who were not administered phototherapy.12 In addition, postnatal age in hours, phototherapy status, hours of age at phototherapy initiation, gestational age at birth, and relevant infant characteristics was also collected.
Data analyses
All hour-specific TSB levels prior to initiation of phototherapy were plotted in 6-h increments, from birth to 72 h thereafter. In keeping with previous research, hour-specific 40th, 50th, 75th, and 95th TSB percentiles12,13 were estimated using quantile regression among all infants, including a quadratic polynomial for age in hours. All quantile regression models were fit using the quantreg package in R. In order to account for repeated measures within subjects, 1000 bootstrap resamples at the subject level were used to generate 95% confidence intervals (CIs).14,15,16
Maisels’ recommended published thresholds for the initiation of phototherapy are based on expert opinion.6 Among infants born at 240/7 to 276/7 weeks’ gestation, the recommended TSB range for starting phototherapy is 85–103 μmol/L while among infants born at 280/7 to 286/7 weeks’ gestation the recommended published threshold is 103–137 μmol/L.6 Based on previous reports suggesting that pre-phototherapy TSB at 24 h can be used to guide phototherapy administration, as a secondary analysis, the difference between pre-phototherapy TSB percentiles derived at 24 h of age and Maisels’ above mentioned lower TSB threshold at the respective gestational age groups were calculated.4 A previous study reported NICUs using the lowest level of Maisels’ published threshold to initiate phototherapy among infants born at <28 weeks’ gestation.9 The differences between the study’s pre-phototherapy TSB percentiles at 24 h of age and Maisels’ published lower threshold6 were stratified by the following gestational age groups based on clinical guidelines; 240/7 to 256/7 weeks, 260/7 to 276/7 weeks and 280/7 to 286/7 weeks’ gestation.
Additionally, we determined the proportion of infants in the study who were started on phototherapy below Maisels’ published threshold6. Infants with a TSB level done >12 h before the time of phototherapy initiation were excluded from the secondary analysis. Among infants born at 240/7 to 276/7 weeks’ gestation, those who had a TSB level <85 μmol/L at the time of phototherapy initiation were considered as being treated below Maisels’ published threshold.6 For infants born at 280/7 to 286/7 weeks’ gestation, those whose TSB level was <103 μmol/L at the initiation of phototherapy were considered as being treated below Maisels’ published threshold. To determine whether the proportion of infants administered phototherapy below Maisels’ published threshold changed with time of phototherapy initiation (in hours) since birth, a Cochran–Armitage trend test was conducted, with significance set at <0.01.17,18
Sample size calculation
The sample size was calculated based on previous pre-phototherapy curves for TSB levels in moderate preterm and near-term infants.12,13 A minimum sample size of 448 extremely preterm infants was required using Bellera and Hanley’s methods for reference limits of 2.5% and 97.5%, with a 90% CI and 10% relative margin of error.19
Results
Of the 737 eligible infants born between 240/7 and 286/7 weeks’ gestation, 642 infants had at least one available TSB measurement performed prior to the initiation of phototherapy within the first 72 h after birth (Supplemental Fig. S1). The median gestational age at birth was 26.0 weeks (Interquartile range [IQR]) 25.0–28.0), and the median birth weight was 900.0 g (IQR 760.0–1100.0) (Table 1).
Pre-phototherapy TSB levels
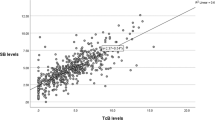
Six hundred and forty-two extremely preterm infants born at 240/7 to 286/7 weeks’ gestation contributed a total of 1134 h-specific pre-phototherapy TSB levels (Fig. 1). Each infant contributed a median of 2 (IQR 1–2) pre-phototherapy TSB samples. Since there was a paucity of pre-phototherapy TSB levels after 72 h of age, quantile regression was limited to data up to 72 h after birth.
At 24 h of age, the estimated pre-phototherapy TSB levels were 84.4 µmol/L (95% CI, 82.2–87.0) at the 40th, 89.4 µmol/L (95% CI, 87.5–91.3) at the 50th, 103.3 µmol/L (95% CI, 101.4–106.2) at the 75th, and 130.4 µmol/L (95% CI, 125.7–135.2) at the 95th percentile (Table 2). The corresponding estimated hourly rates of rise of TSB at birth were 2.8 μmol/L/h (95% CI, 2.4–3.5), 2.9 µmol/L/h (95% CI, 2.4–3.2), 2.8 μmol/L/h (95% CI, 2.2–3.6) and 1.9 μmol/L/h (95% CI, 0.7–3.4) for the 40th, 50th, 75th, and 95th percentiles, respectively. The estimated change in the rate of rise of TSB decreased with time since birth at the 40th, 50th, and 75th percentiles; however, this change was not statistically significant at the 95th percentile (p = 0.50; Table 2). Estimated pre-phototherapy TSB percentiles peaked at 53.8 h of age for the 40th percentile, 55.8 h for the 50th percentile, 63.6 h for the 75th percentile, and beyond 72 h of age for the 95th percentile (Table 2 and Fig. 1).
Pre-phototherapy TSB levels by gestational age groups
Among infants born at 240/7 to 256/7 weeks’ gestation, pre-phototherapy TSB percentiles at 24 h of age from birth were 95.0 µmol/L (95% CI, 91.0–101.0) at the 75th percentile and 120.3 µmol/L (95% CI, 111.1–127.8) at the 95th percentile (Table 3). Among those born at 260/7 to 276/7 weeks, the corresponding respective levels were 104.4 µmol/L (95% CI, 101.8–108.4) and 128.3 µmol/L (95% CI 119.7–131.9) (Table 3). For those born at 280/7 to 286/7 weeks’ gestation, the 75th percentile value was 109.9 µmol/L (95% CI, 106.2–115.0), and the 95th percentile value was 139.0 µmol/L (95% CI, 134.0–147.3) (Table 3).
Derived pre-phototherapy TSB percentiles compared with Maisels’ published thresholds
Among infants born at both 240/7 to 256/7, 260/7 to 276/7, and 280/6 to 286/7 weeks’ gestation, our statistically derived pre-phototherapy TSB levels at the 75th and 95th percentiles were higher at 24 h than Maisels’ published threshold (Table 3).
Phototherapy administration among all infants
Overall, 615 infants (95.8%) subsequently received phototherapy, of which 76.6% had started therapy by 36 h of age (Fig. 2). Among these 615 infants, phototherapy was initiated at a mean (SD) of 31.2 (16.2) hours of age and at a mean TSB level of 104.5 (25.0) µmol/L.
Of the 615 infants who were started on phototherapy, three infants were excluded from the analysis below as their last available TSB level was >12 h from the initiation of phototherapy. Among the 612 analyzed infants, 183 (29.9%) were started on phototherapy at a TSB concentration below Maisels’ published threshold.6 Characteristics were similar between newborns who had phototherapy initiated below and above Maisels’ published threshold6 (Supplemental Table S1). For each subsequent 12 h time interval, the proportion of infants administered phototherapy below Maisels’ threshold decreased significantly with hours of age of phototherapy initiation since birth. (Cochran–Armitage trend test p < 0.01; Table 4).
Discussion
In this Canadian retrospective cohort study of extremely preterm infants born at 240/7 to 286/7 weeks’ gestation, pre-phototherapy TSB percentiles were generated for the first 72 h from birth. Given the higher frequency and earlier initiation of phototherapy among this population, pre-phototherapy TSB percentiles at 24 h were then contrasted with Maisels’ currently published consensus-based threshold for phototherapy initiation. At higher percentiles (i.e., 75th and 95th percentiles), there was a notable difference between Maisels’ consensus-based threshold and our study’s generated 24 h pre-phototherapy TSB percentiles. Furthermore, 95.8% of extremely preterm infants were administered phototherapy, and 76.6% were started on phototherapy by 36 h of age. Among those infants who went on to have phototherapy, overall, 29.9% were started on phototherapy below Maisels’ published threshold,6 especially among infants who had phototherapy initiated at ≤12 h of age.
This is the first study to report hour-specific pre-phototherapy TSB percentiles in extremely preterm infants and to compare them to Maisels’ consensus-based published threshold.6 This is also one of the first studies to report the proportion of infants who started phototherapy below Maisels’ published threshold.6 A previous study on phototherapy administration below published thresholds (referred to therein as “subthresholds”) was limited to term and near-term infants and was focused on longer hospital length of stay as a consequence of subthreshold phototherapy.20 The only other North American study on phototherapy in preterm infants was limited to reporting on the frequency and duration of phototherapy and the median TSB level immediately preceding phototherapy.9
Our study’s statistically derived TSB percentile levels at 24 h of age were notably different from Maisels’ lowest consensus-based published threshold.6 Among the 279 infants who started on phototherapy between 24 and 30 h of age, 55.2% and 87.8% would hypothetically have not received phototherapy within that time point had our study’s 75th or 95th percentile cut-points been used instead, respectively (Supplemental Table S2). These hypothetical estimates of the number of infants not starting phototherapy based on our cut-points are also appreciably greater than the 29.7% figure based on Maisels’ lowest threshold (Supplemental Table S2).6 Certainly, these notable differences do not account for the many factors that might influence the decision to initiate phototherapy in an extremely preterm infants or the possibility that phototherapy might otherwise be initiated soon after the 24–30 h of age interval used in this exercise—factors beyond the scope of the current study. Nevertheless, these finding provide novel Canadian data on pre-treatment TSB in extremely preterm infants, for experts to consider patterns of pre-phototherapy TSB levels in extremely preterm infants.
Almost all infants in this study were started on phototherapy by 36 h of age, in keeping with previous reports of increased frequency of phototherapy use in extremely preterm infants.9,21 Consistent with previous research, the estimated change in the rate of rise of TSB levels decreased after birth.12 The potential long-term negative consequences of early initiation or increased frequency of phototherapy use has not been well studied in extremely preterm infants; however, one study found that early initiation is associated with a longer duration of phototherapy.21 Previous studies have been limited to the negative consequences of aggressive or intensive phototherapy in preterm infants of low birth weight.7 Among extremely preterm infants, little is known about the potential benefits and harms of initiating phototherapy below recommended thresholds.6 Hence, more research is needed to determine the reasons for, and impact of, administering phototherapy below percentile-based or recommended thresholds, including long-term developmental follow-up.6
This study has some limitations. First, Maisels’ published thresholds for phototherapy initiation were based on expert opinion and not on data directly measured in extremely preterm infants.6 As such in Canada, Maisels’ published thresholds6 have been further modified within different centers and applied at the discretion of individual clinicians. Additionally, timing of TSB testing was left to clinical judgment and did not include a protocol. Accordingly, this would have resulted in considerable practice variation within our study. As such, we did not report clinical factors that may have impacted decisions to start phototherapy. Notwithstanding, these recommendations have been widely disseminated across North America. Second, some have suggested that lower thresholds for initiating phototherapy are needed in very ill preterm infants.4 The current study was limited to pre-phototherapy TSB levels and phototherapy administration. Future research should focus on differences in phototherapy thresholds by comorbidities and then proceed to compare short- and long-term neonatal outcomes, accordingly. Third, in this study, we compared our statistically derived TSB percentiles with Maisels’ lowest TSB threshold,6 typically used for infants at high risk of neurotoxicity from severe hyperbilirubinemia. However, preterm infants born before 29 weeks’ gestation are considered at higher risk of neurotoxicity from severe hyperbilirubinemia. Additionally, among infants born <28 weeks’ gestation, one previous study reported using the lower TSB threshold level recommended by Maisels.9 It should be reiterated that current guidelines are not solely based on fixed TSB values, and the use of the lower or higher TSB thresholds offered by Maisels also requires consideration of newborn risk factors associated with neurotoxicity.6 In contrast, our statistically estimated pre-phototherapy TSB percentiles, and the differences observed with those of Maisels, should not be used to guide treatment.6 Fourth, the current study did not describe clinical factors that may impact pre-phototherapy TSB levels and the administration of phototherapy below or above Maisels’ threshold.6 The scope of this study was to statistically derive pre-phototherapy TSB levels for preterm infants born extremely preterm and compare them to Maisels’ published threshold.6 Future larger studies should look at neonatal factors and pre-phototherapy TSB levels and administration of phototherapy above and below Maisels’ phototherapy thresholds.6 Finally, all infants born or transferred to all three NICUs were reviewed for inclusion in the primary analysis regardless of age in hours from birth. This resulted in the exclusion of infants without an accessible pre-phototherapy TSB by 72 h of age, due to the initiation of phototherapy prior to transferring to participating study sites or an infant transfer after 72 h of age from birth. These excluded infants may have had different pre-phototherapy TSB levels from the current cohort.
Conclusion
There is considerable variability in the initiation of phototherapy compared to the most commonly recommended treatment thresholds in extremely preterm infants.6 In addition, we report statistically derived pre-phototherapy TSB percentiles from birth to 72 h of age and compared 24-h pre-phototherapy TSB percentiles with existing consensus-based phototherapy guidelines.6 This study highlights the high frequency of phototherapy use in infants born at 24–28 weeks’ gestation and provides a contemporary understanding of pre-phototherapy TSB levels in extremely preterm infants.
Data availability
The datasets generated and analyzed during the current study are not publicly available due to institutional ethics and privacy policies.
References
Bhutani, V. K., Wong, R. J. & Stevenson, D. K. Hyperbilirubinemia in preterm neonates. Clin. Perinatol. 43, 215–232 (2016).
Karimzadeh, P. et al. Bilirubin induced encephalopathy. Iran. J. Child Neurol. 14, 7–19 (2020).
Olds, C. & Oghalai, J. S. Bilirubin-induced audiologic injury in preterm infants. Clin. Perinatol. 43, 313–323 (2016).
Bhutani, V. K. & Wong, R. J. Bilirubin neurotoxicity in preterm infants: risk and prevention. J. Clin. Neonatol. 2, 61–69 (2013).
Hulzebos, C. V., van Dommelen, P., Verkerk, P. H., Dijk, P. H. & Van Straaten, H. L. Evaluation of treatment thresholds for unconjugated hyperbilirubinemia in preterm infants: effects on serum bilirubin and on hearing loss? PLoS ONE 8, e62858 (2013).
Maisels, M. J., Watchko, J. F., Bhutani, V. K. & Stevenson, D. K. An approach to the management of hyperbilirubinemia in the preterm infant less than 35 weeks of gestation. J. Perinatol. 32, 660–664 (2012).
Morris, B. H. et al. Aggressive vs. conservative phototherapy for infants with extremely low birth weight. N. Engl. J. Med. 359, 1885–1896 (2008).
National Institute for Health and Clinical Excellence. Neonatal jaundice. www.nice.org.uk/CG98 (2010).
Mukherjee, D., Coffey, M. & Maisels, M. J. Frequency and duration of phototherapy in preterm infants <35 weeks gestation. J. Perinatol. 38, 1246–1251 (2018).
The Canadian Neonatal Network. The Canadian Neonatal Network. http://www.canadianneonatalnetwork.org/portal/ (2009).
Better Outcomes Registry & Network. Better Outcomes Registry & Network (Born) Ontario. https://www.bornontario.ca/en/index.aspx (2019).
Jegathesan, T. et al. Hour specific total serum bilirubin percentiles for infants born at 29 to 35 weeks’ gestation. Neonatology 118, 710–719 (2021).
Bhutani, V. K., Johnson, L. & Sivieri, E. M. Predictive ability of a predischarge hour-specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near-term newborns. Pediatrics 103, 6–14 (1999).
Karlsson, A. Bootstrap methods for bias correction and confidence interval estimation for nonlinear quantile regression of longitudinal data. J. Stat. Comput Simul. 79, 1205–1218 (2009).
Koenker, R. Quantreg: quantile regression. R package version 5.51 (2009).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2019).
Armitage, P. Tests for linear trends in proportions and frequencies. Biometrics 11, 375–386 (1955).
Cochran, W. G. Some methods for strengthening the common X² tests. Biometrics 10, 417–451 (1954).
Bellera, C. A. & Hanley, J. A. A method is presented to plan the required sample size when estimating regression-based reference limits. J. Clin. Epidemiol. 60, 610–615 (2007).
Wickremasinghe, A. C., Kuzniewicz, M. W., McCulloch, C. E. & Newman, T. B. Efficacy of subthreshold newborn phototherapy during the birth hospitalization in preventing readmission for phototherapy. JAMA Pediatr. 172, 378–385 (2018).
Mreihil, K., Benth, J. S., Stensvold, H. J., Nakstad, B. & Hansen, T. W. R. Phototherapy is commonly used for neonatal jaundice but greater control is needed to avoid toxicity in the most vulnerable infants. Acta Paediatr. 107, 611–619 (2018).
IBM Corp. IBM Statistics for Macintosh, Version 27.0 (Released 2020).
Addinsoft. Xlstat. https://www.xlstat.com/en/ (2020).
Funding
This study was funded by Drager Medical Systems Inc., Germany and the University of Toronto Open Fellowship Award, Toronto, Canada.
Author information
Authors and Affiliations
Consortia
Contributions
T.J., J.G.R., and M.S. conceptualized the design of the study, drafted the initial manuscript, and revised and approved the final manuscript. C.D.G.K.-S., D.M.C., H.B., and R.Z.H. assisted in the design of the study, assisted with the analyses, and critically revised and approved the final manuscript. V.S. assisted in the design of the study, coordinated data collection, assisted with the analyses, and critically revised and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Patient consent was not required for this study since this study was a retrospective chart review.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Jegathesan, T., Ray, J.G., Keown-Stoneman, C.D.G. et al. Pre-phototherapy total serum bilirubin levels in extremely preterm infants. Pediatr Res 93, 226–232 (2023). https://doi.org/10.1038/s41390-022-02065-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02065-0