Abstract
Background
Preterm children are at higher risk of developing mental health problems than full-term children. Deterioration of children’s mental health was observed during COVID-19 pandemic restrictive measures. Our study compared emotional and attention-deficit/hyperactivity disorder (ADHD) symptoms during school closure between preterm and full-term children.
Methods
Data from two French birth cohorts—ELFE and EPIPAGE-2—were used. In 2011, infants born ≥22 weeks’ gestation were recruited. Parents completed the Strengths and Difficulties Questionnaire when the children were 9 years old and experiencing school closure. Multivariate multinomial logistic regression models were used.
Results
Subjects included 4164 full-term and 1119 preterm children. In univariate analyses, compared to full-term children: extremely and very preterm children more frequently had abnormal and borderline ADHD scores (odds ratio [OR] 1.86, 95% confidence interval [CI] 1.50–2.30, OR 1.42, 95% CI 1.08–1.85, respectively) and abnormal emotional scores (OR 1.86, 95% CI 1.43–2.40); moderate to late preterm children more often had abnormal ADHD scores (OR 1.33, 95% CI 1.01–1.78). The associations did not remain when previous symptoms at 5 years old were considered.
Conclusions
School closure during lockdown did not appear to increase the risk of mental health problems in preterm compared to full-term children.
Impact statement
-
Preterm children are at higher risk of developing mental health problems than full-term children. Deterioration in children’s mental health was observed during COVID-19 pandemic restrictions. However, whether preterm children were a particularly vulnerable subgroup during school closure is unclear.
-
In univariate analyses, extremely and very preterm children more often had abnormal and borderline ADHD symptoms and abnormal emotional symptom scores than full-term children. The associations did not remain significantly associated when previous symptoms were considered.
-
Preterm compared to full-term children more often suffer from ADHD and emotional symptoms, but school closure during lockdown did not appear to increase this risk.
Similar content being viewed by others
Introduction
Children born preterm are at higher risk of developing mental health problems than full-term children1, particularly attention-deficit/hyperactivity disorder (ADHD), mood disorders, anxiety, and behavioral problems1,2. These risks are significant for extremely preterm children (i.e., those born at <33 weeks’ gestation)3. Note that weight at birth plays a role independent of gestational age1.
The worldwide COVID-19 pandemic led to exceptional public health measures, including lockdowns and school closings. Several studies have assessed children’s mental health during lockdowns4. Home quarantine and the closing of educational institutions lead to isolation, limitations on outdoor and physical activities, and problems meeting friends. Loneliness and limited social relationships are associated with more significant mental health difficulties in adolescents during lockdowns and school closings4,5. All around the world, children’s mental health problems increased during lockdown6,7. Anxiety and depression were the most commonly observed problems, particularly among adolescents and girls7. Oppositional-defiant behaviors, ADHD, and sleep disorders were also noticed6,8. Existing emotional or ADHD symptoms at the beginning of lockdown appeared to predict deterioration in symptoms4.
Most of the available research on children’s mental health during COVID-19 school closures relies on population-based samples, and very few studies have focused on children born preterm. One study conducted in Switzerland with 54 very preterm children found no increase in the severity of the pandemic’s impact on well-being compared to 73 typically developing children9. However, the study was limited by the small sample size. The question remains whether premature children were particularly vulnerable to the effects of school closure during COVID. Here we compared 9-years-old preterm and full-term French children in terms of emotional and ADHD symptoms during school closures related to the first lockdown.
Methods
Setting and study design
In the context of the SARS-COV2 pandemic, the Santé, Pratiques, Relations et Inégalités Sociales en population générale pendant la crise COVID-19 (SAPRIS) survey was implemented in mid-March 2020 to evaluate the main challenges of the pandemic in France10. Several French population-based cohorts participated, including two national birth cohorts: ELFE and EPIPAGE-2. Participation in the SAPRIS survey was only offered to families with whom contact by email was possible because the survey relied on Web-based questionnaires.
Sample
In 2011, 344 randomly selected private and public maternity units in metropolitan France participated in the ELFE cohort11. Children with parents who were minors or who were not able to give their consent were excluded; Children were also excluded if their mother did not read French, Arabic, Turkish, or English; in cases of multiple pregnancies (≥3) or birth at <33 weeks’ of gestation; and if the family planned to move out of metropolitan France in the next 3 years.
In the EPIPAGE-2 cohort, all infants born after the completion of 22–34 weeks of amenorrhea were eligible for inclusion. The beginning date for inclusion was in March 2011, and all maternity units in 25 French regions participated. The recruitment period was 8 months for infants born at 22–26 weeks, 6 months for those born at 27–31 weeks and 5 weeks for those born at 32–34 weeks.
Outcome
Parents completed two subscales of the French version of the Strengths and Difficulties Questionnaire (SDQ) when the child was 9 years old, during the first French lockdown (from April 16 to May 4, 2020) or immediately thereafter (May 5–June 21, 2020), thus encompassing the whole period of continuous school closure. The first strict French lockdown for the COVID-19 pandemic occurred from March 17 to May 11, 2020. The SDQ is a brief behavioral questionnaire containing 25 questions divided among five subscales12. Parents completed the subscales addressing emotional symptoms (“Often complains of headaches, stomach-aches or sickness”, “Many worries or often seems worried”, “Often unhappy, depressed or tearful”, “Nervous or clingy in new situations, easily loses confidence”, “Many fears, easily scared”) and hyperactivity/inattention (“Restless, overactive, cannot stay still for long”, “Constantly fidgeting or squirming”, “Easily distracted, concentration wanders”, “Thinks things out before acting” [reverse score], “Good attention span, sees work through to the end” [reverse score]). Scores on the two scales range from 0 (no symptoms) to 10 (the most symptoms). On the emotional problems scale, 4 is considered a borderline state and ≥5 abnormal. On the hyperactivity scale, 6 is considered borderline and ≥7 abnormal. The questionnaire has been validated in several languages, including French12,13.
Main exposure
Preterm children were children born alive before 37 weeks of amenorrhea. We distinguished three categories based on gestational age: extremely and very preterm (<32 weeks), moderate to late preterm (32–36 weeks + 6 days), and full-term (≥37 weeks).
Covariates
To choose appropriate covariates, we reviewed factors associated with emotional or ADHD symptoms in childhood and those reported during the the lockdown. Female sex increases the risk for emotional symptoms14, whereas boys are reportedly at greater risk for ADHD symptoms14. Family financial difficulties have been associated with poor mental health, that is, emotional symptoms, suicide attempts, ADHD symptoms, and anxiety8,15. Furthermore, adults with less education and those young in age were at greater risk for anxiety and depression during lockdown16, and parents’ mental health can reportedly influence children’s well-being6,8. Low birth weight is associated with a risk of developing ADHD17. Finally, preexisting mental health problems increase the risk of having these symptoms again18. Therefore, we chose as covariates maternal age at the child’s birth, low weight at birth (defined as birth weight below the 10th percentile for gestational age), child sex, previous parental ratings on the two SDQ subscales at 5 years old, and maternal education and household income when the child was 1 year old. We used standardized French intrauterine growth curves to determine intrauterine growth restrictions19.
Ethics
Ethical approval and written informed consent were obtained from each participant before enrolment in the original cohort. Regulatory authorities that oversee ethical data collection in France approved the ELFE and EPIPAGE-2 studies: Comité de Protection des Personnes (CPP no. IDFIX-11-024, CPP SC-2873, respectively); Comité National Informatique et Libertés (CNIL no. 910504, CNIL no. 91009); and CNIS no. 2011X716AU for ELFE, CCTIRS no. 10.626 for EPIPAGE-2. According to French law, specific additional written consent was not required for the present nested survey. The Inserm ethics evaluation committee approved the SAPRIS survey (approval #20-672 dated March 30, 2020).
Statistical analyses
Children’s characteristics were described, and the characteristics of children included in the study were compared to those of children lost to follow-up with chi-square tests.
We used classification and regression tree methods to handle missing data20. These methods are attractive for imputation because they are robust against outliers, can be applied to mixed data (both continuous and categorical), and can handle multicollinearity21. In addition, we tested the association between prematurity and the child’s mental health using unadjusted and adjusted multinomial logistic regression to estimate odds ratios (ORs) and 95% confidence intervals (CIs). Estimates were adjusted based on maternal age at the child’s birth, low weight at birth, child sex, previous parental assessments of hyperactivity/inattention and emotional symptoms in the child at 5 years old, and maternal education and monthly household income when the child was 1 year old.
For sensitivity analyses, we conducted these same multinomial logistic regression analyses on a larger sample (n = 5564). Instead of including only individuals with hyperactivity/inattention and emotional disturbances at both 5 and 9 years (n = 5283), we examined individuals with these problems at age 9 and imputed scores for missing data at age 5.
Results
Description of the population
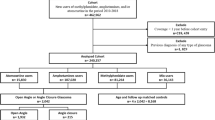
Figure 1 shows participation in the study from birth to the 9-year follow-up, which included 5283 children. Children with incomplete data, that is, without ADHD and emotional symptom assessments at 9 and/or 5 years old, were more frequently full term (92.5% vs. 78.8%, p < 0.05) and small for gestational age (89.0% vs. 87.2%, p < 0.05) compared to the 5283 included children with ADHD and emotional symptom data at both time points. They more frequently had borderline scores for hyperactivity/inattention symptoms at 5 years old (11.1% vs. 8.2%, p < 0.05). They were also more likely to have mothers with less education (46.5% vs. 22.1%, p < 0.05) and who were young (<25 years) at their birth (16.0% vs. 5.3%, p < 0.05). Finally, this group had a lower household income when the child was 1 year old (56.0% vs. 71.9% with monthly income ≥3000 euros, p < 0.05). The children’s characteristics are described in Table 1.
When schools were closed, 701 (13.3%) and 411 (7.8%) children, respectively, had abnormal scores for ADHD and emotional symptoms, and 475 (9.0%) and 295 (5.6%) children, respectively, had borderline scores for ADHD and emotional symptoms. Table 2 shows the ADHD and emotional symptom scores at 5 and 9 years old among preterm and full-term children. Supplemental Tables S1 and S2 show changes in these scores between ages 5 and 9.
Association with hyperactivity/inattention symptoms during school closure
In univariate analyses, compared to full-term children, extremely and very preterm children more often showed abnormal (OR 1.86, 95% CI 1.50–2.30) or borderline (OR 1.42, 95% CI 1.08–1.85) ADHD symptom scores. Moderate to late preterm children showed an increased risk for abnormal ADHD symptom scores (OR 1.33, 95% CI 1.01–1.78; Table 3).
However, these differences were not found after adjustment for covariates. In multivariate analyses, boys were more likely than girls to have high (OR 1.91, 95% CI 1.61–2.28) or intermediate (OR 1.55, 95% CI 1.28–1.89) ADHD symptom scores. Children with abnormal or borderline ADHD symptom scores before the pandemic were more likely than children with scores in the normal range to have abnormal (OR 5.18, 95% CI 4.12–6.51 and OR 3.55, 95% CI 2.76–4.55) or borderline (OR 2.96, 95% CI 2.22–3.94 and OR 2.20, 95% CI 1.61–3.00) scores on the present measurement. Similarly, compared to children with normal emotional symptom scores at 5 years of age, children with abnormal emotional symptom scores at 5 years more often had abnormal (OR 1.59, 95% CI 1.26–2.01) or borderline (OR 1.42, 95% CI 1.08–1.86) ADHD symptoms.
Children whose mothers were 40 years or older at their birth were more likely than children whose mothers were younger to display abnormal ADHD symptoms (ORs for age categories from youngest to oldest: 0.54, 0.46, 0.57, 0.65).
Association with emotional symptoms during school closure
In univariate analyses, compared to full-term children, extremely and very preterm children more frequently exhibited abnormal emotional symptoms (OR 1.86, 95% CI 1.43–2.40). No significant differences were observed between moderate to late preterm and full-term children (Table 4).
Multivariate analyses revealed no significant differences between full-term and preterm children after adjustment for covariates. Boys were less likely than girls to have abnormal (OR 0.80, 95% CI 0.65–0.99) or borderline (OR 0.68, 95% CI 0.53–0.87) emotional symptom scores. Children with previous abnormal or borderline emotional symptoms were more likely than those with previously normal scores to have abnormal (OR 3.67, 95% CI 2.86–4.69 and OR 2.40, 95% CI 1.76–3.27) or borderline (OR 2.29, 95% CI 1.69–3.12 and OR 1.70, 95% CI 1.17–2.47) emotional symptom scores.
Similarly, children with previous abnormal ADHD symptom scores were more likely than children with previously normal scores to have abnormal (OR 1.50, 95% CI 1.10–2.03) or borderline (OR 1.78, 95% CI 1.24–2.56) emotional symptom scores. Finally, children whose mothers were 40 years or older at their birth were more likely than children whose mothers were 25–34 years old to display abnormal emotional symptoms.
Sensitivity analyses
When we performed sensitivity analyses and imputed the data in the presence of missing data for scores measured at age 5, the results were similar, with no difference between preterm and full-term children in multivariate analyses.
Discussion
To the best of our knowledge, this is the first study to report emotional and ADHD symptoms among preterm children during school closures caused by the COVID-19 pandemic and to compare these results to those for full-term children in a large epidemiological sample. Although extremely and very preterm children more often had abnormal ADHD scores during school closure compared to full-term children, the association did not remain when previous symptoms were considered. These results suggest that prematurity is a risk factor for mental health problems but school closure during lockdown did not confer an increased risk of mental health in preterm children compared to full-term children. It is interesting that preexisting mental health problems were associated with a greater risk for symptoms during school closure.
These results are in accordance with the results of other available studies. We found only one study in which child well-being before and during the lockdown was compared across three groups of children: 54 children born very preterm, 73 children with congenital heart disease, and 73 typically developing children9. Children’s psychological well-being decreased significantly during the pandemic but without differences among the three groups. Previous studies on ADHD symptoms conducted outside the COVID-19 pandemic have shown that preterm children are at greater risk for ADHD symptoms from the first years of life, but there does not seem to be any further deterioration in this group over time compared to full-term children2,22,23,24. An Australian study comparing attention profiles at 7 and 13 years between children born before 30 weeks’ gestation and those born full term showed that the very preterm children were at greater risk of developing stable low attention or improving attention patterns, but they did not differ in patterns of declining attention2. Likewise, in another study Breeman et al. showed that very preterm children (<32 weeks) had an increased risk for attention problems in childhood and adulthood22. However, the trajectories of attention development were similar between very preterm and full-term children between 6 and 8 years old22. A study conducted in the United Kingdom and the Republic of Ireland comparing extremely preterm (<26 weeks) and full-term children also showed that extremely preterm children had a greater risk of developing ADHD and emotional symptoms at 6, 11, 16, and 19 years of age. However, ADHD symptoms decreased slightly over time, and the difference declined23. By contrast, with respect to emotional symptoms, the difference and thus the risk increased over time23. However, the results of relevant studies of emotional symptoms before the COVID-19 pandemic are inconsistent. In a Bavarian cohort of very preterm and/or very low-birth-weight children, very preterm children (<32 weeks) were more at risk for emotional problems, with relative stability between 6 and 8.5 years old25.
It is not surprising that in our study, preexisting conditions were particularly associated with the presence of symptoms during school closure. Some studies focusing specifically on the impact of the pandemic on children with ADHD suggest an increase in ADHD symptoms, sometimes with a resultant deterioration in family relationships26. However, children with ADHD have also a significantly higher risk of developing major depressive disorder27.
Within the context of the wider literature, the present results suggest that childhood may not have been the most at-risk age period during the first lockdown. Indeed, a systematic review and meta-analysis of 23 studies assessing the mental health of children and adolescents during the active phase of the COVID-19 pandemic from 2019 to 2020 revealed that adolescents exhibited a higher prevalence of depression than children7. Compared to childhood, adolescence is also a higher risk life period for suicidal ideation or suicide attempts independent of the COVID-19 pandemic28. Assessing the mental health trajectories of preterm adolescents to determine any age effects would be particularly relevant.
Children of older mothers in the present study were more likely to have ADHD symptoms, contrary to what has been reported in the literature29. The same observation was made for emotional symptoms. In a recent study, both younger and older maternal age were linked to depression in offspring30. Older mothers may have been less tolerant or more aware of their child’s symptoms and thus reported them more. Uncontrolled environmental confounding factors could also be involved.
This study has several limitations. First, our primary outcome was measured only once during the pandemic. Measuring ADHD and emotional symptoms just before the beginning of the lockdown and again afterward would have enabled us to better assess the effects of lockdown and school closure on mental health. Second, the SDQ subscale scores were calculated from only parents’ answers, which could have led to measurement bias. The number of children with incomplete data is also important, as it could be related to selection bias. Children with incomplete data were more often male. This could have led to an overestimation of emotional symptoms, as female sex has been associated with depression in several studies14. Children with mothers who were young and who had less education more often had incomplete data. This could have resulted in an underestimation of the number of children with emotional and ADHD symptoms, because adults with less education and younger age were themselves more at risk for anxiety and depression during lockdown, and children’s well-being is associated with parental mental health16. Nonresponders more often reported lower socioeconomic status. However, analyses of the potential association between prematurity and emotional and ADHD symptoms during school closure were adjusted for these variables in children and their families. Hence, these differences should not have affected the comparison of pre- and full-term children. Children with complete data more often had normal ADHD symptom scores at 5 years of age. This could have resulted in an underestimation of the number of children with ADHD symptoms during school closure, because previously existing symptoms were associated with the presence of symptoms during school closure. Finally, our results were for a French sample, and their generalizability may thus be limited to countries with similar characteristics in terms of the health care system and insurance coverage. In the French health care system, premature children benefit from long-term medical and psychological follow-up, which may have helped to reduce the impact of the COVID crisis on their well-being.
Conclusion
Our study suggests that, in the context of the COVID crisis, school closure during the lockdown did not confer an increased risk of mental health problems in preterm children compared to full-term children. It will be important to follow premature children over the long term to fully appreciate the enduring or cumulative effects of the COVID crisis.
Data availability
In regards to data availability, data of the study are protected under the protection of health data regulation set by the French National Commission on Informatics and Liberty (Commission Nationale de l’Informatique et des Libertés, CNIL). The data can be available upon reasonable request after a consultation with the steering com- mittee of the Sapris study. The French law forbids us to provide free access to Sapris data; access could however be given by the steering committee after legal verification of the use of the data.
References
Hee Chung, E., Chou, J. & Brown, K. A. Neurodevelopmental outcomes of preterm infants: a recent literature review. Transl. Pediatr. 9, S3–S8 (2020).
Bogičević, L. et al. Individual attention patterns in children born very preterm and full term at 7 and 13 years of age. J. Int. Neuropsychol. Soc. 1–11 https://doi.org/10.1017/S1355617720001411 (2021).
Cronin, F. M., Segurado, R., McAuliffe, F. M., Kelleher, C. C. & Tremblay, R. E. Gestational age at birth and “body-mind” health at 5 years of age: a Population Based Cohort Study. PLoS ONE 11, e0151222 (2016).
Cooper, K. et al. Loneliness, social relationships, and mental health in adolescents during the COVID-19 pandemic. J. Affect. Disord. 289, 98–104 (2021).
Liu, J. J., Bao, Y., Huang, X., Shi, J. & Lu, L. Mental health considerations for children quarantined because of COVID-19. Lancet Child Adolesc. Health 4, 347–349 (2020).
Schmidt, S. J., Barblan, L. P., Lory, I. & Landolt, M. A. Age-related effects of the COVID-19 pandemic on mental health of children and adolescents. Eur. J. Psychotraumatol. 12, 1901407 (2021).
Ma, L. et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 293, 78–89 (2021).
Moulin, F. et al. Risk and protective factors related to children’s symptoms of emotional difficulties and hyperactivity/inattention during the COVID-19-related lockdown in France: results from a community sample. Eur. Child Adolesc. Psychiatry https://doi.org/10.1007/s00787-021-01752-3 (2021).
Ehrler, M. et al. Impact of the COVID-19 pandemic on children with and without risk for neurodevelopmental impairments. Acta Paediatr. 110, 1281–1288 (2021).
Carrat, F. et al. Incidence and risk factors of COVID-19-like symptoms in the French general population during the lockdown period: a multi-cohort study. BMC Infect. Dis. 21, 169 (2021).
Charles, M. A. et al. Cohort Profile: The French national cohort of children (ELFE): birth to 5 years. Int. J. Epidemiol. 49, 368–369j (2020).
Goodman, R. Psychometric properties of the strengths and difficulties questionnaire. J. Am. Acad. Child Adolesc. Psychiatry 40, 1337–1345 (2021).
d’Acremont, M. & Linden, M. Vder Confirmatory factor analysis of the Strengths and Difficulties Questionnaire in a community sample of French-speaking adolescents. Eur. J. Psychol. Assess. 24, 1–8 (2008).
Ramirez, S. et al. Brief Research Report: the association between educational experiences and Covid-19 pandemic-related variables, and mental health among children and adolescents. Front. Psychiatry 12, 647456 (2021).
Navarro, M. C. et al. Machine learning assessment of early life factors predicting suicide attempt in adolescence or young adulthood. JAMA Netw. Open 4, e211450 (2021).
Fancourt, D., Steptoe, A. & Bu, F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry 8, 141–149 (2021).
Perapoch, J. et al. Prematurity and ADHD in childhood: an observational register-based study in Catalonia. J. Atten. Disord. 25, 933–941 (2021).
Panchal, U. et al. The impact of COVID-19 lockdown on child and adolescent mental health: systematic review. Eur. Child Adolesc. Psychiatry https://doi.org/10.1007/s00787-021-01856-w (2021).
Ego, A. et al. Customized and non-customized French intrauterine growth curves. I-Methodology. J. Gynecol. Obstet. Biol. Reprod. 45, 155–164 (2016).
Burgette, L. F. & Reiter, J. P. Multiple imputation for missing data via sequential regression trees. Am. J. Epidemiol. 72, 1070–1076 (2010).
Buuren, S. V. Flexible Imputation of Missing Data 2nd edn. 444 (CRC Press, Boca Raton, FL, 2018).
Breeman, L. D., Jaekel, J., Baumann, N., Bartmann, P. & Wolke, D. Attention problems in very preterm children from childhood to adulthood: the Bavarian Longitudinal Study. J. Child Psychol. Psychiatry 57, 132–140 (2016).
Linsell, L. et al. Trajectories of behavior, attention, social and emotional problems from childhood to early adulthood following extremely preterm birth: a prospective cohort study. Eur. Child Adolesc. Psychiatry 28, 531–542 (2019).
Yates, R. et al. Rates and stability of mental health disorders in children born very preterm at 7 and 13 years. Pediatrics 145, e20192699 (2020).
Hall, J. & Wolke, D. A comparison of prematurity and small for gestational age as risk factors for age 6–13 year emotional problems. Early Hum. Dev. 88, 797–804 (2012).
Shah, R., Raju, V. V., Sharma, A. & Grover, S. Impact of COVID-19 and lockdown on children with ADHD and their families—an online survey and a continuity care model. J. Neurosci. Rural Pract. 12, 71–79 (2021).
Chronis-Tuscano, A. et al. Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Arch. Gen. Psychiatry 67, 1044–1051 (2010).
Geoffroy, M. C., Orri, M., Girard, A., Perret, L. C., Turecki, G. Trajectories of suicide attempts from early adolescence to emerging adulthood: prospective 11-year follow-up of a Canadian cohort. Psychol. Med. 1–11. https://doi.org/10.1017/S0033291720000732 (2020).
Hvolgaard Mikkelsen, S., Olsen, J., Bech, B. H. & Obel, C. Parental age and attention-deficit/hyperactivity disorder (ADHD). Int. J. Epidemiol. 46, 409–420 (2017).
Filatova, S., Upadhyaya, S., Luntamo, T., Sourander, A. & Chudal, R. Parental age and risk of depression: a nationwide, population-based case-control study. J. Affect. Disord. 282, 322–328 (2021).
Acknowledgements
Agence Nationale de la Recherche (ANR, 0009/SAPRIS/997/NB), Fondation pour la Recherche Médicale, Direction Générale de la Recherche et de l’Innovation, Institut Gustave Roussy, the New-Aquitaine region.
Author information
Authors and Affiliations
Consortia
Contributions
M.B. concept and design the study, interpreted the data and wrote the manuscript. M.M. did the statistical analysis, interpreted the data and revised the manuscript. F.M., X.T., S.V., S.M.C., B.F., T.S., B.G., L.M., M.N.D., M.A.C., P.Y.A., M.M., A.R., interpreted the data, critiqued the manuscript of important intellectual content and approved the final version of manuscript. C.G. concept and design the study, interpreted the data, and revised the manuscript. The SAPRIS group enrolled participants, collected the data, and revised the manuscript. Authors had access to all the data in the study and participated in the decision to submit.
Corresponding author
Ethics declarations
Competing interests
M.M. has been funded by the New-Aquitaine region (AMI Flash Recherche et Innovations COVID). The other authors have no competing interests to declare.
Consent statement
A consent form was signed by parents for inclusion.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bailhache, M., Monnier, M., Moulin, F. et al. Emotional and attention-deficit/hyperactivity disorder symptoms of preterm vs. full-term children during COVID-19 pandemic restrictions. Pediatr Res 92, 1749–1756 (2022). https://doi.org/10.1038/s41390-022-02037-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02037-4
This article is cited by
-
The impact of COVID-19 lockdowns on mental health patient populations in the United States
Scientific Reports (2024)