Abstract
Background
Dysnatremias are frequent in acute gastroenteritis. High outdoor temperatures have been associated with hyponatremia in both adults and the elderly, but no data are available among children with gastroenteritis.
Methods
Children <10 years of age admitted to the emergency department of the Policlinico Hospital, Milan (Italy) between 2009 and 2019 with acute moderate-severe gastroenteritis were enrolled. The association between hyponatremia (sodium < 135 mmol/L) and daily mean levels of temperature or apparent temperature from day of admission up to 14 days before was analyzed by multivariable logistic regression models.
Results
In 202 included children (46% females), we observed an increased risk of hyponatremia per unit increase in outdoor temperature of the sixth, eighth and ninth day before admission [Odds Ratio = 1.24 (95% Confidence Interval: 1.04–1.47), 1.14 (1.01–1.28), and 1.14 (1.01–1.28), respectively]. Analyses considering average temperature levels of the ten days preceding admission returned similar findings as well as those on apparent temperature.
Conclusions
Our data suggest the existence of an association between outdoor temperature and circulating sodium levels in children with acute gastroenteritis. The role of meteorological conditions on electrolyte imbalance should be further explored in the context of climate change.
Impact
-
The role of meteorological variables in the development of dysnatremias has been demonstrated in children and adolescents with cystic fibrosis.
-
This study shows for the first time that higher outdoor temperatures are associated with a higher risk of hyponatremia in children with gastroenteritis.
-
In the context of climate change, the role of external climate conditions on the risk of electrolyte imbalance in children should be more and more considered and explored in future studies.
Similar content being viewed by others
Introduction
Abnormalities in blood sodium are associated with an increased risk of morbidity and mortality in patients requiring emergency care.1,2 In children with acute gastroenteritis, a major cause of children emergency visits, dysnatremias are observed in one every two cases.3 Clinical manifestations might range from mild to life-threatening conditions.4
Reports in adults have suggested that the frequency of hyponatremia has seasonal fluctuations.5 In particular, high outdoor temperatures have been associated with a tendency towards low levels of circulating sodium in both adults and the elderly.6 Similar data were observed in children and adolescents affected with cystic fibrosis.7 However, no data are available on the association between climate conditions and sodium levels in children without any chronic disease.
The aim of this study was to investigate the association between some meteorological variables and circulating sodium levels in otherwise healthy children admitted to the emergency department (ED) for acute gastroenteritis.
Methods
An observational study was conducted between December 2009 and December 2019 at the Pediatric ED of the Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, Italy. Eligible subjects were children <10 years of age admitted to the Pediatric ED with acute moderate–severe gastroenteritis3 and living in the municipality of Milan (the capital city of Lombardy). Subjects without sodium level assessment, hemodynamically unstable, with chronic kidney diseases, or with concurrent medication potentially affecting sodium levels (e.g., diuretics) were excluded.
For all study subjects, the following data were extracted from online medical records: age, sex, body weight, maximum body temperature), days of disease before admission (comprising fever, vomiting, or diarrhea), fluid and food intake in the 24 h before admission, place of residence, and values of circulating sodium at admission (analyzed by direct potentiometry). According to sodium levels, subjects were classified as hyponatremic (sodium <135 mmol/L) or normonatremic (sodium ≥135 mmol/L). The existence of clinical features consistent with acute dysnatremic brain damage such as obtundation, coma, or seizures was also addressed.
Data on outdoor temperature and humidity were obtained from the network of meteorological monitoring stations of the environmental protection agency of the Lombardy region (ARPA Lombardia). Humidity was used to estimate apparent temperature, i.e., the perceived temperature equivalent that includes both outdoor temperature and humidity as the summary meteorological variable.8 Each subject was assigned the daily mean levels of temperature and apparent temperature of the city of Milan, available from December 1, 2009 to December 31, 2019. To analyze their short-term influence on sodium levels at ED admission, different time windows were investigated: (i) daily lags, obtained considering average daily levels of (apparent) temperature from the day of admission (lag 0) up to 14 days before (lag 14); (ii) averaged daily lags, obtained by averaging levels of (apparent) temperature of the day of admission with the levels of the day before (lag 0–1) and of each preceding day up to 14 days before (lag 0–14). All data were retrospectively collected and anonymized.
Data analysis and statistics
Data were summarized using medians, interquartile ranges (IQRs), and proportions. Differences in the distribution of the main characteristics of our study population across categories of sodium levels (i.e., hyponatremic vs. normonatremic) were assessed using the χ2 test for categorical variables and Kruskal–Wallis test for continuous variables. To assess the association between meteorological variables and the risk of being hyponatremic, we performed logistic regression models with increasing levels of adjustment: (a) minimally adjusted models included only year and month of admission; (b) medium adjusted models included (a) + age, sex, and body weight; (c) fully adjusted models included (b) + days of diseases before admission (1, 2, 3, 4, 5+), maximum body temperature (≤37, 37.1–38.0, 38.1–38.5, 38.6–39.0, ≥39.1 °C), food and fluid intake reduction before admission (severely reduced, moderately reduced, or mildly reduced/normal).9
Models were applied to each (averaged) daily lag, with lag terms modeled one at a time. As a sensitivity analysis, single lag terms were entered simultaneously in a single model to allow for mutual adjustment of the lag effects, thus fitting unconstrained distributed lag models.10 Results were expressed as odds ratios (ORs) and corresponding 95% confidence intervals (95% CIs) per unit increase in (apparent) temperature.
Results
A total of 202 children (females = 93, 46%) were included (Table 1). Their median age was 1.2 [IQR: 0.9–1.8] years and median circulating sodium level was 134 [132–137] mmol/L. One hundred and three (51%) children were hyponatremic. Among children with hyponatremia, age was slightly higher (1.4 vs. 1.2 years, p = 0.004) and females represented a higher, although not significant, proportion (51.5 vs. 40.8, p = 0.127). No other characteristic of the study population (i.e., body weight, days of disease before admission, maximum body temperature, and food and fluid intake in the 24 h before admission) significantly differed between the two study groups. Median outdoor temperature at the day of admission was 10.7 [5.9–16.1] °C, while median levels of apparent temperature were slightly lower 8.6 [3.5–15.0]. None of the investigated meteorological variables significantly differed between hyponatremic and normonatremic children in univariate analyses.
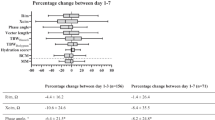
In fully adjusted models, we observed a significant association between outdoor temperature in the sixth, eighth and ninth day before ED admission (lags 6, 8, and 9) and the risk of being hyponatremic on admission, with ORs = 1.24 (95% CI: 1.04–1.47), 1.14 (95% CI: 1.01–1.28), and 1.14 (95% CI: 1.01–1.28), respectively (Fig. 1a and Supplementary Table 1). Very similar findings were observed for apparent temperature (Supplementary Table 1). Results on the effect of temperature at lag 6 were confirmed also when all lag terms were modeled together (OR: 1.78, 95% CI: 1.13–2.81). Analyses considering cumulative daily lags showed a ≈25% significantly higher risk of being hyponatremic for increasing temperature levels from lag 0–7 (OR: 1.24, 95% CI: 1.00–1.53) to lag 0–10 (OR: 1.26, 95% CI: 1.01–1.57) (Fig. 1b and Supplementary Table 2). Again, results on apparent temperature mostly overlapped (Supplementary Table 2). Minimally and medium adjusted analyses returned substantially comparable results (data not shown).
Results are expressed as odds ratios (ORs) and corresponding 95% confidence intervals (95% CIs) per unit increase in levels of temperature (°C) occurring daily from the day of admission (lag 0) up to 14 days before (lag 14) (a) or obtained by averaging the levels of the day of admission with the levels of the day before (lags 0–1) and of each preceding day up to 14 days before (lag 0–14) (b).
Discussion
This study shows for the first time that increasing outdoor temperature levels in the few days preceding the onset of acute gastroenteritis are associated with an augmented risk of hyponatremia in children. Analogous findings were also observed for apparent outdoor temperature.
The association between outdoor temperature and the risk of hyponatremia is in line with previous, recent studies on adults and the elderly. Higher outdoor temperature was found to be associated with sodium levels below 125 mmol/L in adult subjects admitted to the ED in Switzerland.6 Two further studies conducted in ED confirmed that warmer and colder seasons were positively and negatively associated with the risk of hyponatremia, respectively.11,12
Data on apparent outdoor temperature had a similar direction to those on outdoor temperature. A previous study conducted in adults in the ED found that an increase in outdoor temperature or in apparent outdoor temperature had a similar negative effect on fluids and electrolyte imbalance.13 In addition, a metanalysis on the elderly, found a similar negative effect of apparent temperature and outdoor temperature on the risk of mortality.14 These findings appear more and more important in the context of the climate change that is currently observed worldwide. Until the 1980s, hypernatremia and normonatremia were common and hyponatremia rare in childhood acute gastroenteritis. In the following decades, hypernatremia almost disappeared while the prevalence of hyponatremia increased. It is assumed that the resurgence of breastfeeding, formulas having less salt, and the present attitude toward gastroenteritis, with early and fast reintroduction of mostly hypotonic fluids, account for this shift.3 Our data suggest that climate change could also be a contributing factor.
Although the findings of our study are consistent with those in adults and the elderly, concurrent risk factors for hyponatremia are likely to be different in childhood. Differently from adults, none of the included children was on treatment with diuretics or reported pre-existing chronic kidney diseases. On the other hand, nausea, and lack of appetite due to elevated ketone bodies and stimuli by gut mucosa damage, are frequently observed in children with gastroenteritis.15 These conditions, associated with higher sweating, a reduced salt intake, and increased ingestion of free water or other hypotonic fluids, which typically occurs with higher temperatures,16,17,18 might concur with the development of hyponatremia in pediatric patients with gastroenteritis.4
Our study suggests a peculiar role of outdoor temperatures 6–10 days before sodium level testing on the risk of hyponatremia. In the attempt to interpret our finding, we can surmise that parents keep a child with the onset of vomiting, diarrhea, and fever resting at home with a more controlled indoor temperature. As a consequence, we can speculate that external climate conditions might have had a limited impact after the appearance of the first symptoms. On the other hand, the higher external temperature in the days before symptoms’ onset might have predisposed the child to develop hyponatremia. This hypothesis is supported by the finding that most (>90%) children presented symptoms in the 5 days preceding sodium testing, by the sensitivity analyses, and by the models investigating the cumulative daily lags in the days preceding the onset of symptoms. Future studies should confirm this speculation.
This study has limitations. First, it is a single-center, retrospective study. Second, we could not obtain data on the indoor environment before admission to the ED. Third, the sample size is limited. Fourth, missing data in some of the variables we adjusted for might have, at least partly, influenced our findings, even though our results appeared consistent across increasing levels of adjustment. On the other hand, our work has also some important strengths: differently from other previous studies in adults,5,12 we considered daily climate conditions rather than seasonality as exposure of interest. Furthermore, sodium was measured by direct potentiometry, as recommended by international authorities, because spuriously normal or spuriously altered sodium values are not observed with this laboratory technique.19,20 The major strength of the study lies in it being the first to evaluate the interplay between outdoor temperature and the tendency to hyponatremia metabolism in acute childhood gastroenteritis.
In conclusion, our data indicate a possible association between meteorological variables and circulating sodium levels in otherwise healthy children admitted to the ED for acute gastroenteritis. Considering the impact of climate change and, in particular, the increasing global warming, the role of external climate conditions on the risk of hyponatremia in children should be considered and explored in future studies.
References
Joergensen, D., Tazmini, K. & Jacobsen, D. Acute dysnatremias - a dangerous and overlooked clinical problem. Scand. J. Trauma Resusc. Emerg. Med. 27, 58 (2019).
Prasad, S. V., Singhi, S. & Chugh, K. S. Hyponatremia in sick children seeking pediatric emergency care. Indian Pediatr. 31, 287–294 (1994).
Mazzoni, M. B. et al. Hyponatremia in infants with community-acquired infections on hospital admission. PLoS ONE 14, e0219299 (2019).
Peruzzo, M. et al. Body fluids and salt metabolism - part II. Ital. J. Pediatr. 36, 78 (2010).
Imai, N., Osako, K., Kaneshiro, N. & Shibagaki, Y. Seasonal prevalence of hyponatremia in the emergency department: impact of age. BMC Emerg. Med. 18, 41 (2018).
Sailer, C. O. et al. Influence of outdoor temperature and relative humidity on incidence and etiology of hyponatremia. J. Clin. Endocrinol. Metab. 104, 1304–1312 (2019).
Scurati-Manzoni et al. Electrolyte abnormalities in cystic fibrosis: systematic review of the literature. Pediatr. Nephrol. 29, 1015–1023 (2014).
Analitis, A. et al. Effects of cold weather on mortality: results from 15 European cities within the PHEWE project. Am. J. Epidemiol. 168, 1397–1408 (2008).
Iglesia, I. et al. Total fluid intake of children and adolescents: cross-sectional surveys in 13 countries worldwide. Eur. J. Nutr. 54(Suppl 2), 57–67 (2015).
Bhaskaran, K., Gasparrini, A., Hajat, S., Smeeth, L. & Armstrong, B. Time series regression studies in environmental epidemiology. Int. J. Epidemiol. 42, 1187–1195 (2013).
Huwyler, T. et al. Profound hyponatraemia in the emergency department: seasonality and risk factors. Swiss Med. Wkly. 146, w14385 (2016).
Giordano, M. et al. Seasonal variations of hyponatremia in the emergency department: age-related changes. Am. J. Emerg. Med. 35, 749–752 (2017).
Heidari, L. et al. Susceptibility to heat-related fluid and electrolyte imbalance emergency department visits in Atlanta, Georgia, USA. Int. J. Environ. Res. Public Health 13, 982 (2016).
Bunker, A. et al. Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine 6, 258–268 (2016).
Canziani, B. C. et al. Clinical practice: nausea and vomiting in acute gastroenteritis: physiopathology and management. Eur. J. Pediatr. 177, 1–5 (2018).
Peruzzo, M. et al. Body fluids and salt metabolism - part II. Ital. J. Pediatr. 36, 78 (2010).
Malisova, O., Bountziouka, V., Panagiotakos, D. Β, Zampelas, A. & Kapsokefalou, M. Evaluation of seasonality on total water intake, water loss and water balance in the general population in Greece. J. Hum. Nutr. Diet. 26(Suppl 1), 90–96 (2013).
Leshem, M. Salt appetite is not increased in summer heat. Appetite 108, 28–31 (2017).
Malandrini, S. et al. Which laboratory technique is used for the blood sodium analysis in clinical research? A systematic review. Clin. Chem. Lab. Med. 59, 1501–1506 (2021).
Lavagno, C. et al. Hyponatremia in children with acute respiratory infections: a reappraisal. Pediatr. Pulmonol. 52, 962–967 (2017).
Acknowledgements
We wish to thank Matteo Scortichini for his valuable contribution in reviewing the methods applied and suggesting improvements. The study was partially supported by a grant from the Italian Ministry of Health (Ricerca corrente 2020).
Author information
Authors and Affiliations
Contributions
All authors gave a substantial contribution to conception and design, acquisition of data, or analysis and interpretation of data, with M.C. and G.P.M. drafting the article. A.L., M.L.C., M.G.B., and C.A. critically revised the manuscript for important intellectual content; and all authors gave their final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
Informed consent to participate was not required for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Milani, G.P., Lo Leggio, A., Castellazzi, M.L. et al. Outdoor temperature and circulating sodium in children with acute gastroenteritis. Pediatr Res 92, 1270–1273 (2022). https://doi.org/10.1038/s41390-022-01947-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-01947-7