Abstract
Background
We hypothesized that children with congenital solitary functioning kidney (CSFK) present forms of congenital urinary tract anomalies (CUTA) with higher chance of spontaneous resolution compared with patients with two kidneys.
Methods
We retrospectively selected 75 consecutive children with CUTA of the CSFK and 75 matched patients with unilateral CUTA but without CSFK (controls) with prenatal suspicion of unilateral CUTA and early evaluation. We compared the spontaneous CUTA resolution and the prevalence of kidney injury between groups at last follow-up. Patients and controls were clustered under the categories of “severe” and “non-severe” CUTA.
Results
The mean age at first and last follow-up was 0.17 ± 0.07 and 8.5 ± 5.2 years. Compared with controls, patients with CSFK had lower prevalence of severe CUTA at first evaluation; lower prevalence of febrile urinary tract infections, need of surgical correction, and higher rate of spontaneous CUTA resolution during follow-up; and a similar prevalence of mild kidney injury at last follow-up. CSFK compared with controls presented higher cumulative proportion of spontaneous resolution from severe CUTA (100 vs 41.8%; p < 0.001) and from the single CUTA sub-categories (severe vesicoureteral reflux, non-obstructive hydronephrosis, and megaureter).
Conclusions
CSFK patients had lower prevalence of severe forms and better outcomes of their CUTA compared with controls.
Impact
-
One-third of patients with congenital solitary functioning kidney (CSFK) present congenital urinary tract anomalies (CUTA) and manifest poorer outcomes compared with CSFK without CUTA.
-
CSFK patients had lower prevalence of severe forms and better outcomes of their CUTA in spite of similar prevalence of kidney injury compared with controls.
-
This adds evidence about disturbed nephrogenesis in CSFK patients and emboldens conservative management of many of their non-obstructive CUTA.
Similar content being viewed by others
Introduction
Due to their related embryologic origin, more than one congenital anomaly of the kidney and urinary tract can be observed in the same patient.1,2,3,4 For example, renal parenchymal anomalies such as kidney hypo/dysplasia can occur together with anomalies of the collecting system such as vesicoureteral reflux (VUR).1
Approximately one in three of the patients with congenital solitary functioning kidney (CSFK) present ipsilateral (on the side of CSFK) congenital urinary tract anomalies (CUTA).5,6,7 They manifest poorer kidney outcomes compared with CSFK patients without CUTA.3,8,9,10
Following feelings drawn from our daily clinical practice, we hypothesized that patients with CSFK present forms of CUTA with higher chance of spontaneous resolution compared with patients with two kidneys and that the poorer outcomes of CSFK patients with CUTA compared with CSFK patients without CUTA are mostly linked to congenital nephron deficit associated with CSFK rather than with postnatal complications related to the anomalies of the urinary tract.
With the aim to validate our hypothesis and to draw both pathophysiological and clinical information, we compared, for the first time, the outcomes of patients with CUTA of a CSFK with those of subjects having two kidneys and unilateral CUTA.
Methods
We retrospectively selected all the patients with CUTA of CSFK (n = 75) (cases) and identified 75 controls with 2 kidneys and unilateral CUTA and matched for sex, age at first evaluation and last follow-up, as well as kind of CUTA, consecutively attending our Department from January 2000 to January 2020.
We selected the patients of the past 20 years to enrol subjects having undergone homogeneous clinical and surgical strategies of CUTA management under the guide of the senior Paediatric Nephrologist of our Department.
The study was approved by our Research Ethical Committee (approval no. 1375/2016). The informed consent was obtained before any procedure.
Inclusion criteria of CSFK patients
Inclusion criteria of the CSFK patients were: (i) ultrasound-based prenatal diagnostic suspicion; (ii) first evaluation between 1 and 3 months of life with postnatal confirmation of CUTA; (iii) having undergone cystourethrogram (males) or cystoscintigraphy (females).
Inclusion/matching criteria of controls
On the basis of CUTA presented by our CSFK population, we considered as eligible the controls affected by VUR, uretero-pelvic junction obstruction (UPJO), non-obstructive hydronephrosis, and megaureter diagnosed on the basis of a prenatal diagnostic suspicion. Because none of the patients with CSFK had posterior urethral valves, controls with this anomaly were not considered eligible.
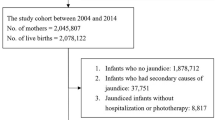
In case of more than one control matchable for each subject with CSFK, being our hypothesis that patients with CUTA of CSFK have milder form of CUTA compared with controls, we selected the patient with the mildest CUTA among the matchable controls for each patient with CSFK in order to not facilitate our hypothesis. In case of the same CUTA degree of two or more matchable controls, the patient to include in the study was drawn in blind. We found two matchable controls in only seven circumstances (Fig. 1).
Exclusion criteria
For both cases and controls, patients with urinary tract infections (UTIs) before our observation, missing data, and parental denied consent to undergo diagnostic procedures were excluded (Fig. 1).
For controls, patients with bilateral CUTA or not matching with age at postnatal CUTA confirmation (1–3 months of life) or at last follow-up were excluded (Fig. 1).
CUTA diagnoses
All the patients underwent postnatal kidney ultrasound within 3 months from birth. The kidney ultrasound was made when they came for observation.
CSFK patients
In the CSFK group, the postnatal kidney ultrasound was performed because of prenatal suspect of CSFK with or without dilation of the urinary tract. Only 5 CSFK patients presented prenatal dilation of the urinary tract (1 with postnatal diagnosis of UPJO, 1 with postnatal diagnosis of non-obstructive hydronephrosis >15 mm, 1 with postnatal diagnosis of >10 mm megaureter, and 2 with postnatal diagnosis of severe VUR).
The CSFK was confirmed by Tc99mDMSA or Tc99mMag3 scintigraphy.
If CSFK patients presented hydronephrosis with anteroposterior diameter of the pelvis >15 mm or megaureter >7 mm at kidney ultrasound, they underwent Tc99mMag3 scintigraphy at first observation. These patients underwent further kidney ultrasounds 3 and 6 months later. If at this close follow-up an obstructive CAKUT was excluded, the patients underwent kidney ultrasounds biannually for the first 2 years of age, then annually until 5 years of age and then every 2 years. The UPJO was suspected on the basis of an increase of anteroposterior diameter of the pelvis during the follow-up associated with obstructive pattern at Tc99mMag3 scintigraphy or on the basis of anteroposterior diameter of the pelvis >30 mm associated with obstructive pattern at Tc99mMag3 scintigraphy. Among CSFK patients, in only one patient the diagnosis of UPJO was made because of anteroposterior diameter of the pelvis >30 mm associated with obstructive pattern at Tc99mMag3 scintigraphy. This patient underwent surgical correction.
As per our internal protocol, if CSFK patients presented with megaureter >15 mm at first observation persisting >15 mm after 3 months associated with obstructive pattern at Tc99mMag3 scintigraphy or presented with megaureter <15 mm reaching a diameter >15 mm during the following strict follow-up (see above) associated with obstructive pattern at Tc99mMag3 scintigraphy, the surgical correction was recommended. None of the enrolled CSFK patients needed surgical correction for megaureter.
Control group
In the control group, postnatal kidney ultrasound was performed because those patients already showed prenatal dilation of the urinary tract.
If patients presented hydronephrosis with anteroposterior diameter of the pelvis >15 mm or megaureter >7 mm at kidney ultrasound, they underwent Tc99mMag3 scintigraphy at first observation. These patients underwent further kidney ultrasounds 3 and 6 months later with a new Tc99mMag3 scintigraphy if they showed significant increase of dilation. Otherwise, the patients underwent kidney ultrasounds biannually for the first 2 years of age, then annually until 5 years of age and then every 2 years. If patients with pelvic dilation showed anteroposterior diameter of the pelvis >30 mm or reduction of the relative function at first Tc99mMag3 scintigraphy or reduction of relative function with delta >5% at subsequent Tc99mMag3 scintigraphy, they were diagnosed as affected by UPJO and underwent surgical correction; otherwise, they were considered as affected by non-obstructive hydronephrosis.
If patients with megaureter showed reduction of the relative function at first Tc99mMag3 scintigraphy or a reduction of relative function with delta >5% at subsequent Tc99mMag3 scintigraphs, they underwent surgical correction.
Both groups
As usually made in the clinical practice of our centre, the VUR had been diagnosed with cystography in males and with cystoscintigraphy in females.11
At cystoscintigraphy, grading of VUR comprised: mild—reflux to the ureter or renal pelvis without dilation; moderate—reflux to the renal pelvis with mild-to-moderate dilation; severe—distended redundant collecting system associated with ureteral dilation.12
If the megaureter was associated with VUR, we considered patients as only affected by VUR.
In patients with VUR, cystoscintigraphy was repeated at 2–3 years of age and, if persisting, at 5–6 years of age and at puberty.
All the patients with moderate-to-severe VUR or megaureter >10 mm, just after the diagnosis, started antibiotic prophylaxis, which was continued up to the first year of life in males and up to the second year in females.
Classification of population on the basis of CUTA severity
The severity and outcomes of CUTA in the two study groups were also evaluated after creating subgroups with comparable postdelivery detected CUTA. The subgroups included mild VUR (VUR grade I–II at cystography or mild to cystoscintigraphy), moderate VUR (VUR grade III at cystography or moderate at cystoscintigraphy), severe VUR (VUR grade IV–V at cystography or severe at cystoscintigraphy), > or < 15 mm (anterior-posterior diameter of the pelvis) non-obstructive hydronephrosis, and > or < 10 mm megaureter. Moreover, patients with moderate VUR, severe VUR, >15 mm non-obstructive hydronephrosis, and >10 mm megaureter were clustered under the umbrella term “severe CUTA”. The remaining patients were clustered under the term “non-severe CUTA”.
Other evaluations at follow-up visits
CSFK patients
After the end of the specific follow-up for an accurate CUTA definition (see above), CSFK patients were yearly evaluated until 5 years of age and then every 2 years. As previously described,2 at every follow-up visit of CSFK patients we routinely measured height, weight, body mass index with its standard deviation score (SDS), and blood pressure with its SDS. Blood pressure was measured, about 15 min after sitting, for 3 times by oscillometric measurements, with an interval of 5 min between measurements. The lowest value among three measurements was taken into account. Moreover, at every follow-up visit also serum creatinine (mg/dL) by Jaffè method with estimated glomerular filtration rate (eGFR) calculated by using the Schwartz equation,13 urinary protein/creatinine ratio (UPr/Cr), and renal ultrasound were evaluated. If the patients showed kidney injury, they were yearly evaluated but the renal ultrasound was biannually made.
Control group
The patients belonging to this group underwent the same follow-up visits and evaluations as that of the patients with CSFK with the exception of serum creatinine measurement that was evaluated every 3 years. As per our clinical practice, also when CUTA resolves, the patients continue periodical follow-up visits, with a periodical renal ultrasound with the aim to evaluate the renal growth and to detect the possible occurrence of renal asymmetry because it could be a sign of CUTA-associated nephropathy which—in our experience—could occur also later in life.
Both groups
In all patients with hypertension, renal arterial stenosis was excluded by Doppler ultrasound of the renal artery.
Febrile UTIs were defined by body temperature >38 °C, urinary leucocytes and/or nitrites, and positive urine culture. Urine culture was considered positive in the presence of ≥105 colonies/mL of a single species on a sample obtained by midstream clean catch specimens or >104 colonies/mL on samples obtained by bladder catheterization. The bladder catheterization was always employed in febrile incontinent patients.2
Kidney injury definition
Kidney injury was defined by either hypertension, or proteinuria, or reduced eGFR2:
Hypertension was defined by persistence of systolic (SBP) and/or diastolic (DBP) blood pressure >95th percentile corrected for age, sex, and height.14 To confirm the suspect of hypertension, these measurements were taken on 3 different occasions in a 3-month period.
Proteinuria was defined, on a first morning void, as persistent (confirmation within 3 months) UPr/Cr >0.5 mg/mg for children aged <2 years and >0.2 mg/mg for patients aged >2 years.
Reduced eGFR was defined by eGFR <90 mL/min/1.73 m2 for children aged >2 years and according to the specific reference values for age for children aged <2 years.15
Statistical analysis
p Values < 0.05 were considered statistically significant. Differences for continuous variables were analysed with the independent-sample t test for normally distributed variables and with Mann–Whitney test in case of non-normality. The normality was assessed by the evaluation of skewness and kurtosis. Values of skewness and kurtosis between −2 and +2 were considered acceptable in order to prove normal distribution.16
Qualitative variables were compared using chi-squared test.
The resolution of CUTA was determined by survival analysis according to the Kaplan–Meier method. The day of birth was considered as starting point, while the end point was the date of the CUTA resolution. The patients arriving at their last available follow-up without showing kidney injury were right censored. Kaplan–Meier curves were compared by log-rank test.
The Stat-Graph XVII software for Windows was used for all statistical analyses with the exception of Kaplan–Meier analyses made with the GraphPad Prism 7 software for Windows.
Results
Out of the 75 CSFK patients, 44 (58.7%) presented renal agenesis and 31 (41.3%) multicystic dysplastic kidney (MCDK). Extrarenal anomalies were present in 12 CSFK patients (1 patient with strabismus, 1 imperforate hymen, 3 cardiopathies, 1 hypospadias, 3 inguinal hernia, 1 cryptorchidism, 1 VATER syndrome, and 1 XYY syndrome).
General characteristics of both CSFK patients and controls are shown in Table 1. In both groups, we had 34 patients with VUR, 28 with non-obstructive hydronephrosis, 12 with megaureter, and 1 with UPJO for a total of 75 subjects in each group. In the control group, 13 patients presented reduced kidney length at ultrasound and reduced relative kidney function (<40%) at Tc99mMag3 scintigraphy of the kidney with CUTA when reaching last follow-up visit.
In the CSFK group, 9 patients presented kidney injury at last follow-up visit. Two of them presented proteinuria (UPr/Cr 0.29–0.31 mg/mg) and hypertension (SBP and DBP 2.5–3.0 SDS), 2 eGFR reduction (84-89 mL/min/1.73 m2) and proteinuria (UPr/Cr 0.39-0.52 mg/mg), 2 proteinuria (UPr/Cr 0.32–0.39 mg/mg), and 3 eGFR reduction (73–79 mL/min/1.73 m2).
In the control group, 6 patients (4 out of 6 with unilateral reduced kidney length at renal ultrasound and reduced relative function at Tc99mMag3 renal scintigraphy) presented kidney injury. Two of them presented proteinuria (UPr/Cr 0.30–0.35 mg/mg), 1 hypertension (SBP 2.5 SDS and DBP 3.3 SDS), and 3 patients eGFR reduction (76-85 mL/min/1.73 m2).
The rate of full adherence to the scheduled time of follow-up was 64.8% (57/88) among CSFK patients and 69% (1171/1697) among controls (p = 0.40). We prescribed antibiotic prophylaxis in 27 CSFK patients (15 with severe VUR, 7 with moderate VUR, and 5 with megaureter >10 mm) and in 40 controls (22 with severe VUR, 7 with moderate VUR, and 11 with megaureter >10 mm). The adherence rate to antibiotic prophylaxis was 96.3% (26/27) among CSFK patients and 92.5% (37/40) among controls (p = 0.64).
Compared with controls, patients with CSFK had lower prevalence of severe CUTA at first evaluation; lower prevalence of febrile UTIs, need of surgical correction, and need of surgical correction for obstruction and higher rate of spontaneous CUTA resolution during follow-up; and a similar prevalence of very mild kidney injury at last follow-up (Table 1). Patients with CSFK presented lower diameter of both renal pelvis in case of non-obstructive hydronephrosis and megaureter compared with controls (Table 1).
The grading characteristics of patients with VUR are shown in Table 2.
Separately analysing the populations of CSFK and controls, we found that patients with CSFK presented higher cumulative proportion of resolution from CUTA compared with controls (100 vs 39.3%; p < 0.001; Fig. 2a). Even separately analysing patients with severe CUTA, the CSFK patients presented higher cumulative proportion of resolution from CUTA compared with controls (100 vs 41.8%; p < 0.001; Fig. 2b). On the other hand, only a trend for faster CUTA resolution among patients with non-severe CUTA was evident in CSFK patients compared with controls (p = 0.09; Fig. 2c).
a Cumulative proportion of recovery from CUTA comparing patients with CSFK vs controls. The cumulative proportion of recovery for CSFK was 29.9% at 3 years, 35% at 6 years, 49.5% at 9 years, 57.4% at 12 years, 79.3% at 15 years, and 100% at 18 years, while for controls it was 10.4% at 3 years, 20.3% at 6 years, 23.0% at 9 years, 25.9% at 12 years, 25.9% at 15 years, and 39.3% at 18 years (p < 0.001). b Cumulative proportion of recovery from severe CUTA comparing patients with CSFK vs controls. The cumulative proportion of recovery for CSFK was 27.3% at 3 years, 37.8% at 6 years, 58.6% at 9 years, 63.7% at 12 years, 89.9% at 15 years, and 100% at 18 years, while for controls it was 8.2% at 3 years, 18.8% at 6 years, and 41.8% from 9 to 18 years (p < 0.001). c Cumulative proportion of recovery from non-severe CUTA comparing patients with CSFK vs controls. The cumulative proportion of recovery for CSFK was 26.8% at 3 years, 35.8% at 6 years, 46.1% at 9 years, 52.1% at 12 years, 69.2% at 15 years, and 100% at 18 years, while for controls it was 16.5% at 3 years, 24.1% at 6 years, and 34.9% from 9 to 18 years (p = 0.09).
Moreover, the CSFK subjects presented higher cumulative proportion of resolution than controls for VUR (85.6 vs 30.4%; p = 0.03; Fig. 3a). This significant difference persisted separately analysing patients with severe VUR (Fig. 3b) but was lost separately analysing patients with moderate (Fig. 3c) and mild VUR (Fig. 3d).
a Cumulative proportion of recovery from VUR comparing patients with CSFK vs controls. The cumulative proportion of recovery for CSFK was 38.8% at 3 years, 42.4% at 6 years, 58.9% at 9 years, 58.9% at 12 years, and 84.6% at 15 years, while for controls it was 20.4% at 3 years and 30.4% from 6 to 15 years (p = 0.03). b Cumulative proportion of recovery from severe VUR comparing patients with CSFK vs controls. The cumulative proportion of recovery for CSFK was 37.3% at 3 years, 46.3% at 6 years, 67.8% at 9 years, 67.8% at 12 years, and 100% at 13 years, while for controls it was 11.1% from 3 to 15 years and 23.2% from 6 to 15 years (p = 0.004). c Cumulative proportion of recovery from moderate VUR comparing patients with CSFK vs controls. The cumulative proportion of recovery for CSFK was 16.7% at 3 and 6 years, 58.8% at 9 and 12 years, and 100% at 15 years, while for controls it was 14.3% at 3 years and 48.6 from 6 to 14 years (p = 0.85). d Cumulative proportion of recovery from mild VUR comparing patients with CSFK vs controls. The cumulative proportion of recovery for CSFK was 53.7% at 3 years and 53.7% from 3 to 15 years, while for controls it was 40% at 3 years (p = 0.76). e Cumulative proportion of recovery from non-obstructive hydronephrosis comparing patients with CSFK vs controls. The cumulative proportion of recovery for CSFK was 11.2% at 3 years, 27.4% at 6 years, 31.9% at 9 years, 43.1% at 12 years, 62.7% at 15 years, and 100% at 18 years, while for controls it was 0% at 3 years, 9.4% at 6 years, 15.0% at 9 years, 21.6% at 12 years, 21.6% at 15 years, and 47.7% at 18 years (p = 0.03). f Cumulative proportion of recovery from non-obstructive hydronephrosis (>15 mm) comparing patients with CSFK vs controls. The cumulative proportion of recovery for CSFK was 12.5% at 3 years, 37.5% at 6 years, 37.5% at 9 years, 53.1% at 12 years, 53.1% at 15 years, and 100% at 18 years, while for controls it was 0% at 3 years, 8.3% at 6 years, 19.7% at 9 years, 19.7% at 12 years, 19.7% at 15 years, and 100% at 18 years (p = 0.31). g Cumulative proportion of recovery from non-obstructive hydronephrosis (<15 mm) comparing patients with CSFK vs controls. The cumulative proportion of recovery for CSFK was 10.3% at 3 years, 21.5% at 6 years, 28.6% at 9 years, 38.8% at 12 years, 67.4% at 15 years, and 100% at 18 years, while for controls it was 0% at 3 years, 10% at 6 years, 10.0% at 9 years, and 22.9% from 12 to 18 years (p = 0.048). h Cumulative proportion of recovery from megaureter comparing patients with CSFK vs controls. The cumulative proportion of recovery for CSFK was 35.2% at 3 years, 35.2% at 6 years, 74.1% at 9 years, 87.0% at 12 years, and 100% at 15 years, while for controls it was 18.5% at 3 years and 30.1% from 6 years to 18 years (p = 0.026).
The CSFK subjects presented higher cumulative proportion of resolution than controls for non-obstructive hydronephrosis (100 vs 47.7%; p = 0.03; Fig. 3e). This significant difference persisted separately analysing patients with non-obstructive hydronephrosis <15 mm (p = 0.048; Fig. 3g) but was lost separately analysing patients with non-obstructive hydronephrosis >15 mm (p = 0.31; Fig. 3f).
CSFK patients with megaureter presented higher cumulative proportion of resolution than controls (100 vs 30.2%; p = 0.026; Fig. 3h). Because almost all (11 out of 12; 91.7%) of controls presented megaureter >10 mm, we did not make Kaplan–Meier analysis for megaureter subgroups.
Discussion
This study was designed for a comparison between CSFK and non-CSFK patients with CUTA in terms of prevalence and of resolution rate of CUTA. All the enrolled patients presented prenatal suspicion of CSFK and/or CUTA and were evaluated very early in postnatal life, before the postnatal complications could have affected renal function. In addition to the strict criteria for matching, the rate of full adherence to the follow-up schedule was very similar between cases and controls.
We decided to not match the patients—a priori—for CUTA severity but only for age at first and at last follow-up and kind of CUTA. Adopting these inclusion criteria, we imitated common clinical situations. In fact, in the daily clinical practice paediatricians, neonatologists, paediatric urologists, and paediatric nephrologists generally face neonates with suspect of congenital anomalies of the kidney and urinary tract because of either prenatal ultrasound identifying a solitary kidney or a MCDK or unilateral/bilateral urinary tract dilation. In line with the recently published clinical recommendation about the care of children with CSFK,7 the first information deriving from the CSFK population analysed on the basis of these inclusion criteria is that it could not be useful to submit all the CSFK patients to cystography or cystoscintigraphy only for presenting with CSFK. This because—following this indication—most of the diagnosed VUR will be asymptomatic.
Moreover, these inclusion criteria allowed us to evaluate potential differences in CUTA severity between the patients with prenatal suspicion of CSFK and those with prenatal suspicion of CUTA on one of the two kidneys. We observed that the prevalence of severe CUTA was significantly higher in controls than in CSFK patients. This could be explained by the fact that prenatal ultrasounds are on average less reliable and will therefore pick-up only the more severe anomalies in the patients with two kidneys and guide them to the first postnatal ultrasound. In contrast, the patients with CSFK are controlled after birth also in case of less severe or absent CUTA only because they showed a solitary kidney.
Probably, for this study, the most proper inclusion criteria for the CSFK could have been the prenatal diagnosis of CSFK with dilation of the urinary tract. However, only five CSFK patients presented prenatal dilation of urinary tract making this selection criteria applicable only for future multi-centre studies. Therefore, this could have represented a bias of our study potentially determining that patients with two kidneys were more severely affected and needed longer time for resolution of dilation than CSFK patients. For this reason, we also separately analysed patients matched for the CUTA severity registered after birth.
We found that the CSFK patients showed higher rate of spontaneous CUTA resolution than controls (Fig. 2a), even separately analysing the subjects with severe CUTA (Fig. 2b). A similar trend was found among patients with non-severe CUTA (Fig. 2c). Moreover, separately analysing the patients with VUR, non-obstructive hydronephrosis, and megaureter, the CSFK patients still showed a higher cumulative proportion of resolution than controls (Fig. 3a, e, h).
Noteworthy, this data was confirmed analysing separately the patients with severe VUR (Fig. 3b). This could support a conservative approach to the VUR of CSFK patients also because in our series the prevalence of UTIs was low and the rate of spontaneous resolution was high. However, the possibility exists that the low rate of febrile UTIs we found could be linked to the extensive diagnostic approach with the precocious diagnosis of VUR followed by early antibiotic-prophylaxis administration. This specific issue should be further investigated in future studies. For example, it could be interesting to compare the rate of febrile UTIs of historical CSFK cohorts having undergone an aggressive diagnostic approach with the future cohorts of CSFK, which will be managed according to the new conservative recommendations.7
Our data about VUR in CSFK are in accord with the findings of Calaway et al. which showed that in their population of 133 MCDK patients only 2 patients had UTIs and only 3% needed surgical correction. On the other hand, our findings are different from those presented by Erlich et al. which, in their meta-analysis, showed that 18% of children with MCDK had UTIs and that 32% of patients with severe VUR had surgical correction.17 The differences with the study of Erlich et al.17 could be linked to the characteristics of our CSFK population. All our patients present prenatal diagnosis and have been enrolled within 3 months of life before any complication occurred. Moreover, all underwent cystography or cystoscintigraphy as per protocol and also if they did not show any sign raising the suspect of VUR at renal ultrasound.18 This could have avoided the oversampling of the most severely affected patients. In the meta-analysis of Erlich et al.,17 these inclusion criteria were not considered and then it is possible that the most severely affected patients could have been oversampled.
Managing asymptomatic patients with hydronephrosis is challenging, because the natural course of UPJO is variable and there is no reliable method to predict whether the function of a kidney with UPJO will remain unaffected or deteriorate with time.19 In the present study, we included non-obstructive hydronephrosis in the group of CUTA, as indicated by some authors,3,20 with the aim to show the evolution of non-obstructive hydronephrosis in the two groups. Classifying the patients with non-obstructive hydronephrosis on the basis of the dilation degree, we found higher cumulative proportion of resolution in CSFK patients compared with controls in case of <15 mm non-obstructive hydronephrosis (Fig. 3g) while in case of >15 mm non-obstructive hydronephrosis the Kaplan–Meir curves were similar (Fig. 3f). The high prevalence of resolution of non-obstructive hydronephrosis in patients with CSFK, as already shown in patients with isolated low-grade hydronephrosis and two kidneys,21 supports the conservative management in patients with CSFK.
The earlier and higher rate of megaureter resolution in CSFK patients than in controls can be due to the milder average grade of megaureter in CSFK patients (Table 1). In fact, the time to and the prevalence of primary megaureter resolution is influenced by its severity.22,23 Therefore, no definitive conclusions can be drawn for CSFK patients with megaureter. However, the Kaplan–Meier curve of our CSFK patients is reassuring towards conservative management.
The lower prevalence of severe CUTA in CSFK patients could justify the lower prevalence of febrile UTIs and need of surgical correction in CSFK patients than in controls. This is confirmed by the lower prevalence of subjects excluded for UTI before the first observation among CSFK patients compared with controls (Fig. 1).
CUTA may represent a major determinant of kidney injury in CSFK patients3,8,10 because of a possibly associated congenital nephron deficit/dysplasia in the remaining kidney.24,25 Independently from the severity of CUTA, we can speculate that patients with CUTA associated with CSFK could be at higher risk of kidney injury due to their halved starting nephronic mass and/or to the potential renal parenchymal dysplasia associated with CUTA. In fact, despite our patients with CSFK presented lower prevalence of severe CUTA, need of surgical correction for obstruction, and UTIs, they showed a similar prevalence of kidney injury compared with controls (Table 1).
In our population, only very few (three) patients were surgically managed not allowing a powered comparison of kidney injury rate among CSFK patients undergoing or not surgery. However, it could be of interest to make this comparison in future multi-centre studies, in order to improve our knowledge about pathophysiological mechanisms of kidney injury in CSFK patients and to have more information to consciously suggest surgical correction of non-obstructive CUTA in CSFK patients.
CSFK patients could present lower prevalence of severe CUTA than controls because more severe CUTA are associated with more severe kidney hypoplasia/dysplasia. This could produce CSFK embryo or foetus destined to abortion. In this way, only less severe CUTA of CSFK could allow foetuses survive up to birth.
A limitation of our study is the retrospective design. As mentioned above, another limitation could be the selection of controls with more severe CUTA. To counteract this limitation in the analysis of recovery from CUTA, however, subgroups of each CUTA with comparable severity were created. Finally, this study is based on a selected population of patients with careful follow-up in a specialistic centre and this might not reflect the average care of patients with CSFK.
In conclusion, this study adds information both from a practical and pathophysiological point of view. From a practical point of view, the relevance is represented by the fact that in our cohort most of the CSFK patients spontaneously recovered CUTA without surgery. This, in fact, could embolden a conservative management in a CSFK patient with non-obstructive CUTA. However, in the future years, following the current recommendations,7 the change in our diagnostic approach to CSFK patients from an aggressive to a conservative one could determine the diagnosis of only the symptomatic non-obstructive CUTA and then the comparison of the prevalence of kidney injury rate between the historical cohorts submitted to aggressive diagnostic approach and the future cohorts undergoing the new diagnostic approach could provide data supporting or not the conservative management of CSFK patients with non-obstructive CUTA that we hypothesize in the present paper.
Moreover, from a pathophysiological point of view, the fact that the patients with CSFK had lower prevalence of severe forms and better outcomes of their CUTA in spite of similar prevalence of kidney injury compared with controls could suggest that the poorer outcomes of CSFK patients with CUTA compared with CSFK without CUTA3,8,9,10 are mostly linked to congenital nephron deficit associated with CSFK rather than to postnatal complications related to the anomalies of the urinary tract.
References
Capone, V. P., Morello, W., Taroni, F. & Montini, G. Genetics of congenital anomalies of the kidney and urinary tract: the current state of play. Int. J. Mol. Sci. 18, 796 (2017).
Marzuillo, P. et al. Congenital solitary kidney size at birth could predict reduced eGFR levels later in life. J. Perinatol. 39, 129–134 (2018).
La Scola, C. et al. Congenital solitary kidney in children: size matters. J. Urol. 196, 1250–1256 (2016).
Westland, R., Schreuder, M. F., Bökenkamp, A., Spreeuwenberg, M. D. & Van Wijk, J. A. E. Renal injury in children with a solitary functioning kidney-the KIMONO study. Nephrol. Dial. Transplant. 26, 1533–1541 (2011).
Westland, R., Schreuder, M. F., Ket, J. C. F. & van Wijk, J. A. E. Unilateral renal agenesis: a systematic review on associated anomalies and renal injury. Nephrol. Dial. Transplant. 28, 1844–1855 (2013).
Schreuder, M. F., Westland, R. & van Wijk, J. A. E. Unilateral multicystic dysplastic kidney: a meta-analysis of observational studies on the incidence, associated urinary tract malformations and the contralateral kidney. Nephrol. Dial. Transplant. 24, 1810–1818 (2009).
Groen in’t Woud, S. et al. Clinical management of children with a congenital solitary functioning kidney: overview and recommendations. Eur. Urol. Open Sci. 25, 11–20 (2021).
Westland, R., Kurvers, R. A. J., van Wijk, J. A. E. & Schreuder, M. F. Risk factors for renal injury in children with a solitary functioning kidney. Pediatrics 131, e478–e485 (2013).
Poggiali, I. V. et al. A clinical predictive model of renal injury in children with congenital solitary functioning kidney. Pediatr. Nephrol. 34, 465–474 (2019).
Marzuillo, P. et al. Congenital solitary kidney from birth to adulthood. J. Urol. 205, 1466–1475 (2021).
Guarino, S. et al. In children with urinary tract infection reduced kidney length and vesicoureteric reflux predict abnormal DMSA scan. Pediatr. Res. 87, 779–784 (2020).
Polito, C., Rambaldi, P. F., La Manna, A., Mansi, L. & Di Toro, R. Enhanced detection of vesicoureteric reflux with isotopic cystography. Pediatr. Nephrol. 14, 827–830 (2000).
Schwartz, G. J., Brion, L. P. & Spitzer, A. The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr. Clin. North. Am. 34, 571–590 (1987).
Flynn, J. T. & Falkner, B. E. New clinical practice guideline for the management of high blood pressure in children and adolescents. Hypertension 70, 683–686 (2017).
Hogg, R. J. et al. National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative clinical practice guidelines for chronic kidney disease in children and adolescents: evaluation, classification, and stratification. Pediatrics 111, 1416–1421 (2011).
George, D. & Mallery, P. SPSS for Windows Step by Step: A Simple Study Guide and Reference, 17.0 Update (Allyn & Bacon, 2010)
Erlich, T., Lipsky, A. M. & Braga, L. H. A meta-analysis of the incidence and fate of contralateral vesicoureteral reflux in unilateral multicystic dysplastic kidney. J. Pediatr. Urol. 15, 77.e1–77.e7 (2019).
Marzuillo, P. et al. Early renal ultrasound in congenital solitary kidney may help to select patients at lower risk of associated vesico-ureteral reflux. Neonatology https://doi.org/10.1159/000516694 (2021).
Baskin, L. S. Congenital ureteropelvic junction obstruction - UpToDate. https://www.uptodate.com/contents/congenital-ureteropelvic-junction-obstruction?topicRef=6110&source=see_link (2019).
Jain, S. & Chen, F. Developmental pathology of congenital kidney and urinary tract anomalies. Clin. Kidney J. 12, 382–399 (2019).
Madden-Fuentes, R. J. et al. Resolution rate of isolated low-grade hydronephrosis diagnosed within the first year of life. J. Pediatr. Urol. 10, 639–644 (2014).
Calisti, A., Oriolo, L., Perrotta, M. L., Spagnol, L. & Fabbri, R. The fate of prenatally diagnosed primary nonrefluxing megaureter: do we have reliable predictors for spontaneous resolution? Urology 72, 309–312 (2008).
Oliveira, E. A. et al. Primary megaureter detected by prenatal ultrasonography: conservative management and prolonged follow-up. Int. Urol. Nephrol. 32, 13–18 (2000).
Schreuder, M. F. Safety in glomerular numbers. Pediatr. Nephrol. 27, 1881–1887 (2012).
Avner, E. D. et al. In Pediatric Nephrology 7th edn (eds Avner, E. D. et al.) 56–57 (Springer Berlin Heidelberg, 2016).
Funding
This paper was supported by funding with protocol number 204328/20 provided by Department of Woman, Child and of General and Specialized Surgery, Università degli Studi della Campania “Luigi Vanvitelli”.
Author information
Authors and Affiliations
Contributions
Study concept and design: P.M., C.P., S.G. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: P.M., E.M.d.G., G.D., P.F.R. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: P.M., G.R.U., D.L., E.M.d.G. Study supervision: P.M., A.D.S., L.L., M.P.B.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients before any procedure.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marzuillo, P., Guarino, S., Sessa, A.D. et al. Evolution of congenital anomalies of urinary tract in children with and without solitary kidney. Pediatr Res 92, 767–775 (2022). https://doi.org/10.1038/s41390-021-01781-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01781-3
This article is cited by
-
Primary non-refluxing megaureter: Natural history, follow-up and treatment
European Journal of Pediatrics (2024)
-
Early diagnosis of solitary functioning kidney: comparing the prognosis of kidney agenesis and multicystic dysplastic kidney
Pediatric Nephrology (2024)