Abstract
Background
Preterm infants have an increased risk of neurodevelopmental disorders. We established a direct quantitative comparison of the association between the degree of prematurity and three different neurodevelopmental disorders.
Methods
In this cohort study, we combined data from 995,498 children in the Danish Medical Birth Register, from birth years 1997–2013, with information on cerebral palsy, epilepsy, and special educational needs. We estimated the gestational week-specific prevalence and risk for each of the disorders.
Results
The risk ratio of cerebral palsy at gestational weeks 21–24, compared to term birth, was more than ten times higher than for the two other disorders. The prevalence of epilepsy and special educational needs declined almost parallel, with 9.2% (4.6%–13.5%) and 12.5% (11.2%–13.7%), respectively, per week of gestation toward term birth. Cerebral palsy did not decline similarly: from gestational weeks 21–24 until week 29 the prevalence declined insignificantly by 0.6% (−11.1%–11.0%) per week; whereas from week 29 until term, the prevalence declined markedly by 36.7% (25.9%–45.9%) per week.
Conclusions
The prevalence and risk of cerebral palsy are affected differently by the degree of prematurity compared with epilepsy and special educational needs, possibly reflecting important differences in cerebral pathophysiology.
Impact
-
For each week of gestation toward term birth, there was a clear log-linear decline in the prevalence of early childhood epilepsy and special educational needs.
-
In contrast, the risk of cerebral palsy was high at the earliest gestational age, and the prevalence did not decline significantly until gestational week 29, from where it declined notably by nearly 40% for each week of gestation until term birth.
-
Our results indicate important differences in the pathophysiological processes that associate preterm birth with these three neurodevelopmental disorders.
Similar content being viewed by others
Introduction
Advances in obstetric and neonatal care have resulted in increasing rates of survival in preterm infants. Nonetheless, preterm infants have an increased risk of a wide range of neurodevelopmental disorders,1,2 including cerebral palsy (CP),3,4,5,6 epilepsy7,8,9,10, and cognitive disorders.11,12 The risk of these disorders is highest at the lowest gestational ages (GA); however, it is usually analyzed in relation to broad GA groups.1,2,3,4,5,6,7,8,9,10,11,12
The etiological and pathophysiological basis for the increasing risk of neurodevelopmental disorders with decreasing GA is not entirely clear. Cerebral development during pregnancy is essential. The brain of the fetus grows approximately three-fold from GA 29 to 41, with a high proportional increase of cortical gray matter and myelinated white matter.13 Additionally, active proliferation of oligodendrocytes and maturation-dependent metabolic factors are believed to leave the brain of preterm infants vulnerable compared to the brain of infants born at term.14 Both white and gray matter abnormalities in preterm infants are associated with cognitive difficulties and CP.15,16 Although premature birth may not be the most important etiological factor in itself, it is a marker of a wide range of ante- and postnatal adversities on the causal pathway of neurodevelopmental disorders.17 For example, it was found that damage from oxidative stress in early developing white matter during pregnancy is comparable to levels of damage sustained from severe perinatal asphyxia,14 which aligns with the fact that children born at term surviving severe perinatal asphyxia are also at a high risk of developing CP, epilepsy, and cognitive disorders.18 The causal pathways and precise neural substrates for each of these disorders may differ, although they often co-exist.
We aimed to examine the direct quantitative association between the degree of prematurity and three neurodevelopmental disorders, CP, epilepsy, and cognitive disorders, respectively, as an indication of potential similarities and differences in their pathogenesis.
Materials and methods
Study design
This retrospective cohort study included all liveborn children born in Denmark during 1997–2013 registered in the Danish Medical Birth Register (DMBR). This nationwide database contains information related to every pregnancy and delivery in Denmark.19 We excluded children with missing GA; children born after 41 completed gestational weeks, according to early ultrasound; children who died before their first birthday; and children with a reported birth weight more or less than 6 standard deviations from the expected sex-specific weight for GA20 or a GA <20 completed weeks, since we assume their GA are incorrectly recorded.
In Denmark, all residents are assigned a unique civil registration number; this was used to link the individual information to four additional databases. To attach a diagnosis of CP, we linked data from two databases covering different periods. First, the Danish Cerebral Palsy Register contains data on all children born during 1997–2007 with a validated diagnosis of CP. The diagnosis was validated by one of four specialized neuropediatricians, after medical chart review, when the children were 5–6 years old.21 Second, the Cerebral Palsy Follow-up Program database contains data on all children born during 2008–2013 with a validated diagnosis of CP. The diagnosis was validated by one of 26 specialized neuropediatricians, after examining the children at ~4 years of age.22 To attach a diagnosis of epilepsy, we linked data from the Danish National Patient Register (LPR) that contains information on all individuals who have been discharged or seen in ambulatory clinics at Danish hospitals.23 The diagnoses are based on the International Classifications of Diseases 10th revision (ICD-10). We included all children with at least one diagnosis of epilepsy (ICD-10, G40–G41) in the first 6 years of life. In order to attach information on special educational needs (SEN)—as a measure of cognitive impairment—we linked data from the Danish Special Educational Register, which contains information regarding special educational needs in compulsory school. In Denmark, indication for SEN is based on a pedagogical and psychological assessment along with an assessment from the headmaster of the school, in consultation with the parents. SEN is registered if a pupil receives at least 9 h of support weekly and reporting to the register is mandatory by law. Only data on children with SEN attending primary and lower secondary school (grade 0–9, age 6 to 15+) during school years 2014/2015 and 2015/2016 was available; thus, the SEN analyses were done on a subset of the cohort born during 1999–2008. Children who had emigrated or died before their sixth birthday and children with missing information regarding SEN were excluded from the SEN analyses.
Children born between GA 21 + 0 and 36 + 6 were considered preterm, and children born between GA 37 + 0 and 41 + 6 were considered born at term. The number of children born in Denmark in the study period determined the sample size.
Approval was obtained by the Danish Data Protection Agency (P-2019-32). We did not have the approval to do cross-linking between the databases on CP and epilepsy with the Danish Special Educational Register. Therefore, analysis of the co-existence of SEN and the two other disorders in the same children could not be done. According to Danish law, ethical approval is not required for register-based studies.
Statistical analysis
Each gestational week from 25 to 36 was considered separately, defining a period of 7 days including day 0 to 6; very few surviving neonates were born between weeks 21 and 24, therefore, they were compiled into one group; children born at term, between weeks 37 and 41, were also compiled into one group and used as reference. This created a total of 14 GA groups.
Prevalence was calculated per 1000 with estimated 95% confidence intervals (CI). To estimate the association between GA and the prevalence of neurodevelopmental disorders; simple linear regression was performed for the prevalence of each disorder, estimating the change in percentage from one GA group to the next. Assumptions of linearity were fulfilled with log-transformation of the prevalence. A clear breakpoint in the slope of the log-transformed prevalence of CP was observed at gestational week 29. Therefore, splines were used to estimate the slope from the lowest GA group to 29 weeks and from 29 weeks to the group of children born at term. This was not deemed necessary for the two other disorders. A p-value less than 0.05 was considered statistically significant.
The association between GA and each disorder was estimated as the risk ratio (RR), with 95% CI, compared to the group of children born at term. Attributable risk fraction (AF) was calculated with 95% Wald CI for each GA group, as a measure of how much of the risk could be attributed to being born prematurely. AF was calculated as the prevalence of the disorder in the preterm GA group minus the prevalence in the group of children born at term, divided by the prevalence in the preterm GA group.
Data management and statistical analyses were performed using the R (version 4.0.3)24 and SAS (SAS Institute, Cary NC) statistical software.
Results
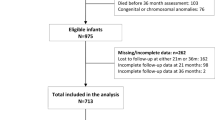
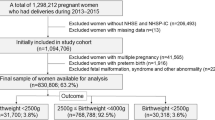
A total of 1,091,460 children born during 1997–2013 were identified in the DMBR. Among these, 25,334 (2.3%) had missing information about GA; 65,813 (6.0%) were born after GA 41; 3957 (0.2%) died before their first birthday and 858 (0.1%) had an assumed incorrectly registered GA (Fig. 1). A total of 995,498 (91.2%) children were included in the study cohort. In the cohort 67,695 (6.7%) children were born premature, 1937 (0.2%) had a diagnosis of CP, and 6649 (0.7%) had a diagnosis of epilepsy. 538 (0.1%) children had both disorders. When analyzing SEN in the cohort born during 1999–2008 (597,035 children, 60.0% of the total cohort), we further excluded: 684 (0.1%) who died between 1 and 6 years of age; 12,852 (2.2%) who emigrated before their sixth birthday; and 10,113 (1.7%) without information regarding SEN. This resulted in a total of 573,386 (96.0%) children with 24,710 (4.3%) having SEN (Fig. 1). The children with SEN were in grades 0–9, when the classification was made. Birth characteristics of the cohort according to the disorders are presented in Table 1.
The three disorders varied in prevalence, SEN being the most frequent with an overall prevalence of 43.1 (42.6–43.6) per 1000 children. In contrast, epilepsy and CP had an overall prevalence of 6.7 (6.5–6.8) and 1.95 (1.9–2.0) per 1000 children, respectively (Table 2). The prevalence of the disorders declined with an increasing degree of maturity as expected. The decline was parallel for epilepsy and SEN, with a decline of 9.2% (4.6%–13.5%, p = 0.001) per increased gestational week for epilepsy and 12.5% (11.2%–13.7%, p < 0.001) per week for SEN (Fig. 2). The prevalence of CP did not decline similarly: from the lowest GA group until week 29, the prevalence declined insignificantly with 0.6% (−11.1%–11.0%, p = 0.91) per week; from week 29 until “37–41 weeks”, the prevalence declined markedly with 36.7% (25.9%–45.9%, p < 0.001) per week of gestation (Fig. 2). Sensitivity analyses showed that the log-linear association between epilepsy and GA was not affected when removing children with both disorders of CP and epilepsy. Similarly, the association between CP and GA was not affected when excluding children with chromosome anomalies and/or birth defects. Moreover, to analyze if birth years and changing neonatal care, affected our results, we divided the cohort into two periods, for birth years 1997–2005 and 2006–2013, which did not change the association between GA and the neurodevelopmental disorders significantly (Supplementary Fig. 1).
Expressed as gestational week-specific RRs (with term birth as the reference), the increasing risk with decreasing GA was very clear, with a 70-fold increased risk for CP at the lowest GA group, which was more than 10-fold the corresponding quantity for epilepsy and SEN (Fig. 3).
Similarly, the AF of SEN and CP increased with decreasing GA (Table 2). Around 90% of the risk of developing CP in preterm children can be associated with their prematurity. In comparison, the total AF for both epilepsy and SEN was around 45%.
Discussion
In this national cohort study, we add to the knowledge on quantitative associations between early GA and three major neurodevelopmental disorders. We have demonstrated that the prevalence of epilepsy in early childhood as well as special educational needs in elementary school, declined steadily by about 10% for each gestational week the fetus remains in the womb until term birth. In comparison, the risk ratio for CP at the lowest GA was ten times higher and the prevalence of CP changed insignificantly until 29 weeks of gestation, then declined notably by nearly 40% for each gestational week until term GA.
The strengths of the study are the nationwide coverage of data for all three disorders and the substantial number of children included. The validity of the Danish education registers is very high.25 Moreover, the diagnosis of CP is validated by a specialized physician around the age of 4–5 years, with a reduced risk of misclassification bias. Additionally, a diagnosis of epilepsy in the LPR has been validated to have a positive predictive value of 79% when defining epilepsy according to the International League Against Epilepsy.26 It is not possible to validate if the children in our study have been diagnosed by a specialized physician accordingly, nonetheless, we do not believe that the validity is affected by GA.
The limitations of the study also relate to the data. Regarding SEN, data was limited to children attending compulsory school in the school years 2014/2015 and 2015/2016, meaning that only children from 10 of the 17 years were included. Preterm infants tend to have an increased risk of repeating grades, and special educational support might be granted more easily because of a history of preterm birth. Consequently, some bias toward the overestimation of the effect of prematurity cannot be excluded. Nevertheless, secular trends were relatively small for all GA groups, and importantly, we find potential biases likely to be small and believe the results in relation to SEN are comparable with those of the two other disorders.
The overall prevalence of the three disorders varied. SEN was relatively common with almost 5% overall; in contrast, epilepsy was only present in slightly <1%, and CP only in 0.2% of the total cohort.
The prevalence of preterm children with CP in Denmark has been stable for the last two decades.27 A systematic review from 2008, also found that the prevalence of CP probably varies little from GA 24 to 26 and decreases from gestational week 27 and onwards, however, the authors suggest that the interpretation should be guarded, since the denominator and definition of CP in the studies varied.3 Conversely, more recent studies from Norway and Finland found that the prevalence of CP was lower at the earliest gestational weeks compared with weeks 26–28.5,6 This seems counterintuitive. Theoretically, it should be worse, brain-wise, to be born at the margin of viability. One explanation could be effective centralization regarding the treatment of women at risk of premature birth and infants born before GA 28 in Denmark. The optimization of treatment may be particularly beneficial at the margin of viability, hence, lowering the risk of CP. However, a perhaps more likely explanation is that a GA bias influences the clinical decision-making processes regarding withholding or withdrawing life support particularly if the infant is in a poor condition at birth or if there are major complications or a high risk of severe brain injury. For example, major peri- and intraventricular hemorrhage is visible by cranial ultrasound in the first critical days of life and typically can involve the cortico-spinal tracts. Consequently, the probability of survival with a high risk of CP due to such injury may be less at the margin of viability. Furthermore, CP in preterm infants is often due to white matter injury (WMI) with persisting high risk until GA 3214,16 and it is not easily diagnosed by early cranial ultrasound. WMI developed at low GA is due to selected vulnerability of pre-oligodendrocytes that develops into immature oligodendrocytes from around GA 30 and onward, along with progressive myelogenesis and increasing resistance.28 These elements of pathophysiology correlate well with our results of declining prevalence from GA 29 (Fig. 2).
Epilepsy in preterm infants can be caused by both white and gray matter injury, with cystic periventricular leukomalacia and intraventricular hemorrhage being the most common findings on imaging, believed to disturb late neuronal migration and/or cortical development of cerebral circuits.29,30 The association between GA and the risk of epilepsy has previously been explored.7,8,9,10 Crump et al. found, in accordance with our study, a strong association with decreasing gestational age after adjusting for CP, although, presenting data from birth years 1973–1979,8 where the initial treatment of preterm neonates was markedly different than in the period of our cohort. Our results indicate that the association between early GA and epilepsy is different from that of CP, thus other important aspects of the causal paths are undescribed and require further investigation.
In contrast, SEN, compared with CP and epilepsy, is a measure of a broad spectrum of neurodevelopmental difficulties that are exposed in school, including general or specific cognitive deficits, attention deficits with or without hyperactivity, and problems of behavioral or psychic character, with immense contributions of socio-economic and cultural factors. This is further supported by the disproportionately high representation of male children with SEN, showing that male children have an ~2.5 higher risk of SEN compared to female children (Supplementary Table 1). Being a broad measure of functional impairment, it may be less surprising that the many adversities of brain development in preterm children add up to a clear “dose–response” relationship. The association between GA and SEN has previously been presented in two studies from Scotland and Denmark.11,12
The importance of our results is in the difference between CP and the other two neurodevelopmental disorders; since they indicate that the pathophysiological processes leading to CP in extremely preterm children are different from the two other disorders. The already high risk of developing WMI before gestational week 29 seems somewhat unconditional of GA, indicating that vulnerability of the pre-oligodendrocytes does not increase toward the margin of viability.28 Furthermore, for epilepsy and SEN survival of the fittest does not seem to provide a reduction of risk for the extremely preterm. Why? For SEN/cognitive impairment, the brain substrate is likely more related to protracted suboptimality of brain growth and development preceding and following preterm birth, rather than due to frank brain injury. For epilepsy, besides an oligodendrocyte-free substrate of brain damage,29 a speculative theory could be that kindling of epileptogenic circuits during the protracted period of postnatal care with abnormal sensory input to the developing neural circuitry also affects the risk of developing epilepsy in early childhood.
Our study demonstrates that the role of prematurity varies greatly among the disorders, it is far more influential in CP with an overall AF of 90% and risk ratio that is ten times higher than for epilepsy and SEN. In comparison, preterm birth precedes around 10% of children with SEN and early childhood epilepsy. AF can only be used as a first approach to causation31 since the causes and circumstances leading to preterm birth vary hugely as does the effect of prematurity on the fetal brain. Therefore, future studies should consider further address the differences in the pathophysiological processes and disorders that link preterm birth to neurodevelopmental disorders.
In conclusion, the risk of CP remains relatively high from the most extreme prematurity until gestational week 29, from when it declines steeply. In contrast with early childhood epilepsy and special educational needs, where the risk decreases log-linearly for each week of gestation until term birth. Furthermore, this study confirms that the proportion of outcomes that can be theoretically associated with preterm birth is substantially higher for CP than for the two other disorders.
References
Moster, D., Lie, R. T. & Markestad, T. Long-term medical and social consequences of preterm birth. N. Engl. J. Med. 359, 262–273 (2008).
Pascal, A. et al. Neurodevelopmental outcome in very preterm and very-low-birthweight infants born over the past decade: a meta-analytic review. Dev. Med. Child Neurol. 60, 342–355 (2018).
Himpens, E. et al. Prevalence, type, distribution, and severity of cerebral palsy in relation to gestational age: A meta-analytic review. Dev. Med. Child Neurol. 50, 334–340 (2008).
Oskoui, M. et al. An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev. Med. Child Neurol. 55, 509–519 (2013).
Trønnes, H. et al. Risk of cerebral palsy in relation to pregnancy disorders and preterm birth: a national cohort study. Dev. Med. Child Neurol. 56, 779–785 (2014).
Hirvonen, M. et al. Cerebral palsy among children born moderately and late preterm. Pediatrics 134, e1584–e1593 (2014).
Sun, Y. et al. Gestational age, birth weight, intrauterine growth, and the risk of epilepsy. Am. J. Epidemiol. 167, 262–270 (2007).
Crump, C., Sundquist, K., Winkleby, M. A. & Sundquist, J. Preterm birth and risk of epilepsy in Swedish adults. Neurology 77, 1376–1382 (2011).
Hirvonen, M. et al. The incidence and risk factors of epilepsy in children born preterm: a nationwide register study. Epilepsy Res. 138, 32–38 (2017).
Li, W. et al. Do premature and postterm birth increase the risk of epilepsy? An updated meta-analysis. Epilepsy Behav. 97, 83–91 (2019).
MacKay, D. F., Smith, G. C. S., Dobbie, R. & Pell, J. P. Gestational age at delivery and special educational need: retrospective cohort study of 407,503 school children. PLoS Med. 7, e1000289 (2010).
Wiingreen, R., Greisen, G., Svensson, J. & Hansen, B. M. Low gestational age at birth and difficulties in school—a matter of ‘dose’. PLoS ONE. 13, e0198482 (2018).
Hüppi, P. S. et al. Quantitative magnetic resonance imaging of brain development in premature and mature newborns. Ann. Neurol. 43, 224–235 (1998).
Back, S. A. Perinatal white matter injury: the changing spectrum of pathology and emerging insights into pathogenetic mechanisms. Ment. Retard. Dev. Disabil. Res. Rev. 12, 129–140 (2006).
Woodward, L. J. et al. Neonatal MRI to predict neurodevelopmental outcomes in preterm infants. N. Engl. J. Med. 355, 685–694 (2006).
Horber, V. et al. The origin of the cerebral palsies: contribution of population-based neuroimaging data. Neuropediatrics 51, 113–119 (2020).
Stoknes, M. et al. The effects of multiple pre- and perinatal risk factors on the occurrence of cerebral palsy. A Norwegian register based study. Eur. J. Paediatr. Neurol. 16, 56–63 (2012).
Simon, N. P. Long-term neurodevelopmental outcome of asphyxiated newborns. Clin. Perinatol. 26, 767–778 (1999).
Knudsen, L. B. & Olsen, J. The Danish medical birth registry. Dan. Med. Bull. 45, 320–323 (1998).
Maršál, K. et al. Intrauterine growth curves based on ultrasonically estimated foetal weights. Acta Paediatr. 85, 843–848 (1996).
Uldall, P., Michelsen, S. I., Topp, M. & Madsen, M. The Danish Cerebral Palsy Registry. A registry on a specific impairment. Dan. Med. Bull. 48, 161–163 (2001).
Rasmussen, H. M. et al. The Danish cerebral palsy follow-up program. Clin. Epidemiol. 8, 457–460 (2016).
Madsen, M. et al. The Danish National Hospital Register: a valuable source of data for modern health sciences. Dan. Med. Bull. 46, 263–268 (1999).
R Core Team. R: A Language and Environment for Statistical Computing, (R Foundation for Statistical Computing, Vienna, Austria, 2020). https://www.R-project.org
Jensen, V. M. & Rasmussen, A. W. Danish education registers. Scand. J. Public Health 39, 91–94 (2011).
Christensen, J., Vestergaard, M., Olsen, J. & Sidenius, P. Validation of epilepsy diagnoses in the Danish National Hospital Register. Epilepsy Res. 75, 162–170 (2007).
Larsen, M. L. et al. Continuing decline in the prevalence of cerebral palsy in Denmark for birth years 2008–2013. Eur. J. Paediatr. Neurol. 30, 155–161 (2021).
Back, S. A. et al. Late oligodendrocyte progenitors coincide with the developmental window of vulnerability for human perinatal white matter injury. J. Neurosci. 21, 1302–1312 (2001).
Tu, Y.-F. et al. Epilepsy occurrence after neonatal morbidities in very preterm infants. Epilepsia 60, 2086–2094 (2019).
Carrasco, M. & Stafstrom, C. E. How early can a seizure happen? Pathophysiological Considerations of extremely premature infant brain development. Dev. Neurosci. 40, 417–436 (2019).
Höfler, M. Causal inference based on counterfactuals. BMC Med. Res. Methodol. 5, 28 (2005).
Acknowledgements
This study was supported by the Elsass Foundation (19-3-0283). The funding parties did not have any involvement in the study.
Author information
Authors and Affiliations
Contributions
M.L.L., R.W., A.J., and G.G. created the concept and design. M.L.L., R.W., G.R., B.L., B.M.H., C.E.H.-H., and G.G. were a substantial part of data acquisition. M.L.L., R.W., and A.J. analyzed the data. M.L.L. and G.G. performed data interpretation. M.L.L., R.W., and G.G. created the original draft. All authors participated in critical reviewing and editing of the final version. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
No patient consent was required for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Larsen, M.L., Wiingreen, R., Jensen, A. et al. The effect of gestational age on major neurodevelopmental disorders in preterm infants. Pediatr Res 91, 1906–1912 (2022). https://doi.org/10.1038/s41390-021-01710-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01710-4