Abstract
Background
Preterm infants are commonly supported with 4–8 cm H2O continuous positive airway pressures (CPAP), although higher CPAP levels may improve functional residual capacity (FRC).
Methods
Preterm rabbits delivered at 29/32 days (~26–28 weeks human) gestation received 0, 5, 8, 12, 15 cm H2O of CPAP or variable CPAP of 15 to 5 or 15 to 8 cm H2O (decreasing ~2 cm H2O/min) for up to 10 min after birth.
Results
FRC was lower in the 0 (6.8 (1.0–11.2) mL/kg) and 5 (10.1 (1.1–16.8) mL/kg) compared to the 15 (18.8 (10.9–22.4) mL/kg) cm H2O groups (p = 0.003). Fewer kittens achieved FRC > 15 mL/kg in the 0 (20%), compared to 8 (36%), 12 (60%) and 15 (73%) cm H2O groups (p = 0.008). While breathing rates were not different (p = 0.096), apnoea tended to occur more often with CPAP < 8 cm H2O (p = 0.185). CPAP belly and lung bulging rates were similar whereas pneumothoraces were rare. Lowering CPAP from 15 to 5, but not 15 to 8 cm H2O, decreased FRC and breathing rates.
Conclusion
In all, 15 cm H2O of CPAP improved lung aeration and reduced apnoea, but did not increase the risk of lung over-expansion, pneumothorax or CPAP belly immediately after birth. FRC and breathing rates were maintained when CPAP was decreased to 8 cm H2O.
Impact
-
Although preterm infants are commonly supported with 4–8 cm H2O CPAP at birth, preclinical studies have shown that higher PEEP levels improve lung aeration.
-
In this study, CPAP levels of 15 cm H2O improved lung aeration and reduced apnoea in preterm rabbit kittens immediately after birth. In all, 15 cm H2O CPAP did not increase the risk of lung over-expansion (indicated by bulging between the ribs), pneumothorax, or CPAP belly.
-
These results can be used when designing future studies on CPAP strategies for preterm infants in the delivery room.
Similar content being viewed by others
Background
Respiratory support for preterm infants at birth has recently shifted from intubation and mechanical ventilation towards non-invasive strategies.1,2,3 Although these strategies are less harmful, the larynx may close during apnoea, which prevents air from entering the lungs when intermittent positive pressure ventilation (IPPV) is applied non-invasively.4,5,6,7,8 This can be avoided by stimulating and supporting spontaneous breathing, which facilitates opening of the larynx.4 While breathing can be enhanced by tactile stimulation, caffeine and 100% oxygen,9,10,11,12 this does not necessarily enhance lung aeration.12 To further improve respiratory support at birth, approaches that optimize lung aeration should also be adopted.
The process of lung aeration has been described extensively.13 At birth, the liquid that fills the airways during pregnancy must be cleared to allow the entry of air and the onset of pulmonary gas exchange. The process of liquid clearance is predominantly driven by transpulmonary pressures generated during spontaneous breathing.14,15,16 Each inspiration provides a pressure gradient for the movement of liquid through the airways and across the distal airway wall into lung tissue. As this airway liquid is replaced by air, a functional residual capacity (FRC) increases stepwise with each inspiration and, in term rabbits, an FRC of 10–15 mL/kg can be established within 3–5 breaths.14,15 As a result, during lung aeration, lung compliance markedly increases (~100-fold) and airway resistance markedly decreases, which greatly reduces the pressures required to inflate the lung. As this liquid accumulates within the interstitial tissue, it increases interstitial tissue pressures,17 which can result in liquid re-entry into the alveoli at end-expiration.15,16,17,18,19
Most preterm infants breathe at birth20,21 and are supported with continuous positive airway pressure (CPAP). The underlying rationale for this approach is to maintain end-expiratory lung volumes or FRC, because a positive end-expiratory pressure (PEEP) has been shown to maintain FRC in intubated and mechanically ventilated very preterm newborns. Indeed, 5 cm H2O of PEEP improves lung aeration and prevents alveolar liquid re-entry in very preterm rabbits (28/32 days, ~26–28 weeks human gestation (GA)).22,23,24 While this PEEP level lies within the pressure range (4–8 cm H2O) widely used for CPAP in the delivery room, it is unknown whether these pressures are optimal for assisting lung aeration in spontaneously breathing infants. For example, a PEEP level of 5 cm H2O is insufficient to maintain FRC in extremely preterm rabbits (27/32 days, ~24 weeks human GA),24 whereas a PEEP of 10 cm H2O markedly improves FRC and the uniformity of air distribution within the lung.25 Furthermore, in intubated preterm sheep, 8 cm H2O of CPAP enhances lung function and oxygenation compared with 5 cm H2O CPAP26 and a PEEP recruitment manoeuvre, which involves a stepwise increase and decrease in PEEP, has been shown to markedly improve lung function.27 However, while higher CPAP levels can improve lung function in preterm infants hours, and even up to days after birth,28,29,30,31 the use of CPAP in spontaneously breathing infants is markedly different from the use of PEEP during mechanical ventilation in intubated infants. Furthermore, as lung mechanics change dramatically during lung aeration, it is currently unclear whether the CPAP level used to assist lung aeration in spontaneously breathing preterm infants should change in conjunction with lung aeration.
Immediately after birth when liquid fills the airways, the viscosity of liquid and its movement through the airways and across the distal airway wall creates a high resistance to the entry of air. As the infant must generate high transpulmonary pressures during inspiration to overcome this resistance, it is possible that a high CPAP level at the mouth opening will assist infants in generating these transpulmonary pressures. However, as the lung becomes more aerated, airway resistance markedly decreases and so the pressure gradients required to move a tidal volume of air decreases. At this time, the role of CPAP changes to preventing liquid re-entry and alveolar collapse and, thus, lower CPAP levels are likely sufficient to maintain FRC.13,14,15,22,32 Considering the underlying physiology at birth, we suggest that preterm infants may initially benefit from high CPAP levels that are then reduced as the lung aerates.
The aim of this study was to investigate the effect of different CPAP levels on lung aeration and spontaneous breathing in very preterm rabbits after birth. We hypothesized that commencing respiratory support with higher CPAP levels will improve aeration and reduce the risk of apnoea, and that these beneficial effects can be maintained after the CPAP level is reduced.
Methods
Ethics statement
Study procedures were approved by the SPring-8 Animal Care and Monash University’s Animal Ethics Committees.
Experimental protocol
Anaesthetics for pregnant doe (Fig. 1a).
Simplified summary of the method section, subdivided in a Anaesthetics for pregnant doe, b Delivery of preterm kitten and experimental preparation, c Respiratory support and CPAP intervention protocol and d Completing study duration. CPAP continuous positive airway pressure, FiO2 fraction of inspired oxygen, IPPV intermittent positive pressure ventilation, i.p. intraperitoneal, i.v. intravenous.
At 29/32 days GA (~26–28 weeks human GA), pregnant New Zealand White rabbits (n = 15) were anaesthetised via an intravenous bolus of propofol (8 mg/kg; Rapinovet, Merck Animal Health) followed by a maintenance dose (~150–400 mg/h; rate ~15-30 mL/h) and additional boluses (0.5–1 mL) if required. Does were supported with oxygen via face mask while breathing, saturation and heart rate (Radical 7, Masimo, CA, USA) were monitored. Spinal anaesthesia was induced by injecting 1:1 bupivacaine (0.6 mL, 0.5%) and lignocaine (0.6 mL, 2%) into the lower spine using a 22G epidural catheter (BD 405254). Once hind quarter reflexes were absent, propofol administration was ceased and sedation continued by intravenous infusion of midazolam (1 mg/kg/h) and butorphanol (1 mg/kg/h) diluted in saline (20–23 mL/h).
Delivery of preterm kittens and experimental preparations (Fig. 1b)
Kittens were delivered via caesarean section. The umbilical cord remained intact and was covered with diclofenac diethylammonium (Voltaren Emugel, GlaxoSmithKline Consumer Health B.V, UK). A custom-made oesophageal tube was inserted, with the tip located in the mid thoracic region. This tube exited through a custom-made, soft rubber face mask that was placed over the kitten’s head and sealed with tissue glue to prevent leak if necessary (small kittens). The umbilical cord was then clamped, and the kitten weighed before it received naloxone (0.2 mg/kg), anexate (10 μg/kg) and caffeine (20 mg/kg) injected intraperitoneally to reverse maternally administered sedatives/analgesics and to stimulate spontaneous breathing. Kittens were then transferred to the imaging hutch, placed on their right side on a heated platform and connected to a temperature probe, oximeter and ECG leads. The face mask was connected to a custom-build ventilator in CPAP mode,33 whereas the oesophageal tube was connected to a pressure transducer to detect breathing (BP Transducer/Cable Kit, ADInstruments, New South Wales Australia). All devices were connected to a PowerLab and LabChart data acquisition system (ADInstruments, NSW, Australia) for continuous physiological recording.
All kittens were included, except if they were stillborn or were too small for instrumentation (<15 g).
Respiratory support and CPAP intervention protocol (Fig. 1c)
The experiment began when the kittens were attached to the recording equipment and imaging commenced as soon as the kittens were judged to have a stable breathing pattern. Respiratory support was initiated with CPAP and 100% oxygen, while tactile stimulation was used to encourage breathing. Kittens continued to receive 100% oxygen throughout the study period. On the indication of apnoea (absence of breathing for 4–5 s), IPPV was applied (PEEP 5, PIP 35 cm H2O, 1:1 inflation: deflation time of 500 ms each). If kittens did not re-establish stable breathing following IPPV, imaging was interrupted, the imaging room entered and kittens received tactile stimulation.
Kittens were randomly divided into five groups although we aimed not to include more than one kitten from each mother to anyone group. Depending on the group, respiratory support was commenced with an initial CPAP level of 0, 5, 8, 12 or 15 cm H2O CPAP. Kittens that initially received 15 cm H2O were further sub-divided into three groups to either (i) maintain CPAP continuously throughout the experiment or to decrease CPAP to (ii) 5 or (iii) 8 cm H2O. In the latter two groups (called the dynamic CPAP groups), once the lungs were visibly aerated (as indicated by imaging) and the kittens had achieved a stable breathing pattern, CPAP was decreased in a stepwise fashion at a rate of ~2 cm H2O per 30 s. These pressures (5–8 cm H2O) reflect the lower- and upper limit of the recommended CPAP range in the Australian and New Zealand neonatal resuscitation guidelines.34 The administered CPAP levels were adjusted by measuring the delivered pressure at the face mask outlet.
Study duration (Fig. 1d)
Studies in each kitten continued for up to 10 min, with imaging occurring for as long as possible during this time. However, the study was stopped early and kittens were excluded from the analysis (or parts thereof) if the kittens developed pneumothoraxes or if there were technical problems. After completing the study, all animals were euthanized with sodium pentobarbitone (Somonopentyl, Kyoritsu Seiyaku Co., Tokyo, Japan) (>100 mg/kg). Does were injected intravenously with 6 mL 1:2 sodium pentobarbitone diluted in saline and kittens were injected intraperitoneally with 0.3 mL (sodium pentobarbitone).
Phase contrast X-ray imaging
Phase contrast X-ray imaging was used to image lung aeration and to quantitatively determine lung gas volumes as described previously.12,35 The study was conducted in experimental hutch 3 of beamline 20B2 in the Biomedical Imaging Centre at the SPring-8 synchrotron in Japan. Due to the number of animals used in this study the experiment was extended over two beamtimes. All images were acquired using a Hamamatsu ORCA Flash C11440-22C detector coupled to a 25 μm gadolinium oxysulfide phosphor and a tandem lens system (effective pixel size 15.4 μm, 2048 × 2048 pixels). The synchrotron X-ray source was tuned to 24 keV with a source to detector distance of ~210 m. Data from 2017 (n = 48) were collected with a sample to detector distance of 2 m, a frame rate of 10 Hz, and a 20 ms exposure time. Data collected in 2019 (n = 29) had a sample to detector distance of 1.5 m, frame rate of 15 Hz, and 15 ms exposure time.
After each kitten was imaged flat and dark field images were collected and used for image correction prior to analysis. The lung gas volume was determined from each image using a power spectrum analysis.35 This technique relates the power spectrum of the lung to the lung gas volume via a calibration that is specific for each experimental set up, allowing the results from the two beamtimes to be combined. The methodology described by Leong et al.35 was extended to include a normalization factor of the lung size of the individual kitten as this improves the calibration by correcting for natural animal variations. The power spectrum analysis is sensitive to rapid changes in intensity, so features such as the air–skin interface and an ECG lead were identified in the images and replaced with the mean pixel value.
As imaging data could only be collected when the hutch is locked and the X-ray beam is on, if the kittens required any manual intervention, the X-ray imaging had to cease to allow entry into the hutch. Imaging and breathing data were synchronized by recording the camera trigger along with the physiological data in LabChart (Powerlab, ADInstruments, Sydney, Australia).
Other outcome measures
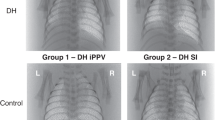
Outputs from the pressure transducer (attached to the oesophageal tube), oximeter, and temperature probe were digitized and recorded by Labchart. Breathing rates were derived from the intrathoracic oesophageal pressure measurements and calculated as (60 s/interval duration in seconds) × number of breaths. All outcomes were assessed while the kittens were on CPAP and were spontaneously breathing on CPAP, prior to the start of IPPV. Other outcome measures include periods of IPPV. If a pneumothorax was clearly visible during imaging (Fig. 2a), this resulted in the immediate cessation of the experiment for that kitten. CPAP belly (defined as air within the stomach that changed the shape of the abdomen, Fig. 2b, c) and bulging of the non-dependent (in the figure, upper) lung between the ribs at end-expiration (categorized as non/minor/significant, Fig. 2d–f) and were visually assessed by TM, SH, and AtP after the experiment.
Phase contrast X-ray images showing a a pneumothorax, b CPAP belly that was assessed as insignificant when the stomach contained air, but did not change the shape of the abdomen, and c CPAP belly that was assessed as significant when the amount of air within the stomach affected the shape of the abdomen. Bulging of the non-dependent lung between the ribs was assessed at end-expiration as either d absent, e minor, or f significant.
Statistical analysis
Data were analysed using SPSS Statistics version 25.0 (IBM Software, Chicago, IL, 2016). Post hoc analyses were performed using the false discovery rate. Statistical significance was accepted when p value < 0.05.
Categorical data were compared with a Pearson chi-square test, Fisher’s exact test, or log-rank survival analysis and presented as n (%). Numerical outcomes were compared using independent-samples Kruskal–Wallis test or related-samples Wilcoxon signed rank test and presented as median (Q1–Q3).
To compare parameters over time, a mean was calculated over 30 s intervals every minute, during both CPAP and IPPV. Linear mixed-effect regression models accounted for the relation between multiple measurements of the same kitten with a first-order autoregressive covariance structure on residuals. Group, time and group × time interactions were included in the model as fixed factors and random effects. Group p values were used to compare means between groups. Data are presented as the median (Q1–Q3).
Friedman’s test analysed the response to reductions in CPAP levels over time within a group. Missing values were completed using the mean value of the group.
Results
Prior to the experiment, kittens were not included if they were delivered stillborn (n = 6) or were too small for instrumentation (n = 2). During or after the experiment, kittens were excluded due to equipment failure (n = 4), tube positioning and/or pressure instability (n = 8) or other technical problems (n = 6). In total, 77 kittens were included in this study. Five kittens were included from the study of Dekker et al.12 as the circumstances under which these experiments were performed were identical. Kittens were excluded from the FRC and/or breathing analysis if they developed a pneumothorax (n = 2) or poor results from the image analysis due to movement (n = 3). Baseline characteristics were similar between groups (Table 1).
Comparison of initial CPAP levels
During the first 10 min after birth, FRC was significantly lower (p = 0.003) in kittens receiving CPAP of 0 and 5 cm H2O compared to kittens receiving a CPAP of 12 and 15 cm H2O (Fig. 3a and Table 2). Significantly fewer kittens reached FRCs >15 mL/kg on a CPAP of 0 cm H2O, compared to CPAP levels of 8, 12 and 15 cm H2O (p < 0.001, Fig. 3b and Table 2). Kittens supported by 0 and 5 cm H2O of CPAP achieved significantly lower maximum FRCs compared to kittens receiving CPAP levels of 12 or 15 cm H2O (p < 0.001, Fig. 3c and Table 2). The final FRC measurement was significantly lower in kittens receiving 0 cm H2O of CPAP compared to 15 cm H2O CPAP (p = 0.003, Fig. 3d and Table 2).
Effect of CPAP level on FRC. a Median (Q1–Q3) change in FRC over time (t0 = equipment ready) within each group; data obtained during IPPV has been included. b Percentage of kittens in each group reaching FRC > 15 mL/kg while on CPAP. c Median (Q1–Q3) of maximum FRC that kittens reached while on CPAP. d Median (Q1–Q3) of final FRC measurement while on CPAP, measured either at end-experiment or prior to the start of ventilation. An asterisk (*) indicates significant differences between groups.
Breathing rates were not statistically significant different across all groups over time (p = 0.096, Fig. 4a and Table 2) or when calculated as area under the curve (AUC) (p = 0.118, Fig. 4b and Table 2). Maximum breathing rates of kittens receiving 0 cm H2O CPAP were significantly lower than those on 5, 12 and 15 cm H2O of CPAP (p = 0.028, Fig. 4c and Table 2). Similarly, while the incidence of apnoea was not significantly different between groups (p = 0.185, Fig. 4d and Table 2), the risk of apnoea over the first 10 min after birth was approximately double in the 0 and 5 cm H2O groups compared to the 12 and 15 cm H2O CPAP groups.
Effect of CPAP level on spontaneous breathing. a Median (Q1–Q3) breathing rate for each group plotted over time (t = 0, equipment ready). b Area under the curve (AUC) of the breathing rate measured over the first 10 min. c Maximum breathing rate achieved while breathing spontaneously on CPAP for each of the different CPAP levels. d Time line for the risk (%) of kittens becoming apnoeic (t0 = equipment ready) within each CPAP group. An asterisk (*) indicates significant differences between groups.
The incidence of lung bulging between the ribs (p = 0.159), pneumothorax (p = 0.347), and CPAP belly (p = 0.756) were not different between groups (Table 2). Due to technical problems, there were insufficient data acquired to analyse the ECG and pulse oximeter measurements to compare heart rate or oxygen saturation.
Rescue interventions
During apnoea, prior to the start of IPPV, kittens (from all groups) had FRC values ranging from 0.4 to 15.5 mL/kg. Following the use of rescue interventions (IPPV and tactile stimulation if necessary), both FRC (median (Q1–Q3) before vs after, 1.3 (0.7–8.9) to 15.5 (9.4–21.2) mL/kg, p < 0.001) and breathing rates (4 (1–9) to 41 (26–48) breaths/min, p < 0.001) were significantly increased.
In total, 42% of the kittens that became apnoeic, started breathing during IPPV without any stimulation. The remaining 58% required tactile stimulation to end apnoea and they received IPPV for 1.14 (0.44–2.10) min before tactile stimulation commenced. Tactile stimulation was successful in terminating apnoea and re-establishing breathing within 17 (15–20) s. In all kittens who required tactile stimulation in addition to IPPV, FRC only increased after they received tactile stimulation and had recommenced breathing.
Changing CPAP levels
In the dynamic CPAP groups, respiratory support was initiated with 15 cm H2O and CPAP was then decreased to 5 and 8 cm H2O after 5:26 (2:53–6:16) and 4:01 (3:01–4:36) min, respectively. Decreasing CPAP from 15 to 5 cm H2O significantly decreased FRC from 17.5 (16.5–20.2) before change to 15.4 (13.6–18.6) mL/kg (median (Q1–Q3) up to 2 min after the end of the CPAP decrease (χ2 (3) = 14.127, p = 0.003, Fig. 5a). Similarly, breathing rates were reduced significantly from 40 (26–49) to 27 (14–42) breaths/min at 3 min after the CPAP had been decrease to 5 cm H2O (χ2 (4) = 14.922, p = 0.005, Fig. 5b). Decreasing CPAP levels from 15 to 8 cm H2O did not reduce FRC (18.9 (4.1–23.4) to 19.8 (12.4–23.2) mL/kg, χ2 (4) = 3.437, p = 0.487, Fig. 5a) or breathing rates (35 (30–40) to 37 (35–46) breaths/min, χ2 (4) = 6.210, p = 0.184, Fig. 5b).
Effect of reducing CPAP levels from 15 cm H2O to either 8 or 5 cm H2O on a functional residual capacity (FRC; median (Q1–Q3)), b breathing rates, c FRC levels measured at experiment end and d breathing rates measured at experiment end. Measurements were taken after CPAP decrease started with t = 0 indicating the end of CPAP changes. An asterisk (*) indicates significant changes within groups.
At the end of the experimental period, there were no differences in FRC when comparing the continuous 15 cm H2O (20.5 (14.2–24.5) mL/kg) CPAP and dynamic 15 to 5 cm H2O (18.7 (5.6–22.6) mL/kg) and 15 to 8 cm H2O (18.2 (14.2–22.1) mL/kg) CPAP strategies (p = 0.518, Fig. 5c). However, final breathing rates were 26 (11–41) breaths/min in the 15 to 5 cm H2O group, compared to 34 (28–48) breaths/min in the 15 cm H2O and 40 (35–48) breaths/min in the 15 to 8 cm H2O CPAP groups (p = 0.059, Fig. 5d) at experiment end.
Discussion
This is the first study to compare the effects of CPAP levels on FRC at birth in spontaneously breathing very preterm rabbits. We found that high CPAP levels, which are higher than those currently used clinically, improved lung aeration. Kittens that were supported with 15 cm H2O CPAP reached higher mean, maximum and final FRC levels and more kittens attained FRCs of >15 mL/kg during the immediate newborn period (up to 10 min after birth). The results of this study also suggest that higher CPAP levels better support spontaneous breathing immediately after birth. While breathing parameters did not reach statistical significance between groups, the occurrence of apnoea was markedly lower in preterm kittens supported with CPAP levels of ≥12 cm H2O. Furthermore, we found that CPAP levels of up to 15 cm H2O did not increase the risk of lung bulging between the ribs, the incidence of pneumothoraxes or CPAP belly immediately after birth.
Our findings that CPAP levels markedly improve lung aeration are consistent with previous studies showing that higher PEEP levels improve lung aeration at FRC in intubated and mechanically ventilated newborns at birth.23,24,25 However, these modes of respiratory support are substantially different, particularly as intubation removes the larynx from the respiratory circuit. In contrast, the larynx and upper airways are in circuit when respiratory support is provided non-invasively. Previously it has been shown that during apnoea, the larynx closes, which can prevent air from entering or leaving the lungs,4,5,6,7,8 whereas during spontaneous breathing the larynx is mostly open, but may close briefly (expiratory braking manoeuvres) to maintain FRC.36 We have also recently shown that the larynx can regulate the pressure applied to the sub-glottic airways during CPAP.37 When preterm sheep received 5–8 cm H2O CPAP, this entire pressure was transmitted to the lungs, while only a proportion (~75%) of the pressure was transmitted into the lungs when 15 cm H2O CPAP was given non-invasively. While this could be a mechanism that protects the lung from high pressures that could overinflate the lung, it is not clear how and when this protective mechanism is activated during lung aeration.5,37 In this study, kittens that received 15 cm H2O CPAP non-invasively via a face mask had improved lung aeration without giving any indications of overinflation. This was assessed as bulging of the lung between the ribs (Fig. 2d–f) and the incidence of a pneumothorax, which were rare (2/77), only occurring in the 0 and 8 cm H2O groups. This finding suggests that higher pressures may have reached the lower airways initially to facilitate lung aeration, but following lung aeration, volume receptors in the lung may have triggered laryngeal protective mechanisms that prevented over-expansion of the lung.
In addition to the benefits we observed, it is possible that our study underestimated the true benefit of high CPAP levels on lung aeration and respiratory function immediately after birth in very preterm rabbits. All kittens were required to breath spontaneously while on CPAP, but if the kittens became apnoeic, rescue interventions (e.g. IPPV and tactile stimulation) were required. However, apnoea occurred much more frequently in kittens receiving 0, 5 and 8 cm H2O CPAP, compared with 12 and 15 cm H2O. Indeed, as the apnoeic kittens required rescue interventions (iPPV and/or tactile stimulation) to increase breathing and FRC, it is possible that these rescue interventions lessened the differences between groups. While we were unable to acquire reliable oxygen data, due to the well-known relationship between hypoxia and apnoea in fetuses and newborns, it is highly likely that breathing, or lack thereof, in these kittens is a sensitive indicator of oxygenation status.38,39
Although IPPV was successful in re-establishing breathing in 42% of kittens that were assessed as apnoeic (breath intervals >4–5 s), the presence of spontaneous breaths, albeit at a low rate (i.e. <12–15 breaths/min), were essential to re-establishing regular breathing. As IPPV alone was not able to re-establish breathing in 58% of apnoeas, it is the combined effect of spontaneous breathing and IPPV, particularly when a breath and inflation coincided, that led to the increase in lung aeration and the re-establishment of breathing.11,40 When this occurs, the larynx is open4 and so the pressure in the face mask is up to 35 cm H2O (in this study) during inspiration (i.e. at PIP during IPPV), which is substantially greater than a CPAP level of 15 cm H2O. While the resulting large pressure gradients, generated by inspiration plus the inflation pressure, partially explains the increase in lung aeration we observed following rescue interventions, it also risks lung over-expansion and injury. Indeed, as the pressure in the face mask cycles between 5 and 35 cm H2O which may or may not coincide with spontaneous breathing, the inherent physiological feedback controls that normally regulate tidal volumes will be ineffective. We suggest that this is a normal scenario that occurs in the delivery room when very preterm infants receive IPPV and inflations come into and out of synchrony with inspiratory efforts. This may contribute to the large variation in tidal volumes that have been reported in very preterm infants.41,42,43
The incidence of apnoea was not statistically different between groups, yet the incidence of apnoea appeared to be markedly higher in the rabbits receiving 0–8 cm H2O CPAP (36–46%) as compared to those rabbits receiving 12–15 cm H2O CPAP (16–20%). This difference was even more pronounced in preterm lambs, with 83% of lambs supported with 5 cm H2O CPAP becoming apnoeic compared to only 17% of lambs supported with 15 cm H2O CPAP.37 We suggest that higher CPAP levels better support spontaneous breathing by improving lung aeration, which increases the lung’s surface area for gas exchange and thereby improves oxygenation, which sustains breathing activity. Indeed, hypoxia is a potent inhibitor of breathing in the foetus and newborn and is likely to be a major cause of apnoea.38,39 Alternatively, CPAP may also reduce alveolar collapse and thereby reduce breathing efforts, making it easier for an infant to breathe.44 We speculate that this may explain our anecdotal observation that the amplitude of the intrathoracic pressure reductions associated with breathing increased with decreasing CPAP level; these data have not been analysed as the pressure amplitude is highly sensitive to positional changes.
The effect of CPAP levels on breathing rates is unclear and appear contradictory, likely because they are influenced by multiple competing factors. We have shown that breathing rates are higher when preterm rabbits are supported by CPAP, but there seemed to be little difference between different CPAP levels. Intubated preterm lambs showed no difference in breathing rates when supported by 5 or 8 cm H2O,26 but lambs achieved higher breathing rates with 15 compared to 5 cm H2O CPAP.37 While these results may appear contradictory, there were major differences in the level and timing of interventions that stimulate breathing. For example, while tactile stimulation is hard to standardize even when there is direct access to the newborn, access to the animal was greatly limited in these synchrotron studies. Indeed, tactile stimulation could only be applied by ceasing imaging and gaining access to the imaging hutch. Thus, differences in the degree of tactile stimulation may have obscured the effect of increased lung aeration and oxygenation on breathing rates. Alternatively, increasing pressure applied to the face and/or airways may have countered the stimulation of respiratory activity in kittens receiving high CPAP via activation of neural receptors on the face (trigeminal nerve) or activation of lung volume receptors.45,46,47,48 In a previous study we have shown that, after establishing lung aeration, increasing CPAP ≥ 7 cm H2O greatly reduces breathing activity in preterm rabbit kittens.4 It appears that immediately after birth, CPAP levels do not affect breathing rates, but when the pressure is suddenly increased after lung aeration it may trigger a Hering-Breuer or trigeminal reflex that protects the airways from high pressures.45,46,47,48
Current recommendations suggest using CPAP levels of 5–8 cm H2O, as higher CPAP levels may increase the risk of lung over-expansion injury and pneumothoraces. We found no indications that, when applied immediately after birth, CPAP levels of 12–15 cm H2O caused lung over-expansion or increased the risk of pneumothorax or CPAP belly in preterm rabbits. We have also recently found that 15 cm H2O CPAP does not impede the increase in pulmonary blood flow at birth in spontaneously breathing preterm sheep.37 In contrast, a PEEP of ≥8 cm H2O in intubated and mechanically ventilated preterm lambs significantly reduces pulmonary blood flow and increases the risk of a pneumothorax.49,50,51,52 These discrepancies highlight the fundamental differences between the two respiratory modes. When infants are supported with CPAP, the CPAP level is effectively the highest external pressure applied to the airways and pressures in the lower airways only transiently exceed the CPAP level to effect expiration. With each breath, the intrathoracic pressures phasically decrease below the CPAP level, thereby reducing the mean airway pressure below the CPAP level. During IPPV, the PEEP level is the lowest externally applied pressure. As the pressures phasically increase above this with each inflation, the mean airway pressure is higher than the PEEP level and is substantially higher than occurs with a similar CPAP level during spontaneous breathing.
It is also important to consider that the timing after birth when the support is applied is also relevant, with the lung being more resistant to the adverse effects of higher pressures when liquid-filled. This is consistent with the finding that the risk of a pneumothorax was not increased when using PEEP levels ≤15 cm H2O in very preterm infants.53,54,55 Nevertheless, it would appear that there is a limit to how much pressure is appropriate in the first few minutes after birth. Indeed, a retrospective comparison study between two hospitals has shown that CPAP levels of 12–35 cm H2O increased the risk of pneumothoraxes compared to 5–8 cm H2O, although other procedural differences between hospitals could not be excluded.56 As such, we suggest that CPAP ≤ 15 cm H2O applied within the first minutes after birth improves lung aeration, but does not cause lung over-expansion and does not impede the circulatory transition in preterm lambs and rabbits immediately after birth. However, as it is likely that the risk of adverse events caused by high pressures increases as the lung aerates after birth, it is important to understand when and by how much this pressure can be weaned.
In two of the three 15 cm H2O CPAP groups, CPAP levels were reduced from 15 cm H2O to either 5 or 8 cm H2O when the lungs were visibly aerated. We found that kittens were able to maintain FRC and regular breathing when CPAP levels were reduced to 8 cm H2O, but not when they were reduced to 5 cm H2O. Although FRC and breathing rates were statistically similar between all three 15 cm H2O CPAP groups at the end of the experiment, the 15 to 5 cm H2O group showed a wider interquartile range. Indeed, the low 25th percentile indicates that some of these rabbit kittens were not able to maintain FRC and breathing rates. Thus, CPAP levels of 5 cm H2O may be too low to sustain lung aeration for up to 10 min after birth in some kittens and that 8 cm H2O is more appropriate. This also suggests that CPAP level should be lowered gradually and that the optimal level may need to be tailored to suit the needs of the individual. This is consistent with a previous study suggesting that small and gradual pressure changes may avoid a loss of FRC,25 but the parameters used to guide these reductions are unknown. In preterm lambs, decreasing CPAP from 15 to 8 cm H2O at a median of 13.4 (8.4–20.3) min after birth was found to increase oxygen requirement, which is indicative of FRC loss and suggests that the reduction in CPAP should have been delayed.37 In that study, CPAP was decreased after lambs reached pulmonary blood flows >300 mL/min, oxygen saturations >90% and supplemental oxygen ≤0.7. However, as it is not feasible to assess aeration or other parameters, such as pulmonary blood flow, in the delivery room, these results may not be directly applicable in humans. Nevertheless, they do indicate that CPAP levels should not be based solely on oxygenation status or breathing effort, as these appear to be dependent on, and are not a determinant of, lung aeration. Indeed, we have previously shown that 100% oxygen can increase breathing rates without necessarily improving FRC in preterm rabbits.12 Similarly, the results of this study show that high CPAP levels increase FRC but do not affect breathing rates, and that a small proportion of kittens became apneic even with FRCs of up to 15.5 mL/kg. This indicates that while breathing rates and oxygenation are closely inter-related, they are not a good measure for lung aeration in the delivery room.
In summary, we found that 15 cm H2O CPAP improves lung aeration in spontaneously breathing preterm rabbits. While high CPAP levels (≥12 cm H2O) facilitate spontaneous breathing and reduce the risk of apnoea, CPAP levels do not influence breathing rates. We found no indication that CPAP levels of up to 15 cm H2O causes lung over-expansion, as indicated by bulging of the lung between the rib or increases in the risk of pneumothoraxes or CPAP belly. Once the lungs are aerated, CPAP can be decreased, but future studies are required to determine when to decrease the pressure and by how much in a clinical setting.
References
Morley, C. J. et al. Nasal CPAP or intubation at birth for very preterm infants. N. Engl. J. Med. 358, 700–708 (2008).
Finer, N. N. et al. Early CPAP versus surfactant in extremely preterm infants. N. Engl. J. Med. 362, 1970–1979 (2010).
Trevisanuto, D. et al. Changes over time in delivery room management of extremely low birth weight infants in Italy. Resuscitation 85, 1072–1076 (2014).
Crawshaw, J. R. et al. Laryngeal closure impedes non-invasive ventilation at birth. Arch. Dis. Child. Fetal Neonatal Ed. 103, F112–F119 (2018).
Harding, R., Bocking, A. D. & Sigger, J. N. Upper airway resistances in fetal sheep: the influence of breathing activity. J. Appl. Physiol. 60, 160–165 (1986).
Renolleau, S., Letourneau, P., Niyonsenga, T., Praud, J. P. & Gagne, B. Thyroarytenoid muscle electrical activity during spontaneous apneas in preterm lambs. Am. J. Respir. Crit. Care Med, 159, 1396–1404 (1999).
Moreau-Bussiere, F. et al. Laryngeal response to nasal ventilation in nonsedated newborn lambs. J. Appl. Physiol. 102, 2149–2157 (2007).
van Vonderen, J. J., Hooper, S. B., Hummler, H. D., Lopriore, E. & te Pas, A. B. Effects of a sustained inflation in preterm infants at birth. J. Pediatr. 165, 903–908. e901 (2014).
Dekker, J. et al. Caffeine to improve breathing effort of preterm infants at birth: a randomized controlled trial. Pediatr. Res. 82, 290–296 (2017).
Dekker, J. et al. The effect of initial high vs. low FiO2 on breathing effort in preterm infants at birth: a randomized controlled trial. Front. Pediatr. 7, 504 (2019).
Dekker, J. et al. Repetitive versus standard tactile stimulation of preterm infants at birth—a randomized controlled trial. Resuscitation 127, 37–43 (2018).
Dekker, J. et al. Increasing respiratory effort with 100% oxygen during resuscitation of preterm rabbits at birth. Front. Pediatr. 7, 427 (2019).
Hooper, S. B., Te Pas, A. B. & Kitchen, M. J. Respiratory transition in the newborn: a three-phase process. Arch. Dis. Child Fetal Neonatal Ed. 101, F266–F271 (2016).
Hooper, S. B. et al. Imaging lung aeration and lung liquid clearance at birth. FASEB J. 21, 3329–3337 (2007).
Siew, M. L. et al. Inspiration regulates the rate and temporal pattern of lung liquid clearance and lung aeration at birth. J. Appl. Physiol. (1985) 106, 1888–1895 (2009).
Siew, M. L. et al. The role of lung inflation and sodium transport in airway liquid clearance during lung aeration in newborn rabbits. Pediatr. Res. 73, 443–449 (2013).
Miserocchi, G., Poskurica, B. H., & Del Fabbro, M. Pulmonary interstitial pressure in anesthetized paralyzed newborn rabbits. J. Appl. Physiol. (1985) 77, 2260–2268 (1994).
Siew, M. L. et al. Surfactant increases the uniformity of lung aeration at birth in ventilated preterm rabbits. Pediatr. Res. 70, 50–55 (2011).
Bland, R. D., McMillan, D. D., Bressack, M. A. & Dong, L. Clearance of liquid from lungs of newborn rabbits. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 49, 171–177 (1980).
Kuypers, K. et al. The effect of a face mask for respiratory support on breathing in preterm infants at birth. Resuscitation 144, 178–184 (2019).
O’Donnell, C. P., Kamlin, C. O., Davis, P. G. & Morley, C. J. Crying and breathing by extremely preterm infants immediately after birth. J. Pediatr. 156, 846–847 (2010).
te Pas, A. B. et al. Establishing functional residual capacity at birth: the effect of sustained inflation and positive end-expiratory pressure in a preterm rabbit model. Pediatr. Res. 65, 537–541 (2009).
Siew, M. L. et al. Positive end-expiratory pressure enhances development of a functional residual capacity in preterm rabbits ventilated from birth. J. Appl. Physiol. (1985) 106, 1487–1493 (2009).
te Pas, A. B. et al. Optimizing lung aeration at birth using a sustained inflation and positive pressure ventilation in preterm rabbits. Pediatr. Res. 80, 85–91 (2016).
Kitchen, M. J. et al. Changes in positive end-expiratory pressure alter the distribution of ventilation within the lung immediately after birth in newborn rabbits. PLoS ONE 9, e93391 (2014).
Mulrooney, N. et al. Surfactant and physiologic responses of preterm lambs to continuous positive airway pressure. Am. J. Respir. Crit. Care Med. 171, 488–493 (2005).
Tingay, D. G. et al. Effect of sustained inflation vs. stepwise PEEP strategy at birth on gas exchange and lung mechanics in preterm lambs. Pediatr. Res. 75, 288–294 (2014).
Miedema, M. et al. Effect of nasal continuous and biphasic positive airway pressure on lung volume in preterm infants. J. Pediatr. 162, 691–697 (2013).
Bhatia, R., Davis, P. G. & Tingay, D. G. Regional volume characteristics of the preterm infant receiving first intention continuous positive airway pressure. J. Pediatr. 187, 80–88 (2017). e82.
Richardson, C. P. & Jung, A. L. Effects of continuous positive airway pressure on pulmonary function and blood gases of infants with respiratory distress syndrome. Pediatr. Res. 12, 771–774 (1978).
Magnenant, E. et al. Dynamic behavior of respiratory system during nasal continuous positive airway pressure in spontaneously breathing premature newborn infants. Pediatr. Pulmonol. 37, 485–491 (2004).
te Pas, A. B. et al. Effect of sustained inflation length on establishing functional residual capacity at birth in ventilated premature rabbits. Pediatr. Res. 66, 295–300 (2009).
Kitchen, M. J. et al. A new design for high stability pressure-controlled ventilation for small animal lung imaging. J. Instrum. 5, 1–11 (2010).
Australian Resuscitation Council, N. Z. R. C. ANZCOR Guideline 13.4—Airway Management and Mask Ventilation of the Newborn Infant. https://resus.org.au/guidelines/ (2016).
Leong, A. F., Paganin, D. M., Hooper, S. B., Siew, M. L. & Kitchen, M. J. Measurement of absolute regional lung air volumes from near-field x-ray speckles. Opt. Express 21, 27905–27923 (2013).
te Pas, A. B. et al. Spontaneous breathing patterns of very preterm infants treated with continuous positive airway pressure at birth. Pediatr. Res. 64, 281–285 (2008).
Martherus, T. et al. High-CPAP does not impede cardiovascular changes at birth in preterm sheep. Front. Pediatr. 8, 584138 (2020).
Gluckman, P. D. & Johnston, B. M. Lesions in the upper lateral pons abolish the hypoxic depression of breathing in unanaesthetized fetal lambs in utero. J. Physiol. 382, 373–383 (1987).
Davey, M. G., Moss, T. J., McCrabb, G. J. & Harding, R. Prematurity alters hypoxic and hypercapnic ventilatory responses in developing lambs. Respir. Physiol. 105, 57–67 (1996).
van Henten, T. M. A. et al. Tactile stimulation in the delivery room: do we practice what we preach? Arch. Dis. Child Fetal Neonatal Ed. 104, F661–F662 (2019).
Schmolzer, G. M. et al. Assessment of tidal volume and gas leak during mask ventilation of preterm infants in the delivery room. Arch. Dis. Child Fetal Neonatal Ed. 95, F393–F397 (2010).
Kaufman, J., Schmolzer, G. M., Kamlin, C. O. & Davis, P. G. Mask ventilation of preterm infants in the delivery room. Arch. Dis. Child Fetal Neonatal Ed. 98, F405–F410 (2013).
Schilleman, K. et al. Evaluating manual inflations and breathing during mask ventilation in preterm infants at birth. J. Pediatr. 162, 457–463 (2013).
Dysart, K. C. Physiologic basis for nasal continuous positive airway pressure, heated and humidified high-flow nasal cannula, and nasal ventilation. Clin. Perinatol. 43, 621–631 (2016).
Sankaran, K., Leahy, F. N., Cates, D., MacCallum, M. & Rigatto, H. Effect of lung inflation on ventilation and various phases of the respiratory cycle in preterm infants. Biol. Neonate 40, 160–166 (1981).
Widdicombe, J. G. & Sellick, H. Vagal deflation and inflation reflexes mediated by lung irritant receptors. Q. J. Exp. Physiol. Cogn. Med. Sci. 55, 153–163 (1970).
Haddad, G. G. & Mellins, R. B. The role of airway receptors in the control of respiration in infants: a review. J. Pediatr. 91, 281–286 (1977).
Kuypers, K. et al. Reflexes that impact spontaneous breathing of preterm infants at birth: a narrative review. Arch. Dis. Child Fetal Neonatal Ed. 105, 675–679 (2020).
Probyn, M. E. et al. Positive end expiratory pressure during resuscitation of premature lambs rapidly improves blood gases without adversely affecting arterial pressure. Pediatr. Res. 56, 198–204 (2004).
Polglase, G. R. et al. Positive end-expiratory pressure differentially alters pulmonary hemodynamics and oxygenation in ventilated, very premature lambs. J. Appl Physiol. (1985) 99, 1453–1461 (2005).
Polglase, G. R. et al. Cardiovascular and pulmonary consequences of airway recruitment in preterm lambs. J. Appl Physiol. (1985) 106, 1347–1355 (2009).
Crossley, K. J. et al. Blood gases and pulmonary blood flow during resuscitation of very preterm lambs treated with antenatal betamethasone and/or Curosurf: effect of positive end-expiratory pressure. Pediatr. Res. 62, 37–42 (2007).
Petrillo, F. et al. Pulmonary recruitment strategy in preterm neonates <29 weeks of gestational age to reduce the need for intubation in the delivery room. Am. J. Perinatol. 36, S115–S119 (2019).
Templin, L. et al. A quality improvement initiative to reduce the need for mechanical ventilation in extremely low gestational age neonates. Am. J. Perinatol. 34, 759–764 (2017).
Kanaan, Z. et al. Feasibility of combining two individualized lung recruitment maneuvers at birth for very low gestational age infants: a retrospective cohort study. BMC Pediatr. 20, 144 (2020).
Martherus, T. et al. Comparison of two respiratory support strategies for stabilization of very preterm infants at birth: a matched-pairs analysis. Front. Pediatr. 7, 3 (2019).
Acknowledgements
The authors thank the support provided by the SPring-8 Japan Synchrotron Radiation Research Institute, which was provided by the SPring-8 Program Review Committee (2016A0132), and gratefully acknowledge the expert assistance of Kentaro Uesugi, Naoto Yagi, Masato Hoshino and Hiroyuki Iwamoto for assistance to conduct our experiments at SPring-8. This experiment was supported by the National Health and Medical Research Council (NHMRC) Program Grant (606789), NHMRC Research Fellowships (SH: APP1058537) and the Victorian Government’s Operational Infrastructure Support Program. A.B.t.P. is recipient of an NWO innovational research incentives scheme (VIDI 91716428). E.V.M. was supported by a Monash University Postdoctoral Fellowship (BPF17-0066) and a NHMRC Peter Doherty Biomedical Early Career Fellowship (APP1138049). M.J.K. is a recipient of ARC Future Fellowship (FT160100454). We acknowledge travel funding provided by the International Synchrotron Access Program (ISAP) managed by the Australian Synchrotron and funded by the Australian Government (AS/IA173/12909 and ISP12221).
Author information
Authors and Affiliations
Contributions
All authors included in this paper fulfil the criteria of authorship. T.M., K.J.C., E.V.M., A.B.t.P. and S.B.H. made substantial contributions to the design of the experiment. All authors were involved in performing the experiment and obtaining data. T.M., M.K.C., M.J.K., A.B.t.P. and S.B.H. were responsible for data analysis and interpretation. T.M., A.B.t.P. and S.B.H. drafted the first version of the manuscript, after which all authors provided feedback and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martherus, T., Croughan, M.K., Crossley, K.J. et al. Higher CPAP levels improve functional residual capacity at birth in preterm rabbits. Pediatr Res 91, 1686–1694 (2022). https://doi.org/10.1038/s41390-021-01647-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01647-8