Abstract
Background
Necrotizing enterocolitis (NEC), a severe gut disorder in preterm infants, is difficult to predict due to poor specificity and sensitivity of clinical signs and biomarkers. Using preterm piglets as a model, we hypothesized that early development of NEC affects blood gene expression, potentially related to early systemic immune responses.
Methods
A retrospective analysis of clinical, tissue, and blood data was performed on 129 formula-fed piglets with NEC diagnosis at necropsy on day 5. Subgroups of NEC (n = 20) and control piglets (CON, n = 19) were analyzed for whole-blood transcriptome.
Results
Preterm piglets had variable NEC lesions, especially in the colon region, without severe clinical signs (e.g. normal growth, activity, hematology, digestion, few piglets with bloody stools). Transcriptome analysis showed 344 differentially expressed genes (DEGs) between NEC and CON piglets. Validation experiment showed that AOAH, ARG2, FKBP5, PAK2, and STAT3 were among the genes affected by severe lesions on day 5, when analyzed in whole blood and in dried blood spots (DBS).
Conclusion
Whole-blood gene expressions may be affected in preterm pigs before clinical signs of NEC get severe. Blood gene expression analysis, potentially using DBS samples, is a novel tool to help identify new early biomarkers of NEC.
Impact
-
Preterm pig model was used to investigate if blood transcriptomics could be used to identify new early blood biomarkers of NEC progression.
-
Whole-blood transcriptome revealed upregulation of target genes in NEC cases when clinical symptoms are subtle, and mainly colon regions were affected.
-
Differential NEC-associated gene expressions could be detected also in dried blood spots, potentially allowing easy collection of small blood volumes in infants.
Similar content being viewed by others
Introduction
Every year, 15 million infants are born preterm (<37 weeks gestation). About 5–10% of preterm infants with very low birth weight (<1500 g) are affected by necrotizing enterocolitis (NEC), a severe intestinal disease with high mortality.1 NEC develops rapidly and unpredictably during the first weeks after preterm birth and often leads to sepsis. Currently, NEC diagnosis relies on a combination of clinical symptoms, including bowel obstruction, abdominal distention, pain and discoloration, bloody stools, and radiological signs. Patients with suspected NEC are initially treated with broad-spectrum antibiotics and enteral feeding restriction. If clear symptoms develop, up to 50% of infants will require surgical intervention to remove the necrotic parts of the intestine.2 However, lack of sensitive and specific early diagnostic markers of NEC limits timely intervention, and 12–36% of patients die after NEC surgery.3,4 Therefore, there is a great need to identify biomarkers that can assist early diagnosis or help to predict the severity of NEC lesions.
Previous studies have identified non-specific systemic biomarkers of NEC, which are inflammation mediators, such as acute phase proteins, cytokines, chemokines, and cell surface antigens. A major drawback of these biomarkers would be their inability to differentiate NEC from sepsis or inflammatory states not originating from the gut.5 Fecal proteins related to gut inflammation (e.g. calprotectin, S100A12) are more indicative of intestinal injury, but adequate and timely stool samples can be difficult to collect. Some proteins that are released by damaged intestinal tissue into the bloodstream (e.g. L-FABP, I-FABP, and TFF-3) are increased in surgical NEC cases.6 These may provide vital information for identifying infants who need surgery, although they are unlikely to be useful for predicting early and mild NEC cases. A recent study showed that a resistin-like molecule β (RELMβ), which is important for gut barrier function and regulates local immunity, was elevated in suspected NEC cases.7 Recent advances in multi-omic technologies have revolutionized the potential to identify early biomarkers of many diseases, including NEC.8 Combined microbiome and metabolome analysis of fecal samples show that firmicute dysbiosis, together with the urinary alanine-to-histidine ratio, can be used as NEC biomarkers9 but optimal fecal sampling and fast analyses remain challenging.
Numerous studies have been done to investigate the mechanisms of NEC development but it is difficult to differentiate between the tissue and blood factors that associate with gut NEC lesions, and the causes and consequences of NEC. Regardless, there is no doubt that NEC development is closely related to immune responses both in the gut and blood, at least for severe cases. On the intestinal side, uncontrolled activation of the receptor for Gram-negative bacteria, TLR4, has been suggested to be a critical contributor to NEC.10 However, cause–effects relationships are unclear, especially when extrapolating from animal models to infants. In young mice, TLR4 activation affects epithelial integrity by increasing enterocyte apoptosis and controlling enterocytes proliferation and migration,11 which in turn allows pathogens to enter the circulation resulting in systemic inflammation. TLR4 activation may also mediate lymphocyte influx into tissues, leading to an induction of Th17 cells and a reduction in Treg cells. Release of the inflammatory cytokine IL-17 by Th17 cells causes mucosal injury by impairment of tight junctions during NEC.12 Characterizing NEC-associated gene expression changes in blood collected during NEC progression may help to identify early biomarkers, despite the difficulties in separating gut-specific effects from systemic gut-independent factors. Systemic responses may also differ between lesions in different parts of the gut (intestine, colon).
Blood samples remain the most easily accessible biofluid from patients in hospitals but for fragile, small preterm infants it remains challenging to preserve blood volume and avoid removing too much blood for analyses. Earlier studies on blood miRNA expression showed that plasma miR-1290 was specific to NEC, thus helping to differentiate NEC from sepsis or other inflammatory conditions.13 Dried blot spots (DBS) have been routinely used for decades to detect inborn errors of metabolism (metabolites by chromatographic techniques, e.g. phenylketonuria, PKU) in both preterm and term newborn infants, using only 80 µL of whole blood dried on filter paper. Recently, it has been suggested that such DBS samples could be used for whole blood gene expression analyses to better understand systemic inflammatory conditions.14 Partly related to the low incidence of NEC, and the challenge in performing fast analyses of such infant blood samples or DBS, these potentials are yet to be explored and validation studies in appropriate animal models are required.
Preterm piglets (90% gestation) are valuable biomedical models due to their similarity with preterm infants in size, anatomy, physiology, and many clinical conditions.15 They are sensitive to systemic infection and spontaneously develop NEC after formula feeding, especially in the first 1–2 weeks of life,16,17 and they show clinical symptoms such as lethargy, bloody stools and abdominal distension and discoloration that require discontinuation of feeding and antibiotics treatment to avoid NEC progression. Mild NEC cases often show lesions exclusively in the colon region while in more severe cases the small intestine is usually affected, with more robust clinical signs18 and damage to the developing brain.19 Using preterm piglets as a highly NEC-sensitive model of preterm infants, we hypothesized that early NEC development affects expression of blood genes, reflecting an early systemic immune responses. Thus, we aimed to characterize the whole blood transcriptome in preterm piglets with and without signs of NEC progression after the first few days of life. Key genes expression changes were validated in both whole blood and DBS by a more rapid tool, quantitative PCR (qPCR), to further investigate if specific blood gene expression changes in DBS samples could be a future tool for early NEC diagnosis.
Materials and methods
Animal experimental procedure
All animals used in this study originated from four previous animal experiments, including two published studies20,21 and two unpublished studies, where animal procedures were approved by the Danish National Committee on Animal Experimentation. One hundred and twenty-nine piglets from eight sows (Danish Landrace × Large White × Duroc) were delivered in these four experiments by cesarean section at preterm (day 106, 90% of gestation) and kept until day 5 of life. Immediately after cesarean section, piglets were transferred to our piglet neonatal intensive care unit, fitted with orogastric and umbilical arterial catheters, and reared in individual incubators. The piglets received parenteral nutrition (2–4 mL/kg/h) plus a gradually increasing amount of enteral nutrition with infant formula (24–120 mL/kg/day) for 5 days to predispose them to NEC development. Depending on the study design of the four experiments, the milk formula diet was either commercially available infant formula or prepared by blending commercially available infant formula ingredients, providing varying nutrient (15–73 g/L protein, 42–65 g/L carbohydrate, and 35–56 g/L fat), variable lactose-to-maltodextrin ratio, and energy densities (2730–3990 kJ/L). Piglets were weighed once daily and clinically assessed twice daily. Feces were scored according to following criteria: 1 = firm feces, 2 = pasty feces, 3 = droplets of watery feces/diarrhea, 4 = moderate diarrhea, 5 = intense diarrhea. The presence of bloody diarrhea and/or abdominal distension was recorded. Physical activity of each pig was recorded by an infrared video surveillance camera and proportion of active time within each hour recorded.22 On day 5, intestinal permeability was measured by the lactulose–mannitol technique shortly before euthanasia.23 Blood samples were collected by cardiac puncture at the time of euthanasia and immediately transferred into EDTA tubes for later hematology analysis. Plasma were analyzed for tumor necrosis factor-α (TNFα) by enzyme-linked immunosorbent assay (ELISA, R&D Systems, Abingdon, UK).
At necropsy, the entire small intestine was evenly divided into three regions (proximal, middle, and distal intestine) and NEC was evaluated in both small intestine and colon according to a macroscopic NEC scoring system (for pictures, see Fig. 1 and refs. 18,24) 1 = absence of lesions, 2 = local hyperemia, 3 = hyperemia, extensive edema, and local hemorrhage, 4 = extensive hemorrhage, 5 = local necrosis and/or pneumatosis intestinalis, 6 = extensive transmural necrosis and/or pneumatosis intestinalis. Piglets with a score ≥3 in any of the intestinal regions (including small intestine and colon) were diagnosed as “NEC”. Piglets with scores 3–4 in any intestinal or colon region were categorized as suffering from “mild NEC lesions” while those having scores 5–6 in any region were categorized as “severe NEC lesions”. The 129 piglets that survived until day 5 from all four experiments were used for retrospective analysis of their clinical data, and colon tissues from 79 piglets in two experiments were collected for analysis of cytokine (IL-1b and IL-8) levels as well as mucin-containing goblet cells density as previously described.20 A further 20 NEC piglets (NEC) and 20 litter-mate healthy controls (CON) were randomly selected from six sows as a discovery cohort and were used for the transcriptome analysis. Forty-one piglets from the other two sows were used as a validation cohort to perform blood qPCR analyses.
Photographs of small intestine and colon are presented in left and right panels, respectively. According to macroscopic NEC scoring system (1 = absence of lesions, 2 = local hyperemia, 3 = hyperemia, extensive edema and local hemorrhage, 4 = extensive hemorrhage, 5 = local necrosis and/or pneumatosis intestinalis, 6 = extensive transmural necrosis and/or pneumatosis intestinalis), piglets with a score ≥3 in any of the intestinal regions (including small intestine and colon) were diagnosed as “NEC”. Piglets with scores 3–4 in any intestinal or colon region were categorized as “mild NEC” cases, while those with scores 5–6 in any region were categorized as “severe NEC” cases.
Transcriptome analysis
Blood samples from the discovery cohort were collected by cardiac puncture at euthanasia and 50 µL of whole blood was stored in a lysis/binding solution (MagMax 96 blood RNA isolation kit, Thermo Fisher, Waltham, MA) at −20 °C. Total blood RNA was extracted using MagMax 96 blood RNA isolation kit according to the manufacturer’s instructions, no more than 6 months after storage. RNA-seq libraries were constructed using 500 ng RNA and VAHTS mRNA-seq V3 Library Prep Kit for Illumina (Vazyme, China). The libraries were sequenced on the Illumina Hiseq X Ten platform (Illumina, San Diego, California) to generate 150 bp paired-end reads. Quality and adapter trimming of raw reads were performed using TrimGalore (Babraham Binoinformatics, UK). The remaining clean reads (~26M per sample) were aligned to the porcine genome (Sscrofa11.1) using Tophat2.25 The annotated gene information of porcine genome was obtained from Ensembl (release 91). The script htseq-count26 was used to generate gene count matrix, followed by gene-level expression analyses using DESeq2.27
qPCR analyses
Blood samples from the validation cohort were collected by cardiac puncture at euthanasia and stored by two methods for up to 1 year before analysis: (1) stored as whole blood (WB) in the lysis/binding solution as described above and (2) stored as dried blood spots (DBS). For both storage methods, 50 µL of whole blood was used. For the DBS sample, blood was spotted onto a filter paper (Statens Serum Institut, Denmark) using a pipette, and was air-dried at room temperature for about 3 h before storage at −20 °C. Total blood RNA from the first storage method was extracted using MagMax 96 blood RNA isolation kit, according to the manufacturer’s instructions. Total blood RNA from DBS was extracted using Monarch Total RNA Miniprep Kit (New England Biolabs, Ipswich, MA) with a modified protocol. Briefly, one full DBS was cut into small pieces and incubated in 600 µL 1× DNA/RNA protection reagent at room temperature. During incubation, the DBS sample was homogenized by continuous vortexing with a stainless steel bead (Sigma-Aldrich, # Z763829, St. Louis, MO) for 15 min, followed by Prot K reaction at 55 °C for 30 min. The supernatant was collected using Qiashredder (Qiagen, Germany) by centrifugation at 10,000g for 2 min and RNA was extracted following the rest of protocol.
Blood RNA after extraction was quantified using a NanoDrop 1000 spectrophotometer (Thermo Fisher, Waltham, MA). For WB and DBS samples, 500 and 50 ng RNA were converted into cDNA, respectively, using High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher, Waltham, MA). qPCR was performed using LightCycler 480 SYBR Green I Master kit (Roche, Switzerland) on LightCycler 480 (Roche, Switzerland) and results were analyzed according to the double delta Ct method. Relative expression of target genes was normalized to the housekeeping gene HPRT1. All primers were designed using Primer-Blast28 and the sequences of primers are listed in Supplementary Table S1.
Statistical analysis
All data were analyzed in the software R (version 4.0.2). For clinical outcomes, continuous variables (birth weight, daily weight gain, physical activity, gut permeability, gastric residuals, hematology data, cytokines, and goblet cells density) were analyzed using linear models with lm() function. Ordered categorical outcomes (NEC severity scores) were analyzed using the ordinal regression model with clm() function from package ordinal. These models were adjusted for litter, diet, and sex, followed by post hoc Tukey’s test for pairwise comparison between groups. Categorical variables (sex, presence of diarrhea, bloody stool, and abdominal distension) were analyzed using Fisher’s exact test. For qPCR analysis, comparison between two groups was made using t-test. A P value of <0.05 was considered statistically significant, and a P value <0.10 was considered a tendency to an effect. Transcriptome data were analyzed by negative binomial generalized linear model in DESeq2, where model was adjusted for litter and diet. Significant differentially expressed genes (DEGs) between NEC and CON groups were identified by DESeq2 using Benjamini–Hochberg (BH)-adjusted P value, with <0.1 as cut-off. Correlation between gene expression was performed using Spearman’s rank correlation based on normalized counts produced from DESeq2, and the correlation with absolute spearman rho >0.6 as well as BH-adjusted P value <0.05 was considered statistically significant. Gene ontology and KEGG pathway enrichment analysis were performed using DAVID29 and a BH-adjusted P value of <0.05 was considered statistically significant.
Results
Clinical outcomes
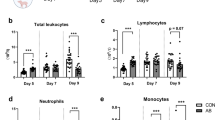
A total of 129 preterm piglets from eight sows were euthanized on postnatal day 5 for NEC diagnosis and 74 was diagnosed as NEC and 55 as healthy controls (CON). According to NEC severity (defined as the maximum NEC score among all intestinal regions), the 74 NEC piglets included 49 mild (score 3–4) and 25 severe cases (score 5–6, Fig. 1). Macroscopic NEC lesions were found primarily in the colon (n = 64), rather than small intestine (n = 10, 6, and 16 for proximal, middle, and distal intestine, respectively). Consistently, severity score for the colon and distal small intestine, but not proximal and middle small intestine, was significantly higher for NEC, especially severe NEC, relative to CON piglets (Table 1). As NEC lesions occurred primarily in the colon, cytokines (IL-1b and IL-8) levels in the colon were analyzed. Results showed significant increase of IL-1b and IL-8 in NEC, especially severe NEC piglets (Table 1), and these cytokine levels were positively correlated with NEC scores in the colon (spearman rho = 0.61 and 0.54 for IL-1b and IL-8, both P < 0.05). Moreover, reduced goblet cells in the colon were observed in severe NEC (P < 0.05) and mild NEC piglets (P < 0.1, Table 1). The density of goblet cells was negatively correlated with colon NEC scores (spearman rho = −0.51, P < 0.05). Clinical outcomes of all 129 preterm piglets are summarized in Table 1. The average birth weight of preterm piglets was 1017 g and was similar for NEC and CON groups. During the first 3 days, diarrhea (feces score >2) was observed only in few piglets (up to 6 per group). On day 4 and 5, 67 and 90 out of 129 piglets had diarrhea, but the overall incidence of diarrhea during the first 5 days was similar among groups (75–88%). Bloody stool was observed in 14 NEC piglets but absent in CON piglets (P < 0.05). Most piglets that had bloody stools were later diagnosed with severe NEC (12/14, only two piglets with mild NEC lesions had also bloody stool). Three NEC piglets and four CON piglets showed abdominal distention (P > 0.05), the remaining piglets did not show such signs. By day 5, NEC and CON piglets showed similar growth rates (14 ± 1 g/day) and physical activity, as detected by surveillance camera (16.0% active time per hour), supporting that the NEC lesions observed at autopsy had not yet affected the piglet clinical condition notably. At the time of euthanasia, the three groups of piglets had similar gut permeability, gastric residual volume, plasma TNFα level and hematology results, except for increased neutrophils and decreased lymphocytes in severe NEC pigs (both P < 0.05, Table 1). In summary, limited clear clinical NEC symptoms were evident prior to the time of autopsy, except in the 48% of severe NEC piglets showing bloody stool. Mild NEC piglets could not be differentiated from CON piglets by their clinical conditions or blood values (Table 1).
Blood transcriptome reveals NEC-associated DEGs
To examine whether whole blood gene expressions changed during the pre-clinical NEC stages, blood samples were collected at euthanasia and 40 piglets from six sows were randomly selected for RNA-seq as a discovery cohort. One sample failed its RNA-sequencing, resulting in 39 transcriptome data (20 for NEC and 19 for CON). Of 25,880 genes annotated in the Ensembl database (Sscrofa11.1, release 91), 18,894 of the genes were detected in at least one pig. Based on the individual expression of these genes, principal component analysis (PCA) showed no clear separation between NEC and CON groups (Fig. 2a). To identify DEGs between the two groups, a threshold of adjusted P < 0.1 was used. This resulted in 344 DEGs with ascertainable gene symbols, including 158 and 186 DEGs that were up- and down-regulated in NEC, and equivalent to 1.8% of analyzed genes (Fig. 2b and Supplementary Table S2). The results suggest that whole-blood gene expression is not markedly affected at early (mild) stage of NEC. A detailed look at the relationship between DEGs and NEC severity was investigated partly in the 20 NEC cases in our discovery cohort (11 mild + 9 severe NEC cases). By comparing these two subgroups to CON piglets, we found that only 8 out of the 344 DEGs showed significant difference between mild NEC and CON groups, while the majority of DEGs (70%) were significantly altered by severe NEC. Therefore, changes in whole-blood gene expressions were mainly associated with severe NEC lesions, less with mild NEC lesions, according to our score system.
a Principal component analysis (PCA) was performed based on the individual expression level of all analyzed genes. Scores of first two principle components from PCA are plotted. b Volcano plot illustrating the DEGs between NEC and CON group. c Barplot showing significantly enriched KEGG pathways. d Heatmap illustrating co-occurrence of DEGs and NEC-related keywords in literature identified on PubMed. Black and gray colors indicate for presence and absence of co-occurrence, respectively. EA epithelial apoptosis, II intestinal inflammation, IBD inflammatory bowel disease, CD Crohn’s disease, UC ulcerative colitis. e Putative co-expression network, where each node represents a gene and each edge represents a significant correlation between gene pairs. Top 10 hub genes are labeled. f Heatmap showing relative expression level of the top 10 hub genes between NEC and CON groups. g Boxplot of targeted DEGs that were selected for validation.
To understand the functional significance of these NEC-associated DEGs, KEGG pathway enrichment analysis was performed according to DAVID database. This resulted in six significant pathways (Fig. 2c, FDR < 0.05), including “T cell receptor signaling pathway”, “Chemokine signaling pathway”, “Endometrial cancer”, “Ras signaling pathway”, “Signaling pathways regulating pluripotency of stem cells”, and “Natural killer cell mediated cytotoxicity”. Next, to explore whether any of the DEGs might play a role in NEC development, a subsequent PubMed literature search was performed. We defined 10 NEC-related keywords, including NEC, colitis, necrotic, hemorrhage, pneumatosis, epithelial apoptosis, intestinal inflammation, inflammatory bowel disease (IBD), Crohn’s disease, and ulcerative colitis. Then for each DEG, we searched PubMed record using the “Text Word” field tag to identify co-occurrence of keywords and genes. Result showed no DEGs co-occurred with pneumatosis but revealed 123 DEGs that co-occurred with at least one of the other 9 keywords (Fig. 2d). Moreover, we sought to characterize the relationships among all DEGs. To do this, pairwise correlation was performed to determine possible co-expressed gene pairs.30 A total of 6830 out of 58,996 gene pairs having absolute Spearman rho >0.6 and FDR < 0.05 were selected to conduct a putative co-expression gene network (Fig. 2e). Among the top 10 hub genes (Fig. 2f) that had the highest number of connection to other genes, ATP6V1A, FOXN2, PAK2, ZAP70, and ZEB2 were found in PubMed record and related to hemorrhage, IBD, or colitis.31,32,33,34,35 Finally, 10 DEGs including PAK2 and 9 DEGs (AOAH, ARG2, FKBP5, GSK3B, PTGS1, SP1, STAT3, TGFB1, and TOLLIP) that co-occurred with NEC and other keywords in PubMed literature were selected for validation (Fig. 2g).
Validation of NEC-associated DEGs in whole blood and DBS
To validate the selected NEC-associated DEGs, 41 piglets delivered from two separate sows were used as validation cohort. This included 13 CON and 28 NEC piglets (incl. 22 mild and 6 severe NEC cases). We first examined the expression of 10 selected DEGs in whole blood using qPCR. As a result, five genes (AOAH, ARG2, FKBP5, PAK2, and STAT3) were increased in expression in severe NEC cases, relative to expression in mild NEC cases or CON piglets (Fig. 3a). When combining both mild and severe NEC cases into one NEC group, none of the selected DEGs showed significant differential expression between NEC and CON.
a Expression of target DEGs in validation piglet cohort. Animals were classified into three groups according to their NEC score: CON (scores 1–2, n = 13), mild (scores 3–4, n = 22), and severe (scores 5–6, n = 6). Data are presented as means ± SEMs. Comparison between two groups was performed using t-test (*P < 0.05, **P < 0.01, #P < 0.1). WB whole blood, DBS dried blood spots. b Correlation of gene expression between whole blood and DBS is shown in scatterplot with y-axis on the right. Expression of target genes in whole blood is shown in bar plots with y-axis on the left.
We next evaluated whether the expression pattern of these NEC-associated DEGs remained detectable in DBS, thus providing evidence for developing NEC biomarkers based on infant DBS samples. We found that an average of 1.6 µg total RNA could be extracted using 50 µL of whole blood, while DBS containing the same amount of blood revealed an average of 336 ng total RNA, equivalent to 21% RNA amount in the whole blood. Nevertheless, qPCR quantification showed that the five target genes (AOAH, ARG2, FKBP5, PAK2, and STAT3) in DBS were consistently increased in severe NEC cases (Fig. 3a). The expression levels of these genes in DBS were well correlated with those in whole blood (Fig. 3b) with expression levels for four genes (AOAH, ARG2, FKBP5, STAT3) having a Pearson’s R > 0.94. The PAK2 gene had the lowest Pearson’s R (0.58) for the whole blood to DBS comparison, but also the lowest expression level among the five genes (Fig. 3b). Moreover, expression level of ARG2 and STAT3, but not AOAH, FKBP5, and PAK2, were positively correlated with neutrophil-to-lymphocyte ratio (P < 0.05), likely associated with systemic inflammatory status.
Discussion
Blood remains the most readily available biofluid from patients for biochemical analyses to support disease diagnosis and treatment, including NEC diagnosis and treatment in preterm infants. In this proof-of-concept study, we used preterm piglets to investigate if the whole blood transcriptome could be used to identify new putative NEC biomarkers, especially markers that appear before NEC symptoms are clinically evident. In preterm pigs, NEC lesions affect all regions of the gut (“NEC totalis”) but often first appear in the colon region, then in more severe cases also the small intestine, especially the distal parts. Clinical symptoms and the developing brain are most affected when the small intestine is affected.18,19 Our previous studies indicate that some of milder colon lesions may undergo spontaneous repair after day 5.36 While the age- and region-dependent NEC development may differ between pigs and infants, the predisposing factors and mechanism leading to local and systemic effects may remain the same.
In the retrospective analysis, bloody stool was the only clinical symptom that predicted NEC lesions at autopsy on day 5. However, isolated rectal bleeding is not specific to NEC and could be due to anatomical causes (e.g. strictures), other enteric infections, or immunological responses related to immaturity or allergies.37,38 Thus at this early stage, NEC is suspected and can only be confirmed by visual tissue inspection at necropsy. Consistent with our previous study,39 piglets at this stage and with relatively mild feeding progression, also show tissue inflammation but limited evidence of systemic inflammation, supporting the need to look for blood biomarkers that may be more sensitive. The whole-blood transcriptome analysis revealed hundreds of DEGs that were associated with severe NEC, according to our scoring system (see Fig. 1 and refs, 18,24) despite that such lesions had not yet induced any clear clinical symptoms in the animals (similar to advanced Bell stages for preterm infants.40) The identified NEC-associated DEGs were detectable in both whole blood and DBS. Our results suggest a potential to use the blood transcriptome, potentially derived from DBS samples, to develop new early biomarkers for infants with unclear clinical NEC symptoms. Such biomarkers will help to avoid surgery on infants who can be treated medically, and avoid delays in surgical intervention for those that need this for recovery. Blood genes relevant as NEC biomarkers may differ according to many factors, including prenatal inflammatory stimuli (chorioamnionitis) and older age at NEC onset, as indicated by our other blood transcriptome studies in preterm pigs.41,42 Following such prenatal immune priming or extended periods of NEC stimuli after birth, blood gene expression changes may differ from those in the pre-NEC stages, resulting in systemic immune suppression. We acknowledge the challenges in direct translation between preterm pigs and infants, yet the spontaneous preterm pig NEC model is an excellent tool to provide proof of concept for new ways to understand the complex interaction between NEC and systemic factors in preterm infants.
In preterm pigs, three genes AOAH, FKBP5, and PAK2 were of particular interest because they were confirmed to increase in expression in severe NEC cases, likely independent of systemic infections, as confirmed by our ex vivo blood stimulation experiments (unpublished study). The expression of these three genes were highest in the two pigs with most severe NEC lesions (score 6 in both the small intestine and colon, reflecting extensive hemorrhage and necrotic lesions). Both these piglets had bloody stools after 4 days of life, but clinical record and hematology results could not differentiate them from other animals with or without NEC at autopsy. Thus, NEC-associated DEGs may be used to indicate NEC severity and may supplement other clinical parameters. Whether the same blood genes could be NEC sensitive in infants remains to be shown.
Blood biomarkers of diseases that is located to specific organs (e.g. the gut in the case of NEC) would most often reflect a consequence, rather than a cause, of the disease. Nevertheless, some of our target genes warrant further investigation with regards to their specific roles in NEC pathogenesis. It has been hypothesized that TLR4 activation plays a crucial role in NEC development.43 Rodent experimental models have shown that TLR4-mediated Th17 lymphocyte influx, whereby release of IL-17 disrupts the intestinal barrier, leading to NEC. This process is dependent on STAT3, which drives Th17 differentiation.12 Upon activation, lymphocytes in the mucosal immune system travel through mesenteric lymph nodes and thoracic duct, from where they circulate in the blood before reentering mucosal tissues. Thus, our observation of increased STAT3 in the whole blood in piglets with severe NEC lesions may reflect pathogenic lymphocyte influx to the gut during the early phase of NEC that initially activates immune responses. Moreover, one of our detected genes, PAK2, was identified as a hub gene among all NEC-associated DEGs. This gene was suggested as a driver of colitis in a recent study of IBD, where multi-omics data from mouse and human biopsies were used to generate this hypothesis.35 Both PAK2 and STAT3 have been suggested as key genes of IBD and inhibition of PAK signaling resolves pathological bleeding and restores normal epithelial crypt morphology in IBD mice models.35 Whether PAK2 also drives NEC development or whether targeting PAK signaling protects against NEC remains to be shown.
Another gene that increased in pigs with severe NEC lesions was ARG2, for a gene encoding for arginase 2, a catabolizing enzyme of arginine. It has been shown that low arginine availability in the immature intestine is a risk factor for NEC, likely due to the result of poor intestinal perfusion.44 Clinical trials in preterm infants also showed that arginine supplementation reduced the incidence of NEC.45 Finally, FKBP5 encodes for FK506 binding protein 5, which is a regulator of the glucocorticoid receptor (GR). Overexpression of FKBP5 is known to cause glucocorticoid resistance, either by reducing affinity of GR for glucocorticoids or by reducing nuclear translocation and activation of GR itself.46,47 As glucocorticoids are potent inhibitors of the immune system, increased FKBP5 in severe NEC cases may be related to inappropriate immune response.
In summary, we have demonstrated that in preterm piglets, blood gene expression is indeed altered by early-stage NEC lesions. Differential expression of genes may reflect different NEC severities in different gut regions, and possibly different systemic immunological effects in relation to NEC progression. In preterm pigs, NEC severity scores are based on visible gut lesions at tissue autopsy.18,24 This scoring is not directly comparable to the clinical/radiographic symptoms of mild or definitive NEC in infants (early and late Bell stages). We cannot exclude that blood transcriptomic effects of NEC differ between infants and pigs, and it is important to demonstrate if similar NEC-related blood transcriptomic signatures can be found in infants. Given that we defined “NEC” using our macroscopic scoring system, it is unclear to which extent the NEC-associated blood gene expression changes correlate closely with histopathological changes in the intestinal and colonic tissue, although previous studies demonstrated extensive loss of villi in piglets with severe NEC.48,49 Expressions of candidate genes could be investigated in human infants with NEC and evaluated for potential use as early NEC biomarkers to help decision making in clinical neonatology. Blood transcriptome is a high-throughput tool to screen for novel biomarkers and validated biomarkers should be measured by more rapid techniques (e.g., qPCR) to provide timely information in clinical care. Considering the extended stability of mRNA stored as DBS,50 both acute DBS samples (at suspected NEC), as well as archived neonatal DBS (already collected for other reasons), could be used for developing diagnostic and prognostic biomarkers of NEC. Further studies are required in both piglets and infants to understand how blood gene expressions are affected by development of NEC lesions in different regions of the gut, interacting with many pre- and postnatal factors, and this information should be integrated with other blood omics analyses (e.g. genomics, metabolomics, proteomics) as well as results from conventional blood analyses.
Data availability
All sequencing and processed data are deposited in the Gene Expression Omnibus (GEO) with accession number GSE166152.
References
Patel, R. M. et al. Causes and timing of death in extremely premature infants from 2000 through 2011. N. Engl. J. Med. 372, 331–340 (2015).
D’Angelo, G. et al. Current status of laboratory and imaging diagnosis of neonatal necrotizing enterocolitis. Ital. J. Pediatr. 44, 84 (2018).
Juhl, S. M., Gregersen, R., Lange, T. & Greisen, G. Incidence and risk of necrotizing enterocolitis in Denmark from 1994–2014. PLoS ONE 14, e0219268 (2019).
Luig, M., Lui, K., Nsw & Group, A. N. Epidemiology of necrotizing enterocolitis—Part I: Changing regional trends in extremely preterm infants over 14 years. J. Paediatr. Child Health 41, 169–173 (2005).
Ng, P. C., Ma, T. P. & Lam, H. S. The use of laboratory biomarkers for surveillance, diagnosis and prediction of clinical outcomes in neonatal sepsis and necrotising enterocolitis. Arch. Dis. Child Fetal Neonatal Ed. 100, F448–F452 (2015).
Ng, E. W. et al. Gut-associated biomarkers L-FABP, I-FABP, and TFF3 and LIT score for diagnosis of surgical necrotizing enterocolitis in preterm infants. Ann. Surg. 258, 1111–1118 (2013).
Luo, J., Li, H. P., Xu, F., Wu, B. Q. & Lin, H. C. Early diagnosis of necrotizing enterocolitis by plasma RELMbeta and thrombocytopenia in preterm infants: a pilot study. Pediatr. Neonatol. 60, 447–452 (2019).
Agakidou, E., Agakidis, C., Gika, H. & Sarafidis, K. Emerging biomarkers for prediction and early diagnosis of necrotizing enterocolitis in the era of metabolomics and proteomics. Front. Pediatr. 8, 602255 (2020).
Morrow, A. L. et al. Early microbial and metabolomic signatures predict later onset of necrotizing enterocolitis in preterm infants. Microbiome 1, 13 (2013).
Leaphart, C. L. et al. A critical role for TLR4 in the pathogenesis of necrotizing enterocolitis by modulating intestinal injury and repair. J. Immunol. 179, 4808–4820 (2007).
Sodhi, C. P. et al. Toll-like receptor-4 inhibits enterocyte proliferation via impaired beta-catenin signaling in necrotizing enterocolitis. Gastroenterology 138, 185–196 (2010).
Egan, C. E. et al. Toll-like receptor 4-mediated lymphocyte influx induces neonatal necrotizing enterocolitis. J. Clin. Invest. 126, 495–508 (2016).
Ng, P. C. et al. Plasma miR-1290 is a novel and specific biomarker for early diagnosis of necrotizing enterocolitis-biomarker discovery with prospective cohort evaluation. J. Pediatr. 205, 83–90. e10 (2019).
Grauholm, J. et al. Gene expression profiling of archived dried blood spot samples from the Danish Neonatal Screening Biobank. Mol. Genet. Metab. 116, 119–124 (2015).
Sangild, P. T. et al. Invited review: the preterm pig as a model in pediatric gastroenterology. J. Anim. Sci. 91, 4713–4729 (2013).
Ren, S. et al. Neonatal gut and immune maturation is determined more by postnatal age than by postconceptional age in moderately preterm pigs. Am. J. Physiol. Gastrointest. Liver Physiol. 315, G855–G867 (2018).
Baek, O. et al. Diet modulates the high sensitivity to systemic infection in newborn preterm pigs. Front. Immunol. 11, 1019 (2020).
Cao, M. et al. Physical activity and gastric residuals as biomarkers for region-specific NEC lesions in preterm neonates. Neonatology 110, 241–247 (2016).
Sun, J. et al. Necrotizing enterocolitis is associated with acute brain responses in preterm pigs. J. Neuroinflamm. 15, 180 (2018).
Nguyen, D. N. et al. Prenatal intra-amniotic endotoxin induces fetal gut and lung immune responses and postnatal systemic inflammation in preterm pigs. Am. J. Pathol. 188, 2629–2643 (2018).
Holgersen, K. et al. Supplemental insulin-like growth factor-1 and necrotizing enterocolitis in preterm pigs. Front. Pediatr. 8, 602047 (2020).
Cao, M. et al. Physical activity level is impaired and diet dependent in preterm newborn pigs. Pediatr. Res. 78, 137–144 (2015).
Thymann, T. et al. Formula-feeding reduces lactose digestive capacity in neonatal pigs. Br. J. Nutr. 95, 1075–1081 (2006).
Stoy, A. C. F. et al. Increased intestinal inflammation and digestive dysfunction in preterm pigs with severe necrotizing enterocolitis. Neonatology 111, 289–296 (2017).
Kim, D. et al. TopHat2: accurate alignment of transcriptomes in the presence of insertions, deletions and gene fusions. Genome Biol. 14, R36 (2013).
Anders, S., Pyl, P. T. & Huber, W. HTSeq—a Python framework to work with high-throughput sequencing data. Bioinformatics 31, 166–169 (2015).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Ye, J. et al. Primer-BLAST: a tool to design target-specific primers for polymerase chain reaction. BMC Bioinformatics 13, 134 (2012).
Huang da, W., Sherman, B. T. & Lempicki, R. A. Bioinformatics enrichment tools: paths toward the comprehensive functional analysis of large gene lists. Nucleic Acids Res. 37, 1–13 (2009).
van Dam, S., Vosa, U., van der Graaf, A., Franke, L. & de Magalhaes, J. P. Gene co-expression analysis for functional classification and gene-disease predictions. Brief. Bioinformatics 19, 575–592 (2018).
Liu, T. et al. Quantitative proteomic analysis of intracerebral hemorrhage in rats with a focus on brain energy metabolism. Brain Behav. 8, e01130 (2018).
Tsuchida, C. et al. Expression of REG family genes in human inflammatory bowel diseases and its regulation. Biochem. Biophys. Rep. 12, 198–205 (2017).
Bouzid, D. et al. Association of ZAP70 and PTPN6, but Not BANK1 or CLEC2D, with inflammatory bowel disease in the Tunisian population. Genet. Test. Mol. Biomark. 17, 321–326 (2013).
Boros, E. et al. Elevated expression of AXL may contribute to the epithelial-to-mesenchymal transition in inflammatory bowel disease patients. Mediat. Inflamm. 2018, 3241406 (2018).
Lyons, J. et al. Integrated in vivo multiomics analysis identifies p21-activated kinase signaling as a driver of colitis. Sci. Signal. 11, eaan3580 (2018).
Li, Y. et al. Bovine colostrum before or after formula feeding improves systemic immune protection and gut function in newborn preterm pigs. Front. Immunol. 10, 3062 (2019).
Oulmaati, A. et al. Risk factors of mild rectal bleeding in very low birth weight infants: a case control study. BMC Pediatr. 13, 196 (2013).
Maayan-Metzger, A., Ghanem, N., Mazkereth, R. & Kuint, J. Characteristics of neonates with isolated rectal bleeding. Arch. Dis. Child Fetal Neonatal Ed. 89, F68–F70 (2004).
Stoy, A. C. et al. Bovine colostrum improves intestinal function following formula-induced gut inflammation in preterm pigs. Clin. Nutr. 33, 322–329 (2014).
Neu, J. & Walker, W. A. Necrotizing enterocolitis. N. Engl. J. Med. 364, 255–264 (2011).
Ren S, et al. Sub-clinical necrotizing enterocolitis-induced systemic immune suppression in neonatal preterm pigs. Am J Physiol Gastrointest Liver Physiol. (2021)
Ren, S., Pan, X., Gao, F., Sangild, P. T. & Nguyen, D. N. Prenatal inflammation suppresses blood Th1 polarization and gene clusters related to cellular energy metabolism in preterm newborns. FASEB J. 34, 2896–2911 (2020).
Nino, D. F., Sodhi, C. P. & Hackam, D. J. Necrotizing enterocolitis: new insights into pathogenesis and mechanisms. Nat. Rev. Gastroenterol. Hepatol. 13, 590–600 (2016).
Robinson, J. L. et al. Prematurity reduces citrulline-arginine-nitric oxide production and precedes the onset of necrotizing enterocolitis in piglets. Am. J. Physiol. Gastrointest. Liver Physiol. 315, G638–G649 (2018).
Shah, P. S., Shah, V. S. & Kelly, L. E. Arginine supplementation for prevention of necrotising enterocolitis in preterm infants. Cochrane Database Syst. Rev. 4, CD004339 (2017).
Maltese, P. et al. Glucocorticoid resistance in Crohn’s disease and ulcerative colitis: an association study investigating GR and FKBP5 gene polymorphisms. Pharmacogenomics J. 12, 432–438 (2012).
Wochnik, G. M. et al. FK506-binding proteins 51 and 52 differentially regulate dynein interaction and nuclear translocation of the glucocorticoid receptor in mammalian cells. J. Biol. Chem. 280, 4609–4616 (2005).
Sangild, P. T. et al. Diet- and colonization-dependent intestinal dysfunction predisposes to necrotizing enterocolitis in preterm pigs. Gastroenterology 130, 1776–1792 (2006).
Siggers, J. et al. Transition from parenteral to enteral nutrition induces immediate diet-dependent gut histological and immunological responses in preterm neonates. Am. J. Physiol. Gastrointest. Liver Physiol. 301, G435–G445 (2011).
Gauffin, F., Nordgren, A., Barbany, G., Gustafsson, B. & Karlsson, H. Quantitation of RNA decay in dried blood spots during 20 years of storage. Clin. Chem. Lab. Med. 47, 1467–1469 (2009).
Acknowledgements
We thank Thomas Thymann, Anders Brunse, Duc Ninh Nguyen, Jing Sun, Kristine Holgersen, Jane Povlsen, Elin Skytte, Kristina Møller (University of Copenhagen), and Jonas Bybjerg-Grauholma (Statens Serum Institut, Denmark) for their support to animal procedures and laboratory analyses. This work was supported by the Innovation Foundation Denmark NEOCOL project (to P.T.S.) and the Agricultural Science and Technology Innovation Program (ASTIP) of China (to F.G.).
Author information
Authors and Affiliations
Contributions
X.P. analyzed and interpreted the transcriptome data, and was the major contributor in writing the manuscript. T.M., S.R., and D.N.N. performed animal experiment and analysis. D.N.N., R.L.S., F.G., and P.T.S. took part in the main study design and critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
Patient consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Pan, X., Muk, T., Ren, S. et al. Blood transcriptomic markers of necrotizing enterocolitis in preterm pigs. Pediatr Res 91, 1113–1120 (2022). https://doi.org/10.1038/s41390-021-01605-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01605-4
This article is cited by
-
Identifying immune signatures of sepsis to increase diagnostic accuracy in very preterm babies
Nature Communications (2024)
-
Brain lipidomics and neurodevelopmental outcomes in intrauterine growth restricted piglets fed dairy or vegetable fat diets
Scientific Reports (2022)