Abstract
Objective
Kawasaki disease (KD) is a childhood vasculitis with conflicting reported North American trends in incidence and patient characteristics. Objectives: (1) determine KD incidence between 1995 and 2017; (2) compare patient characteristics by era and age group; (3) determine complication and cardiovascular follow-up rates.
Methods
We used population-based health administrative data to identify children (0–18 yr) hospitalized with KD in Ontario, Canada between 1995 and 2017. We excluded children with prior KD diagnosis or incomplete records. We determined the annualized incidence and follow-up trends.
Results
KD was diagnosed in 4,346 children between 1995 and 2017. Annual KD incidence was 22.0 (<5 yr), 6.1 (5–9 yr), and 0.6 (10–18 yr) per 100,000 children. KD incidence increased significantly for all age groups, including from 18.4 to 25.0 cases per 100,000 children <5 yr. Ninety-day mortality occurred in ≤5 children (≤0.1%). Coronary artery aneurysm (CAA) occurred in 106 children (2.4%, 95% confidence interval 2.0–2.9) during admission and 151 (3.5%, 95% confidence interval 3.0–4.1) during 11-year median follow-up. Children 10–18 yr had longer hospitalizations (4.3 vs. 3.5 days, p = 0.003) and more CAA (7.4% vs. 3.4%, p = 0.007). By 1-year post-diagnosis, 3970 (91.3%) and 2576 (59.3%) children had echocardiography and cardiology follow-up, respectively.
Conclusions
KD incidence is increasing in Ontario, with greater healthcare utilization from hospitalizations and subsequent follow-up.
Impact
-
4346 children were hospitalized for Kawasaki disease over 22 years in Ontario, and Kawasaki disease incidence increased significantly for all age groups, males and females.
-
Older children (10–18 years) had longer hospital length of stay, more PICU admissions and more frequent coronary artery aneurysms.
-
Nearly all children with Kawasaki disease had follow-up echocardiography within 1 year.
Similar content being viewed by others
Introduction
Kawasaki disease (KD) is a systemic vasculitis that predominantly affects infants and young children. It is hypothesized to result from a systemic immune response in genetically susceptible individuals, triggered by infectious or environmental antigens.1 KD is potentially life-threatening due to coronary artery involvement and is the most common cause of acquired heart disease among children in developed countries.2,3,4 KD has been reported in >60 countries and the global incidence is increasing, driven by rising incidence among Asians.5,6,7,8,9,10 The most recent Japanese Nationwide Survey (2017–2018) reported an incidence of 359 cases per 100,000 children aged <5 yr, which is nearly 20-times higher than the reported incidence in North America for this age group.11,12 In North America, it is also reported that KD incidence has reached a plateau over the past 15 years.6,11,13 Previous Canadian studies have evaluated KD incidence since 1995 using cross-sectional survey data, which were stopped in 2013 due to poor response rates.11,13 These studies generally demonstrated increasing KD incidence, although this was not a consistent finding across all age groups. Based on the available data, it remains unclear whether KD incidence is truly increasing in North America, and in which patient populations the incidence has increased.
There are also limited and conflicting data on disease characteristics among North American children treated with intravenous immunoglobulin (IVIG).6,11,13 Due to the frequency of acute hospitalizations and cardiovascular sequelae, small changes in KD incidence have significant health economic implications. Since children with KD are typically hospitalized for IVIG administration, health administrative data have been used to study KD epidemiology.11,12,13,14,15 We utilized Ontario databases to address three objectives: (1) determine the incidence of KD over a period of two decades, (2) compare children diagnosed with KD by era and age group, and (3) describe rates of acute complications and follow-up patterns after discharge.
Methods
Design and participants
We performed a retrospective population-based cohort study of hospitalized children diagnosed with KD across Ontario. Ontario is Canada’s largest province, with a population that has increased from ~11.1 to 14.0 million people between 1996 and 2016,16 and has a universal healthcare system. This project was authorized under section 45 of Ontario’s Personal Health Information Protection Act and approved by Hamilton Integrated Research Ethics Board. We reported our study in accordance with STROBE17 and RECORD18 statements.
We included all children (0–18 yr) in Ontario between April 1, 1995 and March 31, 2017. Our study exposure was hospitalization with a discharge diagnosis of KD, based on International Classification of Diseases, 9th Revision (ICD-9) [446.1] or ICD-10 [M30.3] codes in the Canadian Institute for Health Information (CIHI) Discharge Abstract Database11 (Supplementary Fig. 1). These codes have been recently validated using this Ontario database (positive predictive value (PPV): 93.5%).11 Among all Ontario children, we excluded those diagnosed with KD within 7 years prior to study initiation (1988–1995). Among our KD cohort, we included only the first eligible hospitalization after 1995, to restrict to new KD diagnoses. We also excluded children in the South East Local Health Integrated Network (due to incomplete outpatient billing records) or without the Ontario Health Insurance Plan (OHIP) coverage during hospitalization. The hospitalization year was determined by fiscal year starting April 1 (e.g., 1995 = April 1, 1995 to March 31, 1996). The cohort was stratified by age (<5, 5–9, and 10–18 years) and index hospitalization era (era 1: 1995–2001, era 2: 2002–2016). These age groups were selected for comparison with previous North American studies.11,12,13,14 Eras were chosen to evaluate the coding system change in 2002 from ICD-9 to ICD-10.
Data sources
We utilized Ontario health administrative data housed at ICES. ICES is an independent, non-profit research institute whose legal status under Ontario’s health information privacy law allows it to collect and analyze healthcare and demographic data, without consent, for health system evaluation and improvement. The databases contain records for all legal Ontario residents with OHIP coverage (>99% of individuals). Administrative databases used included: CIHI Discharge Abstract Database, CIHI Same Day Surgery, National Ambulatory Care Reporting System for emergency department visits, OHIP for physician billings and ETHNIC for surname-based identification of Chinese (sensitivity 80%, PPV 92%) and South Asian (sensitivity 50%, PPV 89%) individuals.19 The Registered Persons Database was used to determine the number of children alive in Ontario each fiscal year. Descriptions of each database are included in Supplementary Appendix 1. These datasets were deterministically linked using unique encrypted identifiers and analyzed at ICES. Complete and uncleaned data were available to investigators for analysis. Emigration from the province (0.1% per year)20 and death were the only reasons for loss to follow-up.
Demographics and comorbidities
We evaluated the characteristics of children with KD, stratified by age and hospitalization era. Demographic variables: age, sex, ethnicity,19 rural status (community < 10,000 persons)21 and neighborhood income quintile (by postal code).22 Hospitalization variables: admission month/year, hospital (first hospital during index episode of care), length of stay, presence of a PICU admission during the index episode of care, hospital complications (coronary artery aneurysm (CAA), myocarditis/pericarditis, macrophage activation syndrome (MAS) or hemophagocytic lymphohistiocytosis (HLH), gallbladder hydrops and hemolytic anemia), IVIG administration and red blood cell (RBC) transfusion. We looked back to birthdate or April 1, 1991 to determine whether the children had pre-existing comorbidities (e.g., cardiovascular, rheumatologic, or renal disorders). Supplementary Appendix 1 contains the administrative codes used to define each variable.
Outcomes
The primary outcome was annualized age- and sex-standardized incidence of KD among all Ontario children. Secondary outcomes included annualized incidence of KD among hospitalized children, frequency of RBC and IVIG transfusions, and seasonal variation in KD incidence. We also studied complications associated with KD such as 90-day mortality (from admission date) and CAA (defined by administrative coding) during hospitalization (CAA during the acute phase of KD) or any time prior to death or March 31, 2018 (any CAA). Finally, we assessed echocardiography and cardiologist visits within 1 year.
Statistical analyses and reporting
Baseline characteristics and outcomes were compared using distribution-appropriate univariable comparison tests. A p-value of <0.05 was considered statistically significant. In accordance with ICES data privacy policies, cell sizes ≤5 individuals were not reported (NR). Annualized KD incidence was determined by the number of KD diagnoses each fiscal year per 100,000 population of all children alive in Ontario on April 1st of that fiscal year (following application of exclusion criteria). Incidence was standardized by age and sex using 2011 Canadian Census data. We then calculated KD incidence among hospitalized Ontario children (per 1000 hospitalized children) and by age at hospitalization (<5, 5–9, and 10–18 years). Cochran–Armitage testing23 was used to evaluate trends in KD incidence and CAA frequency.
Results
Patient and admission characteristics
We identified 4,346 children hospitalized for KD between 1995 and 2017; <5 yr: 3,138 (72.2%), 5–9 yr: 1019 (23.4%) and 10–18 yr: 189 (4.3%) (Table 1). The median age was 3.0 years (IQR 1–5) and 520 children (12.0%) were <1 yr at diagnosis. There was a male predominance, with 2608 males (male-to-female ratio 1.5) (Supplementary Fig. 2). The median follow-up time was 11.2 years (range 0–23). KD cases were evenly distributed across income quintiles. The 2016 Census reported that 10.3% of Ontario’s population lived rurally.21 We found that relatively fewer KD children lived rurally (268, 6.2%). Admission to non-academic centers occurred in 2142 children (49%) and to PICU in 104 (2.4%). Prior cardiovascular events (defined in Supplementary Appendix 1) occurred in 164 children (3.8%).
Stratified by age (Table 1), older children (10–18 yr) had a longer mean length of stay (4.3 days [10–18 yr] vs. 3.6 days [5–9 yr] vs. 3.5 days [<5 yr], p = 0.003) and more frequent PICU admissions (5.3% [10–18 yr] vs. 2.7% [5–9 yr] vs. 2.1% [<5 yr], p = 0.01). Stratified by era (Supplementary Table 1), there was no difference in age at hospitalization or length of stay. There were significantly more children of Chinese origin in era 2 (14.7% vs. 9.2%, p < 0.001), and the proportion of Chinese individuals in the cohort increased gradually over time (Supplementary Fig. 3). This increase mirrored population growth of East Asian individuals in Ontario (Supplementary Fig. 4). Fewer children in era 2 lived rurally (5.3% vs. 8.3%, p < 0.001), consistent with Ontario’s declining rural population (14.8% [1996] vs. 10.3% [2016]).21
Incidence, seasonal variation
Overall KD incidence was 6.9 cases (95% confidence interval (CI) 5.7–8.1) per 100,000 Ontario children. Between 1995 and 2017, KD incidence increased from 6.1 (95% CI 5.1–7.2) to 8.8 cases (95% CI 7.7–10.1) per 100,000 Ontario children (p < 0.001) (Fig. 1).
Stratified by age, KD incidence was 22.0 cases (95% CI 17.8–26.1) per 100,000 children <5 yr, 6.1 cases (95% CI 4.3–7.8) per 100,000 children 5–9 yr and 0.6 cases (95% CI 0.3–1.0) per 100,000 children 10–18 yr. KD incidence increased significantly over time in each age group. Between 1995–2017, KD incidence increased from 18.4 (95% CI 14.9–22.6) to 25.0 cases (95% CI 21.1–29.5) per 100,000 Ontario children <5 yr, increased from 4.0 (95% CI 2.7–5.6) to 7.7 cases (95% CI 5.8–9.9) per 100,000 Ontario children 5–9 yr, and increased from 0.7 (95% CI 0.3–1.3) to 1.1 cases (95% CI 0.6–1.8) per 100,000 Ontario children 10–18 yr (Fig. 2). KD incidence also increased between 1995 and 2017 in males (from 7.5 (95% CI 5.9–9.4) to 11.1 cases (95% CI 9.3–13.1) per 100,000 Ontario male children) and females (from 4.6 (95% CI 3.4–6.0) to 6.5 cases (95% CI 5.2–8.0) per 100,000 Ontario female children) (Supplementary Fig. 5). KD diagnoses were more frequent between November to March and less frequent from August to September (Fig. 3). Seasonal variation in KD incidence closely mirrored that of all-cause pediatric hospitalizations.
“Era 1” (April 1995–March 2002) and “Era 2” (April 2002–March 2017) represent the proportion of Kawasaki disease diagnoses each calendar month. “All hospitalizations” represent the proportion of all-cause pediatric hospitalizations within Ontario occurring each calendar month, across the whole study period.
Outcomes, follow-up
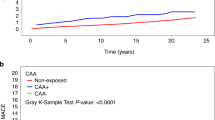
CAA during the acute phase of KD were diagnosed during hospitalization in 106 children (2.4%, 95% CI 2.0–2.9) (Table 2). Any CAA was diagnosed during 11-year median follow-up in 151 children (3.5%, 95% CI 3.0–4.1). Any CAA frequency declined over time (Supplementary Fig. 6), but this was not significant (p = 0.07). There was no difference in the acute phase or any CAA frequency by era (Supplementary Table 2). Myocarditis/pericarditis occurred in 71 children (1.6%), MAS/HLH in 10 (0.2%) and gallbladder hydrops in 26 (0.6%). IVIG administration was coded in 2482 children (57.1%) and was more common in era 2 (67.3% vs. 30.9%, p < 0.001), which may be the result of improved administrative coding. Fifty-one children (1.2%) received RBC transfusions. Mortality within 90 days of hospitalization occurred in ≤5 children (≤0.1%). Older children (10–18 yr) had more frequent acute phase and any CAA, and less frequent IVIG administration (Table 2).
Following discharge, 3970 children (91.3%) had ≥1 follow-up echocardiogram between 14 and 365 days. Echocardiogram follow-up was more frequent in era 2 (94.7% vs. 82.6%, p < 0.001) and among children living in urban vs. rural areas (91.5% vs. 85.0%, p < 0.001). Cardiology follow-up occurred in 2470 children (56.8%) by 90 days and 2576 children (59.3%) by 1 year after hospitalization. Cardiology follow-up within 1 year was less common in era 2 (56.0% vs. 67.7%, p < 0.001).
Discussion
We used health administrative databases to assemble a large cohort of Canadian children diagnosed with KD over two decades. The incidence of KD in Ontario increased significantly over time for all age groups, males and females. Among 4346 KD cases, ≤0.1% died within 90 days and 151 (3.5%) developed any CAA. Older children had longer lengths of hospital stay, more frequent PICU admissions, and more frequent CAA.
Canadian KD surveillance from 1995 to 2013 occurred by triennial cross-sectional surveys. These were discontinued due to regulatory barriers and poor response rate.11 Lin et al.13 reported the 1995–2006 surveys, finding an incidence of 26.2 ( yr), 6.7 (5–9 yr), and 0.9 (10–14 yr) cases per 100,000 population. KD incidence increased during their study, with an increasing proportion of incomplete KD. Manlhiot et al.11 studied Canadian hospitalizations from 2004 to 2014, finding an incidence of 19.6 (<5 yr), 6.4 (5–9 yr), and 1.3 (10–18 yr) cases per 100,000 population. Incidence increased slightly among children 5–9 yr and 10–18 yr, with no difference among <5 yr. In comparison, we observed increased incidence for all age groups over a 22-year period. This is consistent with Asian countries with robust KD surveillance.5,6,7,10,24 KD case ascertainment in Ontario may have increased over time due to greater physician awareness or improved healthcare access. In the absence of diagnostic testing for KD, the increasing incidence may also reflect lower thresholds for diagnosis and treatment of suspected KD cases, in order to prevent potential cardiovascular sequelae. This theory is supported by reports that the proportion of “incomplete KD” cases has increased over time.8,13,25
We found year-to-year variation, with a 2004 peak corresponding to a spatiotemporal KD cluster reported around Toronto.26 This KD cluster was also observed in the Northeast United States,11 suggesting a shared infectious trigger, although no specific infectious disease was identified.26 In the United States, the incidence of KD is highest in Asians and Pacific Islanders.12,27 Japanese-American children in Hawaii have similar KD incidence to children in Japan,28 demonstrating that genetic factors significantly modify KD risk among Asian children. In Canada, a significant correlation exists between KD incidence and Asian population size (r = 0.61, p = 0.03), excluding coastal Maritimes provinces.11 In our study, increasing KD incidence mirrored East Asian population growth in Ontario and the proportion of Chinese children was higher in era 2. These findings suggest that the rising incidence of KD may be correlated with the significant growth of the East Asian population in Ontario over the past two decades.
Data from multiple countries show that in-hospital mortality associated with KD is rare, occurring in 0.01–0.2% of cases.4,5,14,29,30 In Japan, the standardized mortality rate for children with KD is significantly higher during the acute phase of illness.29,31 The risk of mortality peaks between 15 and 45 days after KD onset.32 In our study, ≤0.1% of children died within 90 days. In North America, CAAs are reported in 3–5% of IVIG-treated children.5,11,13,30 Older age at KD diagnosis is associated with less frequent IVIG treatment, delayed diagnosis, and increased cardiovascular complications.33,34,35 This was consistent with our findings that older children (10–18 yr) had longer hospital stays, more PICU admissions, less frequent IVIG administration, and more frequent CAA. Hemolytic anemia is a recognized IVIG side-effect and occurs in 0.4–4% of KD cases.36,37 We found that 1% of children developed hemolytic anemia and received RBC transfusions. The accuracy of administrative coding for IVIG administration is unknown, with no previous validation study. As seen in other administrative database studies in KD,10 we found that coding for IVIG administration appeared to be incomplete in Ontario. However, IVIG administration was significantly more common in era 2, which may reflect increased coding accuracy and IVIG utilization.
Follow-up patterns after KD are poorly understood. KD guidelines applicable during our study period recommended two follow-up echocardiograms, at variable time points.38,39,40 Lowry et al.41 studied 302 American children with normal initial echocardiograms, finding that 250 (83%) had one and 107 (35%) had both follow-up echocardiograms. In our study, follow-up echocardiography occurred in 93% of children and was more common in era 2, despite less frequent cardiology visits. Echocardiogram follow-up was also less common among children living in rural areas, which may be attributable to decreased access to pediatric echocardiography and greater distances from the hospital. These findings suggest that an increasing proportion of KD follow-up care is being provided by non-cardiologists, and compliance with echocardiography guidelines is improving. In Ontario’s universal healthcare system, cardiologist consultation may be reserved for children with cardiac sequelae.
Our study has multiple strengths. We assembled a large cohort of Canadian children diagnosed with KD over 22 years. Compared against previous Canadian epidemiological studies,11,13 this longer study duration demonstrated increasing KD incidence for all age groups, males and females. We also examined patient characteristics and outcomes (e.g., ethnicity, PICU admissions, myocarditis/pericarditis, and hemolytic anemia) not previously reported in Canada. Few publications address follow-up after KD hospitalizations. We provide additional data on echocardiography and cardiology follow-up patterns. We excluded children diagnosed with KD between 1988 and 1995 to approximate a birth cohort of new KD diagnoses. Ontario’s universal healthcare system and low emigration minimized our losses to follow-up. Given the frequency of acute hospitalizations, cost of IVIG, need for echocardiography follow-up and potential long-term cardiovascular disease, the increasing incidence of KD in Ontario holds significant healthcare resource and spending implications. This highlights the importance of research in enhanced diagnostic testing (e.g., novel biomarkers) and therapeutic strategies to avoid unnecessary hospitalizations and medications.
Administrative codes for KD have a high reported PPV42,43 and were validated in the Ontario Discharge Abstract Database against concurrent surveillance survey data.11 However, no code validation study includes a non-KD control cohort. The use of administrative data does have limitations, preventing detailed characterization of KD cases. We cannot validate KD criteria, distinguish complete from incomplete KD using ICD codes. We could not identify KD cases not diagnosed by a physician or hospitalized. The accuracy of our outcome codes (e.g., CAA, IVIG, and echocardiography) are unknown and we are unable to determine CAA Z-score or internal diameter. However, the codes used were specific to CAA (Supplementary Appendix 1) and our observed CAA rate is consistent with clinical studies in the IVIG era.5,13,40,44 We chose to compare baseline characteristic and outcome data between two eras, in order to evaluate differences between administrative coding systems in Ontario (era 1 (1995–2001): ICD-9 and era 2 (2002–2016): ICD-10), and to reduce the number of small cell sizes that could not be reported. We acknowledge that significant differences in patient demographics and outcomes may be present within these eras, which we were unable to detect. We evaluated follow-up echocardiography between 14 and 365 days based on existing KD guidelines during our study and potential differences between administrative service and coding dates. Cardiology visits were ascertained using OHIP billing codes. Physicians practicing but not billing as cardiologists (e.g., not licensed as cardiologists in Ontario) may be excluded, but we hypothesize this was uncommon. Finally, Chinese and South Asian individuals were identified using a surname-based algorithm.19 However, this database is unable to identify individuals of other ethnic groups and excludes surnames shared between ethnic groups such as South Asian Muslims or non-Han Chinese.
Using population-based data, we created a large cohort of North American KD children, accrued over more than two decades. KD incidence increased significantly among all age groups, but CAA frequency has not changed. Older children had longer hospital stays, more PICU admissions, less frequent IVIG treatment, and more frequent CAA. Future research will evaluate the healthcare resource implications of rising KD incidence to better plan for the provision of high-quality healthcare to these patients.
References
Burgner, D. & Harnden, A. Kawasaki disease: what is the epidemiology telling us about the etiology? Int. J. Infect. Dis. 9, 185–194 (2005).
Taubert, K. A., Rowley, A. H. & Shulman, S. T. Nationwide survey of Kawasaki disease and acute rheumatic fever. J. Pediatr. 119, 279–282 (1991).
Taubert, K. A. Epidemiology of Kawasaki disease in the United States and worldwide. Prog. Pediatr. Cardiol. 6, 181–185 (1997).
Holman, R. C. et al. Kawasaki syndrome hospitalizations in the United States, 1997 and 2000. Pediatrics 112, 495–501 (2003).
Makino, N. et al. Nationwide epidemiologic survey of Kawasaki disease in Japan, 2015-2016. Pediatr. Int J. Jpn Pediatr. Soc. 61, 397–403 (2019).
Singh, S., Vignesh, P. & Burgner, D. The epidemiology of Kawasaki disease: a global update. Arch. Dis. Child 100, 1084–1088 (2015).
Lin, M.-T. & Wu, M.-H. The global epidemiology of Kawasaki disease: review and future perspectives. Glob. Cardiol. Sci. Pract. 2017, https://doi.org/10.21542/gcsp.2017.20 (2018).
Ae, R. et al. Epidemiology, treatments, and cardiac complications in patients with Kawasaki Disease: the nationwide survey in Japan, 2017–2018. J. Pediatr. 225, 23–29 (2020).
Kim, G. B. et al. Epidemiology of Kawasaki disease in South Korea: a nationwide survey 2015–2017. Pediatr. Infect. Dis. J. 39, 1012–1016 (2020).
Huang, Y.-H. et al. Increased incidence of Kawasaki disease in Taiwan in recent years: a 15 years nationwide population-based cohort study. Front. Pediatr. 7, 121 (2019).
Manlhiot, C. et al. Epidemiology of Kawasaki disease in Canada 2004 to 2014: comparison of surveillance using administrative data vs periodic medical record review. Can. J. Cardiol. 34, 303–309 (2018).
Holman, R. C. et al. Hospitalizations for Kawasaki syndrome among children in the United States, 1997–2007. Pediatr. Infect. Dis. J. 29, 483–488 (2010).
Lin, Y. T. et al. Repeated systematic surveillance of Kawasaki disease in Ontario from 1995 to 2006: Kawasaki disease in Ontario, Canada. Pediatr. Int. 52, 699–706 (2010).
Chang, R. K. R. Hospitalizations for Kawasaki disease among children in the United States, 1988-1997. Pediatrics 109, e87 (2002).
Williams, C. L. et al. A systematic review of validated methods for identifying Kawasaki disease using administrative or claims data. Vaccine 31, K28–K33 (2013).
Statistics Canada. Ontario [Province] and Canada [Country] (table). Census profile. 2016 Census. https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/index.cfm?Lang=E. Accessed 10 Dec 2019 (2017).
von Elm, E. et al. The strengthening the reporting of observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet Lond. Engl. 370, 1453–1457 (2007).
Benchimol, E. I. et al. The reporting of studies conducted using observational routinely-collected health Data (RECORD) Statement. PLoS Med. 12, e1001885 (2015).
Shah, B. R. et al. Surname lists to identify South Asian and Chinese ethnicity from secondary data in Ontario, Canada: a validation study. BMC Med. Res. Methodol. 10, https://doi.org/10.1186/1471-2288-10-42 (2010)
Chanchlani, R. et al. Secular trends in incidence, modality and mortality with dialysis receiving AKI in children in Ontario: a population-based cohort study. Clin. J. Am. Soc. Nephrol. 14, 1288–1296 (2019).
Bollman, R. Rural Demography Update. Rural Ontario Institute 2016. http://www.ruralontarioinstitute.ca/file.aspx?id=26acac18-6d6e-4fc5-8be6-c16d326305fe. Accessed 10 Dec 2019 (2016).
Canadian Institute for Health Information (CIHI). Health Indicators 2013. Canadian Institute for Health Information 2013. https://secure.cihi.ca/free_products/HI2013_EN.pdf. Accessed 18 Dec 2019 (2013).
Armitage, P. Tests for linear trends in proportions and frequencies. Biometrics 11, 375 (1955).
Kim, G. B. et al. Epidemiology and clinical features of Kawasaki disease in South Korea, 2012-2014. Pediatr. Infect. Dis. J. 36, 482–485 (2017).
Ghelani, S. J. et al. Increased incidence of incomplete Kawasaki disease at a pediatric hospital after publication of the 2004 American Heart Association guidelines. Pediatr. Cardiol. 33, 1097–1103 (2012).
Hearn, J. et al. Spatiotemporal clustering of cases of Kawasaki disease and associated coronary artery aneurysms in Canada. Sci. Rep. 8, 17682 (2018).
Uehara, R. & Belay, E. D. Epidemiology of Kawasaki disease in Asia, Europe, and the United States. J. Epidemiol. 22, 79–85 (2012).
Holman, R. C. et al. Racial/ethnic differences in the incidence of Kawasaki syndrome among children in Hawaii. Hawaii Med. J. 69, 194–197 (2010).
Nakamura, Y. et al. Mortality among Japanese with a history of Kawasaki disease: results at the end of 2009. J. Epidemiol. 23, 429–434 (2013).
Son, M. B. F. et al. Treatment of Kawasaki disease: analysis of 27 US pediatric hospitals from 2001 to 2006. Pediatrics 124, 1–8 (2009).
Nakamura, Y. et al. Mortality among persons with a history of Kawasaki disease in Japan: the fifth look. Arch. Pediatr. Adolesc. Med 156, 162 (2002).
Kato, H., Ichinose, E. & Kawasaki, T. Myocardial infarction in Kawasaki disease: clinical analyses in 195 cases. J. Pediatr. 108, 923–927 (1986).
Muta, H. et al. Older age is a risk factor for the development of cardiovascular sequelae in Kawasaki disease. Pediatrics 114, 751–754 (2004).
Song, D. et al. Risk factors for Kawasaki disease-associated coronary abnormalities differ depending on age. Eur. J. Pediatr. 168, 1315–1321 (2009).
Minich, L. L. et al. Delayed diagnosis of Kawasaki disease: what are the risk factors? Pediatrics 120, e1434–e1440 (2007).
Nolan, B. E. et al. High-dose intravenous immunoglobulin is strongly associated with hemolytic anemia in patients with Kawasaki disease. Transfusion 58, 2564–2571 (2018).
Luban, N. L. C. et al. Intravenous immunoglobulin-related hemolysis in patients treated for Kawasaki disease: IVIG-related hemolysis and Kawasaki disease. Transfusion 55, S90–S94 (2015).
McCrindle, B. W. et al. Diagnosis, treatment, and long-term management of kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation 135, e927–e999 (2017).
Dajani, A. S. et al. Guidelines for long-term management of patients with Kawasaki disease. Report from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation 89, 916–922 (1994).
Newburger, J. W. et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics 114, 1708–1733 (2004).
Lowry, A. W. et al. Variability in delivery of care and echocardiogram surveillance of Kawasaki disease. Congenit. Heart Dis. 7, 336–343 (2012).
Bronstein, D. E., Besser, R. E. & Burns, J. C. Passive surveillance for Kawasaki disease in San Diego County. Pediatr. Infect. Dis. J. 16, 1015–1018 (1997).
Kao, A. S. et al. Spatial and temporal clustering of Kawasaki syndrome cases. Pediatr. Infect. Dis. J. 27, 981–985 (2008).
Holve, T. J. et al. Long-term cardiovascular outcomes in survivors of Kawasaki disease. Pediatrics 133, e305–e311 (2014).
Acknowledgements
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. This study received funding from institutional grants from Hamilton Health Sciences and McMaster University Department of Pediatrics. Parts of this material are based on data and/or information compiled and provided by CIHI. However, the analyses, conclusions, opinions, and statements expressed in the material are those of the authors, and not necessarily those of CIHI. We thank the ICES McMaster and Ottawa teams, including Richard Perez for his dedicated work planning and supervising analysis for this study, as well as Erin O’Leary for project coordination. M.B. was supported by a New Investigator Fund from Hamilton Health Sciences. C.R. was supported by Resident Research Award funding from the Department of Pediatrics, McMaster University. E.I.B. was supported by a New Investigator Award from the Canadian Institutes of Health Research, Canadian Association of Gastroenterology, and Crohn’s and Colitis Canada. E.I.B. was also supported by the Career Enhancement Program of the Canadian Child Health Clinician Scientist Program.
Author information
Authors and Affiliations
Contributions
C.R., R.C., and M.B. conceptualized and designed the study, coordinated and supervised data collection and analysis, drafted the initial manuscript, and reviewed and revised the manuscript. H.S., E.D., and E.I.B. conceptualized and designed the study, coordinated and supervised data collection and analysis, and reviewed and revised the manuscript. S.B., C.D., T.M., R.P., J.K., B.K., E.K., C.J.-R., and R.W. reviewed and revised the proposed study design, reviewed data analyses, assisted with data interpretation, and reviewed and revised the manuscript. A.G. conceptualized and designed the study, was primarily responsible for data collection and analysis, and reviewed and revised the manuscript. All authors have approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Data sharing
Deidentified individual participant data will not be made available.
Ethical approval
The use of data in this project was authorized under section 45 of Ontario’s Personal Health Information Protection Act and was approved by Hamilton Integrated Research Ethics Board.
Patient consent
ICES is an independent, non-profit research institute whose legal status under Ontario’s health information privacy law allows it to collect and analyze healthcare and demographic data, without consent, for health system evaluation and improvement.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Robinson, C., Chanchlani, R., Gayowsky, A. et al. Incidence and short-term outcomes of Kawasaki disease. Pediatr Res 90, 670–677 (2021). https://doi.org/10.1038/s41390-021-01496-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01496-5
This article is cited by
-
Unexpectedly high incidence of Kawasaki Disease in a Canadian Atlantic Province- an 11-year retrospective descriptive study
Pediatric Rheumatology (2023)
-
Cardiovascular outcomes in children with Kawasaki disease: a population-based cohort study
Pediatric Research (2023)
-
Cardiovascular Outcomes During Index Hospitalization in Children with Kawasaki Disease in Ontario, Canada
Pediatric Cardiology (2023)