Abstract
Background
We aimed to determine the reference values to define an age-specific normal range of controlled attenuation parameter (CAP, a measure of liver steatosis) and liver stiffness measurement (LSM) values assessed by ultrasound-based transient elastography in adolescents without underlying liver disease.
Methods
A total of 462 participants were included in this cross-sectional study using data from NHANES 2017–2018. LSM and CAP were carried out using the FibroScan® M-probe. Anthropometric, metabolic and hematological parameters were measured.
Results
The median CAP was 199.0 dB/m (150.0–245.0 dB/m, 10th to 90th percentiles) and the median LSM was 4.7 kPa (3.4–6.3 kPa, 10th to 90th percentiles) for ages 12–19.9 years. Regression analyses show that the CAP and LSM were not positively correlated with age (boys CAP R2 = 0.001, p = 0.576 and LSM R2 = 0.012, p = 0.096; girls CAP R2 = 0.011, p = 0.113 and LSM R2 = 0.006, p = 0.236). Finally, CAP was positively associated with LSM in girls (β = 0.189, p = 0.005) but not in boys (β = −0.083, p = 0.202).
Conclusions
The reference values indicated here for LSM and CAP will help in the screening of adolescents between ages 12 and 19.9 years and might serve as a useful method for identifying those youth at high risk of nonalcoholic fatty liver disease.
Impact
-
The reference values indicated in this study for liver stiffness measurement (LSM) and controlled attenuation parameter (CAP) will help in the screening of adolescents between ages 12 and 19.9 years in clinical practice.
-
The cutoffs of LSM and CAP might serve as a useful method for identifying those youth at high risk of nonalcoholic fatty liver disease.
Similar content being viewed by others
Introduction
Prevalence studies have reported an increase in the incidence of hepatic disorders in children and adolescents, likely fueled by the alarming rates of youth obesity that can lead to hepatopathies, such as nonalcoholic fatty liver disease (NAFLD) or even non-alcoholic steatohepatitis.1,2 Indeed, epidemiological data show a mean prevalence of NAFLD of 7.6% in the general population3 and some studies describe a wide range in the reported prevalence of NAFLD in children, from <2 to >40%.1,4 This enormous range is due, in part, to differences in study design, methodology, and population, including accuracy of the diagnostic modality used, geography, race, ethnicity, setting, and health status.5
In clinical practice, NAFLD diagnosis is established by the detection of steatosis, which can be performed by imaging techniques or liver biopsy, and by the exclusion of other causes of abnormal transaminase values and hepatic fatty infiltration (e.g., viral infection, celiac disease, autoimmune hepatitis, and metabolic liver disease, among others) by medical history and laboratory screening.1 Hepatic biopsy is considered the gold standard in the diagnosis of NAFLD, but parental refusal for this invasive procedure is common, especially since other noninvasive diagnostic tools are available, including magnetic resonance imaging, liver ultrasound transient elastography (TE), two-dimensional (2D) shear wave elastography, hepatic Doppler, or ultrasonography.6
The FibroScan® device (Echosens, Paris, France) was developed to use ultrasound-based TE to determine the controlled attenuation parameter (CAP), a measure of liver steatosis, and liver stiffness measurement (LSM). Both parameters can be obtained simultaneously by the device in a rapid, noninvasive, reproducible, and painless manner. In a systematic review comparing TE with biopsy for the detection of fibrosis, advanced fibrosis, and cirrhosis, the mean area under the receiver operating characteristic curve for TE was 0.85, 0.92, and 0.94, respectively.7 The diagnostic accuracy of TE is considered excellent (93–96%) for ruling out advanced liver diseases in adults.8 Moreover, the accuracy of the CAP measurement for the detection of steatosis compared with biopsy for steatosis ≥10% as determined by area under curve was 0.81, and for steatosis >34% this value was 0.80.9,10,11,12,13 A recent individual patient data meta-analysis concluded that CAP provides a standardized noninvasive measure of hepatic steatosis.12 However, the FibroScan® with the M-probe has seldom been used in the assessment of liver fat and fibrosis in youth with liver diseases,14,15 and accordingly, the reference values for CAP and LSM have not yet been established in a large sample of youth without liver disease.
While use of the FibroScan device has become routine practice in adults, the question remains of whether both the technique and the diagnostic cutoff values for adults can be applied to youth,16,17 and in this line, published TE data for people aged <20 years remain scarce. Accordingly, the purpose of the present study was to define an age-specific normal range of CAP and LSM values in adolescents without underlying liver disease using data from the 2017–2018 National Health and Nutrition Examination Surveys (NHANES), a program developed to evaluate the health and nutritional status of children and adults in the United States.
Methods
Design and study population
This cross-sectional study used data from NHANES 2017–2018, the details of which are available elsewhere.18 Participants aged ≥18 years provided written consent, adolescents aged 12–17 years provided documented assent, and parental permission was obtained for those aged <18 years. All procedures conformed to the tenets of the Declaration of Helsinki of 1975 (revised in 2013). NHANES was approved by the National Center for Health Statistics research ethics review board (CDC, 2016). Further approval was not sought for our study because the data used were free of personal identifiers [https://wwwn.cdc.gov/nchs/nhanes/].
Participants
Of the 9952 participants in NHANES (2017–2018) who were aged 0–80 years, 1194 were aged <20 years. Inclusion criteria for the study were the following: (i) clinically healthy participants aged between 12 and 19 years; (ii) normal weight (body mass index [BMI] ≥–2 to ≤+1 standard deviation [SD]); (iii) without chronic liver disorder; (iv) normal laboratory parameters (complete cellular blood count, metabolic and liver function parameters); and (v) a complete TE test. Data from 1080 individuals were available for eligible analyses. Additionally, exclusion criteria were: (i) bilirubin >17.1 μmol/L (n = 30); (ii) alanine aminotransferase (ALT) >40 IU/L (n = 52); (iii) γ-glutamyl transferase (GGT) >84 U/L (n = 1); (iv) glucose >6.0 mmol/L (n = 7); (v) cholesterol >5.2 mmol/L (n = 24); (vi) high-sensitivity C-reactive protein (hsCRP) >10 mg/dl (n = 5); (vii) blood pressure >140/90 mmHg (n = 1); (viii) self-reported liver disease (n = 2); (ix) overweight+obesity (n = 405); (x) thinness [very under/underweight] (n = 56); and (xi) positive for HBsAg/IgG, anti-HBc/anti-HCV/anti-HIV antibodies, and/or others (n = 34). One participant was excluded as a clear outlier for the LSM value (+3 SD). Figure 1 shows the flowchart of the data management process.
Instrumentation and measurements
All measurement procedures were taken from the published guidelines and procedures used by NHANES [https://wwwn.cdc.gov/nchs/nhanes/]. The liver status examination component was added to provide nationally representative data of fatty liver disease in the general population and to develop interventions that will reduce the public health burden.
Age was reported during the NHANES examination and was grouped as 12–13.9, 14–15.9, 16–17.9, and 18–19.9 years. Anthropometric measures (body mass, height, and waist circumference) were collected by trained health technicians. Z-score relative values were calculated with the SAS code provided by the WHO Anthro Team.19 Body fat percentage was measured by dual-energy x-ray absorptiometry using a Hologic QDR 4500A densitometer (Hologic Inc., Bedford, MA). Metabolic parameters (total cholesterol, glucose, glycohemoglobin, ALT, aspartate aminotransferase [AST], GGT, total bilirubin, hsCRP, and ferritin concentrations) were measured on the Roche Cobas 6000 (c501 module) analyzer by highly trained medical personnel in the NHANES Mobile Examination Center (MEC) using standard protocols. Hematological testing (white blood cell [WBC] count, red blood cell count, packed cell volume, hemoglobin concentration, mean corpuscular volume, mean corpuscular hemoglobin, mean corpuscular hemoglobin concentration, red cell distribution width) and WBC subfraction (lymphocytes, monocytes, neutrophils, basophils, eosinophils, and platelets) was based on the Beckman Coulter® method of counting and sizing, in combination with an automatic diluting and mixing device for sample processing. Resting systolic and diastolic blood pressures were measured 3–4 times with a sphygmomanometer by trained staff. All participants who presented normal values of both laboratory parameters and ultrasound according to age and sex were finally included in our study.
The TE measurements were obtained in the NHANES MEC using the FibroScan® model V2 Touch, equipped with a medium (M, 3.5 mHz, diameter 7 mm) probe (in 99% of tests). To achieve a value of “normal range” liver status as accurately as possible, participants were excluded if they (i) were unable to lie down on the examination table, (ii) were pregnant, (iii) had an implanted electronic medical device, or (iv) were wearing a bandage or had lesions on the right side of their abdomen near to the ribs. Liver status imaging was performed with the subject lying in supine position. The device estimates hepatic steatosis in decibels/meter (dB/m) and the LSM in kilopascals (kPa). The median CAP in dB/m, LSM in kPa, and interquartile range values of each participant were obtained simultaneously in the examination. Results were included in the final analysis only if the following three criteria were met: fasting time of at least 3 h, ≥10 complete measures, and the interquartile range was <30% of the median value. The inter-rater reliability (health technician compared with reference examiners, n = 32) was 0.86 for LSM and 0.94 for CAP. In addition, NHANES used four shear wave liver fibrosis phantoms (CIRS Model 039) for determining variances within and between FibroScan® devices and probes over time. The intra-machine coefficient of variation was 1.4–3.2%. A detailed description of quality assurance and quality control measures considered for this component can be found in the NHANES—Liver Ultrasound Transient Elastography Procedures Manual (https://wwwn.cdc.gov/nchs/nhanes/ContinuousNhanes/Manuals.aspx?BeginYear=2017).
During the interview, participants or proxy respondents (such as parents) were asked to report lifestyles, education level, race, and medical conditions. For a subset of individuals, lifestyle outcomes (i.e., hours watching TV or videos over the past 30 days and days physically active at least 60 min) and the number of usual hours sleep on weekdays or workdays and weekends (range 3–13.5 h) were recorded. Finally, education level (4–5th grade, 6–8th grade, 9–12th grade, no diploma, General Educational Development credential or equivalent, high school graduate, and other factors such as more than high school and/or less than 9th grade), race/ethnicity (non-Hispanic white, non-Hispanic black, Mexican American or other Hispanic, and other, including multiracial), and medical condition data were recorded.
Statistical analyses
We performed all analyses using SPSS statistical package version 26 (IBM Inc., Chicago, IL). Statistical analysis comprised both descriptive statistics and inferential statistics. Normality for selected variables was verified using histograms and Q-Q plots. Differences in these characteristics across age categories were tested using linear regression and logistic regression for continuous and categorical variables, respectively. Differences in the prevalence of ALT according to thresholds for high/low (90th percentile) LSM and CAP median values were analyzed using χ2 tests.
CAP and LSM median values were then used to generate sex- and age-specific normative percentiles (P) in LSMchartmaker Pro (V.2.43, The Institute of Child Health, London, UK), which analyzes data using the Lambda (L) Mu (M) Sigma (S) method.20 Using penalized likelihood estimation, the P3, P10, P25, P50, P75, P90, and P97 smoothing centiles were chosen as age- and sex-specific reference values and can be expressed in terms of smoothing parameters or equivalent degrees of freedom.21 Lineal and non-lineal regression analyzes were calculated to determine the variation of CAP and LMS median values with age. Likewise, linear regression analysis was used to determine the relationship between CAP and LMS median values by sex. Finally, an analysis of covariance was used to investigate whether clinical characteristics differed by CAP and LMS median value group by applying the P90 cutoff point in both the gender and age groups, controlling for gender and age. The p values for all statistical analyses were two tailed, with a significance level of 0.05.
Results
Descriptive data presented as means, SD, and percentages across age categories are shown in Table 1. Body mass, waist circumference, Z-score BMI, metabolic risk factors (glucose, ALT, AST, GGT, total bilirubin), CAP and LSM values, and days physically active were significantly higher in boys than in girls (p < 0.01). Girls showed higher levels for body fat, total cholesterol, hsCRP, WBC, and sleep hours (weekends) than boys (p < 0.01).
To aid in the clinical interpretation of TE values, we reported the summary of CAP (dB/m) and LSM (kPa) measures (Tables 2 and 3 and Fig. 2) in each age- and sex-specific group. In boys aged 12–19 years, the median (range) for CAP was 198.6–204.4 dB/m (mean 199.9, SD 39.1) and for LSM the range was 4.4–4.9 kPa (mean 4.8, SD 1.5). The median (range) in girls were 186.3–205.9 dB/m (mean 200.7, SD 42.6) for CAP and 4.3–4.4 kPa (mean 4.3, SD 1.1) for LSM. The corresponding smoothed centile curves (P10, P50, and P75) are presented in Fig. 3. CAP and LSM were not positively correlated with age (boys CAP R2 = 0.001, p = 0.576 and LSM R2 = 0.012, p = 0.096; girls CAP R2 = 0.011, p = 0.113 and LSM R2 = 0.006, p = 0.236). CAP was positively associated with LSM in girls (β = 0.189, p = 0.005) but not in boys (β = −0.083, p = 0.202).
Adjusted age and sex thresholds for high/low (90th percentile) LSM and CAP median values for clinical and biochemical profile differences of participants aged 12–19 years from NHANES (2017–2018) are provided in Fig. 4. Adjusted analysis of variance showed that there were differences in clinical outcomes (body mass, Z-score BMI, waist circumference, systolic blood pressure) and biochemical profile (ALT, GGT, ferritin levels) according to thresholds for high/low (90th percentile) LSM and CAP median values.
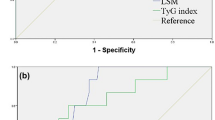
In addition to the adjusted thresholds for high/low (90th percentile) LSM and CAP median values, two previously published ALT cutoff points for diagnosing hepatic steatosis in children and youth were applied in the present study population: (a) the ALT concentrations of >22 IU/L in girls and >26 IU/L in boys, according to the criteria proposed by Schwimmer et al.,22 and (b) the ALT cutoffs of ≥24 proposed by Ruhl and Everhar.23 Significant differences were observed for the prevalence of high ALT levels according to thresholds for high/low (90th percentile) LSM and CAP median values (all p < 0.05) (Supplemental Fig. S1).
Discussion
The accuracy of FibroScan® vibration-controlled TE in assessing liver steatosis and liver fibrosis in patients has been postulated.24,25 Our study highlights the use of both CAP and LSM, with the goal of guiding pediatricians who wish to apply the technique, and provide normal liver status values from healthy youth for reference.
In the update of the guidelines on liver elastography of the World Federation of Ultrasound in Medicine and Biology, a section is dedicated to the assessment of liver steatosis because of its increasing relevance and the rising worldwide prevalence of NAFLD.26 The reference values presented in this study will be a valuable resource in the clinical assessment of liver function and for comparisons with studies from other countries as suggested by World Federation of Ultrasound in Medicine and Biology. To the best of our knowledge, while CAP and LSM are documented in adults,7,25 a few studies27,28,29 have focused on identifying reference values for both CAP and LSM in children and/or adolescents using TE.
Our study did not show age- and sex-dependent values of CAP or LSM values. In this line, several studies based on TE found no influence of gender or sex on liver stiffness,28,29,30,31 whereas others reported lower LSM values in women, most likely due to the anti-fibrogenic effect of estrogen.31,32 In accordance with our results, Tokuhara et al.23 did not show age-dependent values of CAP in youths by TE.
As far as we know, our study is the first to report CAP reference values based on a large, nationally representative population of adolescents. The recent study by Tokuhara et al.27 in 139 healthy children, (median age, 11.7 years; age range, 1.3–17.2 years) reported age-dependent reference values for LSM and an age-independent reference value for CAP in children over a wide range of ages. In their study, the median CAP values were 183 dB/m (112–242) for ages 1–17.2 years and 190 dB/m (111–288) for ages 12–18 years. Similarly, in our study, CAP was not positively correlated with age (boys rho = 0.035 and girls rho = 0.107, p > 0.05), criteria similar to those used by Tokuhara et al.,23 such as normal serum liver enzymes, normal hematologic parameters, healthy blood pressure, without a history of hepatopathy, and normal weight (BMI ≥−2 to ≤+1 SD).
In our study, TE revealed similar 50th percentile values between the four age groups: 4.4 kPa in participants with the age between 12 and 13.9 years, 4.7 kPa in those between 14 and 15.9 years, 4.6 kPa between 16–17.9 years, and 4.5 kPa in those between 18 and 19.9 years. The first reference LSM values for children/adolescents were published by Engelmann et al.29 from a cohort of 235 healthy Caucasian children between 0 and 18 years of age without evidence of liver disease. In this study, median LSM values were 5.1 kPa for adolescents aged 12–18 with age-dependent LSM. Goldschmidt et al.28 described a median LSM of 4.6 kPa (2.8–8.9) in adolescents 11–18 years, without sex differences (male = 4.4 kPa, range 2.8–8.1 vs female = 4.6 kPa range 2.5–8.9), with no age-related differences. By contrast, Tokuhara et al.27 showed a significant age-dependent increase, with values of 3.4 kPa (2.3–4.6, 5th to 95th percentile) for preschoolers, 3.8 kPa (2.5–6.1) for elementary schoolers, and 4.1 kPa (3.3–7.9) for adolescents. However, there were no significant differences in LSM between boys and girls in each age group. Finally, Mărginean et al.17 reported values of 3.7 ± 0.5 kPa in adolescents between 12 and 15 years of age and 3.6 ± 0.5 kPa in adolescents between 15 and 18 years for liver stiffness using a 2D shear wave device.
By using TE and providing both CAP and LSM values, we propose a reference for the normal upper limit defined as 1.33 times the SD or 90th percentile. In healthy adolescent boys/girls, the upper normal limit for CAP is 258.9/243.1 dB/m (12–13.9 years), 251.9/266.3 dB/m (14–15.9 years), 247.0/265.2 dB/m (16–17.9 years), and 249.3/246.0 dB/m (18–19.9 years). For LSM, the upper normal limit in boys/girls is 6.6/5.0 kPa (12–13.9 years), 7.5/6.2 kPa (14–15.9 years), 7.2/6.0 kPa (16–17.9 years), and 6.9/6.0 kPa (18–19.9 years) in healthy adolescents without abnormal serum liver enzymes, hematologic parameters, blood pressure, history of hepatopathy, or unhealthy weight.
Our study has some limitations, including the unavailability of liver biopsies to confirm the absence of fibrosis in the study population, even though it is not justified in healthy adolescents. In addition, the NHANES sample sizes for some demographic subgroups, as well as the number of primary sampling units, are small. Missing data on lifestyle should also be considered. The study included secondary data sources, and the researchers were not in control of the data collection procedures. But, by using stringent criteria to define a healthy population, the margin of error is likely to be minimized. Our study has multiple strengths, such as the assessment of liver stiffness by TE methods in a young and healthy population, the fact that all assessments were performed by experienced and skilled trained staff from NHANES, the large sample size, the accuracy of the statistical analysis, and the establishment of cutoffs for CAP and LSM that are essential as reference values when assessing adolescents with different hepatic disorders.
In conclusion, considering the worldwide increase in pediatric obesity, the reference values of the liver ultrasound TE component might serve as a useful method for identifying those youth at high NAFLD risk and its progression. Moreover, our findings are also very important for the literature since data regarding the assessment of both CAP and LSM in healthy adolescents are scarce.
References
Yu, E. L. et al. Prevalence of nonalcoholic fatty liver disease in children with obesity. J. Pediatr. 207, 64–70 (2019).
Loomba, R. & Sanyal, A. J. The global NAFLD epidemic. Nat. Rev. Gastroenterol. Hepatol. 10, 686–690 (2013).
Schwimmer, J. B. et al. Magnetic resonance imaging and liver histology as biomarkers of hepatic steatosis in children with nonalcoholic fatty liver disease. Hepatology 61, 1887–1895 (2015).
Jimenez-Rivera, C. et al. Prevalence and risk factors for non-alcoholic fatty liver in children and youth with obesity. BMC Pediatr. 17, 113 (2017).
Di Sessa, A. et al. Pediatric non-alcoholic fatty liver disease: current perspectives on diagnosis and management. Pediatr. Health Med. Ther. 10, 89–97 (2019).
Machado, M. V. & Cortez-Pinto, H. Non-invasive diagnosis of non-alcoholic fatty liver disease. A critical appraisal. J. Hepatol. 58, 1007–1019 (2013).
Jiang, W. et al. Diagnostic accuracy of point shear wave elastography and transient elastography for staging hepatic fibrosis in patients with non-alcoholic fatty liver disease: a meta-analysis. BMJ Open 8, 21787 (2018).
Friedrich-Rust, M., Poynard, T. & Castera, L. Critical comparison of elastography methods to assess chronic liver disease. Nat. Rev. Gastroenterol. Hepatol. 13, 402–411 (2016).
Myers, R. P. et al. Controlled attenuation parameter (CAP): a noninvasive method for the detection of hepatic steatosis based on transient elastography. Liver Int. 32, 902–910 (2012).
de Lédinghen, V. et al. Controlled attenuation parameter for the diagnosis of steatosis in non-alcoholic fatty liver disease. J. Gastroenterol. Hepatol. 31, 848–855 (2016).
Sasso, M. et al. Liver steatosis assessed by controlled attenuation parameter (CAP) measured with the XL probe of the FibroScan: a pilot study assessing diagnostic accuracy. Ultrasound Med. Biol. 42, 92–103 (2016).
Karlas, T. et al. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J. Hepatol. 66, 1022–1030 (2017).
Petroff, D. et al. Assessment of hepatic steatosis by controlled attenuation parameter using the M and XL probes: an individual patient data meta-analysis. Lancet Gastroenterol. Hepatol. 6, 185–198 (2021).
Belei, O. et al. Comparison of three ultrasound based elastographic techniques in children and adolescents with chronic diffuse liver diseases. Med. Ultrason. 18, 145–150 (2016).
Nobili, V. et al. Accuracy and reproducibility of transient elastography for the diagnosis of fibrosis in pediatric nonalcoholic steatohepatitis. Hepatology 48, 442–448 (2008).
Zeng, J. et al. Feasibility study and reference values of FibroScan 502 with M probe in healthy preschool children aged 5 years. BMC Pediatr. 19, 129 (2019).
Mărginean, C. O., Meliţ, L. E., Ghiga, D. V. & Săsăran, M. O. Reference values of normal liver stiffness in healthy children by two methods: 2D shear wave and transient elastography. Sci. Rep. 10, 1–10 (2020).
Johnson, C. L., Dohrmann, S. M., Burt, V. L. & Mohadjer, L. K. National health and nutrition examination survey: sample design, 2011–2014. Vital Health Stat. 2 162, 1–33 (2014).
De Onis, M. et al. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 85, 660–667 (2007).
Cole, T. J. & Green, P. J. Smoothing reference centile curves: the LMS method and penalized likelihood. Stat. Med. 11, 1305–1319 (1992).
Pan, H. & Cole, T. User’s Guide to LMSchartmaker (Medical Research Council, 2010).
Schwimmer, J. B. et al. SAFETY study: alanine aminotransferase cutoff values are set too high for reliable detection of pediatric chronic liver disease. Gastroenterology 138, 1357–1364 (2010).
Ruhl, C. E. & Everhart, J. E. Upper limits of normal for alanine aminotransferase activity in the United States population. Hepatology 55, 447–454 (2012).
Eddowes, P. J. et al. Accuracy of FibroScan controlled attenuation parameter and liver stiffness measurement in assessing steatosis and fibrosis in patients with nonalcoholic fatty liver disease. Gastroenterology 156, 1717–1730 (2019).
Gherlan, G. S. Liver ultrasound elastography: more than staging the disease. World J. Hepatol. 7, 1595–1600 (2015).
Ferraioli, G. et al. Liver ultrasound elastography: an update to the World Federation for Ultrasound in Medicine and Biology Guidelines and Recommendations. Ultrasound Med. Biol. 44, 2419–2440 (2018).
Tokuhara, D., Cho, Y. & Shintaku, H. Transient elastography-based liver stiffness age-dependently increases in children. PLoS ONE 11, e0166683 (2016).
Goldschmidt, I. et al. Application and limitations of transient liver elastography in children. J. Pediatr. Gastroenterol. Nutr. 57, 109–113 (2013).
Engelmann, G. et al. Feasibility study and control values of transient elastography in healthy children. Eur. J. Pediatr. 171, 353–360 (2012).
Galina, P. et al. Performance of two–dimensional ultrasound shear wave elastography: reference values of normal liver stiffness in children. Pediatr. Radiol. 49, 91–98 (2019).
Corpechot, C., El Naggar, A. & Poupon, R. Gender and liver: is the liver stiffness weaker in weaker sex? Hepatology 44, 513–514 (2006).
Şirli, R., Sporea, I., Tudora, A., Deleanu, A. & Popescu, A. Transient elastographic evaluation of subjects without known hepatic pathology: does age change the liver stiffness? J. Gastrointest. Liver Dis. 18, 57–60 (2009).
Acknowledgements
R.R.-V. is funded in part by a Postdoctoral Fellowship Resolution ID 420/2019 of the Universidad Pública de Navarra. A.G.-H. is a Miguel Servet Fellow (Instituto de Salud Carlos III—CP18/0150). The author(s) received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final version of the manuscript. R.R.-V. contributed to the conception and study design and reviewed/edited manuscript. M.C.-R. analyzed and interpreted the data and wrote the manuscript. A.G.-H. analyzed the data, performed statistical analyses, and reviewed/edited manuscript. M.I. contributed to the conception, study design, and data interpretation and reviewed/edited manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical conduct of research
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent was obtained for all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Ramírez-Vélez, R., García-Hermoso, A., Correa-Rodríguez, M. et al. Defining values for controlled attenuation parameter and liver stiffness in youth without liver disease. Pediatr Res 91, 912–920 (2022). https://doi.org/10.1038/s41390-021-01441-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01441-6
This article is cited by
-
Association between hypertension and the prevalence of liver steatosis and fibrosis
BMC Endocrine Disorders (2023)
-
Association between type 2 diabetes status and prevalence of liver steatosis and fibrosis among adults aged ≥ 40 years
BMC Endocrine Disorders (2022)