Abstract
Morbidity and mortality in prematurely born infants have significantly improved due to advancement in perinatal care, development of NeuroNICU collaborative multidisciplinary approaches, and evidence-based management protocols that have resulted from a better understanding of perinatal risk factors and neuroprotective treatments. In premature infants with intraventricular hemorrhage (IVH), the detrimental secondary effect of posthemorrhagic ventricular dilation (PHVD) on the neurodevelopmental outcome can be mitigated by surgical intervention, though management varies considerably across institutions. Any benefit derived from the use of neuromonitoring to optimize surgical timing and technique stands to improve neurodevelopmental outcome. In this review, we summarize (1) the approaches to surgical management of PHVD in preterm infants and outcome data; (2) neuromonitoring modalities and the effect of neurosurgical intervention on this data; (3) our resultant protocol for the monitoring and management of PHVD. In particular, our protocol incorporates cerebral near-infrared spectroscopy (NIRS) and transcranial doppler ultrasound (TCD) to better understand cerebral physiology and to enable the hypothesis-driven study of the management of PHVD.
Impact
-
Review of the published literature concerning the use of near-infrared spectroscopy (NIRS) and a cerebral Doppler ultrasound to study the effect of cerebrospinal fluid drainage on infants with posthemorrhagic ventricular dilation.
-
Presentation of our institution’s evidence-based protocol for the use of NIRS and cerebral Doppler ultrasound to study the optimal neurosurgical treatment of posthemorrhagic ventricular dilation, an as yet inadequately studied area.
Similar content being viewed by others
Introduction
Of the ~500,000 prematurely born infants in the United States per year, intraventricular hemorrhage (IVH) develops in about 15–30% of infants weighing <1500 g at birth.1,2,3,4 Posthemorrhagic ventricular dilation (PHVD) occurs in about 30–50% of infants with severe IVH, progressive PVHD spontaneously arrests in about 40%, and 30–50% of the remainder ultimately undergo ventriculoperitoneal (VP) shunt placement.3,5,6,7 In infants <1500 g, IVH incidence has decreased from 40–50% in the 1970s–1980s to 20–25% in the 1990s.5 The incidence of cerebral palsy in those born at gestational age less than 34 weeks has decreased by a factor of three from the 1990s to the 2000s.1 Brain injury associated with PHVD results from the initial hemorrhagic insult, toxic metabolic sequelae of the hemorrhage, and progressive ventricular dilation.8,9 Therapeutic progress in each of these categories has resulted in improved outcomes. The hemorrhage risk, which is highest in the first three postnatal days,1,10 has been mitigated by optimizing perinatal risk factors and neuroprotective treatments such as steroids, surfactant, antibiotics, cesarean section, positive pressure and high-frequency ventilation, and hemodynamic monitoring.4 Surgical reduction of toxic blood products via neuroendoscopic lavage, as well as drainage, irrigation, and fibrinolytic therapy (DRIFT) have a beneficial effect on developmental outcomes, though fibrinolytic therapy increases rehemorrhage risk.11,12,13,14 Though CSF diversion via shunt placement is the most common surgical endpoint, surgical practices and intervention thresholds vary significantly.8,15 Criteria for surgical intervention are mainly based on physical exam and ventricle measurements on cranial ultrasound (CUS), which embody the current standard of care and strongest evidence base, but incompletely measure the pathophysiologic processes leading to brain injury associated with PHVD.8,15 Incorporating additional noninvasive neuromonitoring modalities into the management of PHVD, in particular near-infrared spectroscopy (NIRS) and transcranial doppler ultrasound (TCD) studies, has the potential to improve understanding of this disease process and to guide research on its management. In addition, there is growing support for considering the neurodevelopmental outcome, instead of shunt dependence, to be the most important surgical outcome measure.16
The term posthemorrhagic hydrocephalus (PHH) is often used in surgical literature because hydrocephalus implies a pathologic state requiring surgical treatment. The PHH and PHVD classifications overlap, and the variation in terminology can make direct comparisons of management and outcomes more difficult. PHVD is used in this review as an objective anatomic description that includes the subset of patients who progress to PHH.
The neurosurgical management of PHVD and NICU neuromonitoring modalities have been reviewed extensively. Our objectives are to review (1) current approaches to surgical management of PHVD in preterm infants and outcome data, in particular, neurodevelopmental outcome; (2) neuromonitoring modalities and the effect of neurosurgical intervention for PHVD on neuromonitoring data; (3) our neuroNICU evidence-based protocol for the management of PHVD. The overall goals of our protocol are to detect and treat PHVD early in order to minimize secondary brain injury and to better understand the effects of surgical treatments on neurodevelopmental outcomes and the pathophysiology of PHVD.
Surgical management of PHVD in prematurely born infants and outcomes
PHVD is usually detected by head ultrasound screening protocols in premature infants. The risk of PHVD increases with the severity of IVH (Papile grade),17 though ex vacuo ventricular dilation can have a larger contribution to PHVD with grade IV IVH (periventricular hemorrhagic infarction) due to cystic evolution resulting from the parenchymal injury. The rate of PHVD is lower in grade IV than grade III IVH, though the rate of cerebral palsy is higher in patients with grade IV than grade III IVH.18 Untreated progressive PHVD in infants causes progressive head growth across percentile lines and worsened cognitive and motor function, often resulting in severe disability or death.19,20 Treatments of PHVD conceptually fall into three categories: (1) Reduction of cerebrospinal fluid (CSF) production: diuretics (Lasix, acetazolamide), choroid plexus cauterization; (2) Diversion of CSF: lumbar puncture (LP), serial taps of an implanted ventricular reservoir, external ventricular drain, ventriculosubgaleal shunt, endoscopic third ventriculostomy (ETV); (3) Restoration of CSF absorption: clearance of blood and inflammatory products using intraventricular thrombolytics, neuroendoscopic lavage, or drainage of CSF via serial LP or reservoir taps.
Evidence-based guidelines for the management of posthemorrhagic hydrocephalus in premature infants were published in 2014 in the Journal of Neurosurgery Pediatrics,21 and one Level III recommendation regarding neuroendoscopic lavage (NEL) was added to the updated 2020 guidelines:22
-
1.
Level I evidence:
-
a.
Routine serial lumbar puncture is not recommended to reduce the need for VP shunt placement or to prevent the progression of hydrocephalus.
-
b.
Intraventricular thrombolytics are not recommended to reduce the need for shunt placement.
-
c.
Acetazolamide and furosemide are not recommended to reduce the need for shunt placement.
-
a.
-
2.
Level II:
-
a.
Ventricular access device (VAD), external ventricular drain, ventriculosubgaleal shunt, and lumbar puncture are treatment options but require clinical judgment. (Ventricular reservoir is a type of VAD.)
-
b.
Ventriculosubgaleal shunts reduce the need for daily CSF aspiration compared with VADs.
-
a.
-
3.
Level III:
-
a.
Evidence is insufficient to recommend a specific weight or CSF parameter to guide the timing of shunt placement.
-
b.
Evidence is insufficient to recommend endoscopic third ventriculostomy.
-
c.
Neuroendoscopic lavage is a feasible and safe option for the removal of intraventricular blood products and may lower the rate of shunt placement.23
-
a.
The lack of strong evidence for a particular surgical strategy has resulted in wide variability in management between institutions, from the choice of surgical temporization procedure, to shunt conversion rate, length of stay, and imaging modalities.15 Complications such as loculated hydrocephalus and shunt failure are more likely in children with PHVD than other congenital causes of hydrocephalus, with the complication risk (including infection) increasing with decreased gestational age and lower body weight at the time of VP shunt placement.1,24,25 Low birth weight infants with IVH who develop PHVD are usually treated with a temporary CSF diversion technique, such as serial taps of a ventricular reservoir,6,26,27 until they are large enough to receive a shunt (1.5–2.5 kg).28,29 The reported conversion rate of the ventricular reservoir to VP shunt ranges from 55 to 90%, without an increased infection rate with reservoirs relative to other temporization methods.15,27,28 Shunt revision rate may be lower in patients initially treated with reservoirs prior to shunt placement.30 Endoscopic third ventriculostomy (ETV) is another surgical approach designed to avoid shunt placement altogether, though its success rate is lower in PHVD than other hydrocephalus etiologies.31,32 A recent Cochrane Library systematic review found no proven reduction of death, disability, or permanent shunt placement with serial CSF removal via lumbar puncture or ventricular reservoir/ventricular tap.33
Studies comparing the relationship between specific surgical interventions, the timing of intervention, cerebral physiology, and neurodevelopmental outcomes are limited. A multi-institutional retrospective review of 127 preterm infants (<30 weeks) with PHVD classified management as “early approach” (procedural intervention with LP, ventricular reservoir, or VP shunt based on cranial ultrasound ventricular index > +2 SD and/or anterior horn width >6 mm) vs “late approach” (intervention based on clinical signs of increased ICP, most often shunt placement). The rates of shunt complication and infection were higher in the late approach cohort and neurodevelopmental outcomes were better in the early group. Early approach patients had similar neurocognitive outcomes independent of the need for intervention, and late approach patients had worse cognitive and motor outcomes than those without intervention,7 suggesting that early intervention based on ventricular measurements rather than clinical signs of increased ICP may lead to improved outcomes. This multi-institutional group then conducted a randomized controlled trial (ELVIS) of procedural intervention at low threshold (VI > 97 percentile and AHW > 6 mm and/or thalamo-occipital distance >25 mm) vs high threshold (VI > 97p + 4 mm and AHW > 10 mm). The study accrued 126 preterm infants (<34 weeks) with PHVD after Grades III–IV IVH, and found no difference in the rate of death or shunt placement between the two groups.34 The ELVIS trial composite outcome of death, cerebral palsy, or Bayley composite cognitive/motor scores < −2SD at 24 months corrected age occurred in 35% of the low threshold group and 51% of the high threshold group, and this difference was significant after adjusting for gestational age, IVH severity, and cerebellar hemorrhage.35 A subanalysis of the ELVIS data found larger ventricular volumes and more brain injury in the late intervention group.36 These findings support an early intervention threshold. It is interesting that the presence of a shunt did not correlate with worse outcomes within the early treatment group, suggesting that shunt placement is more likely a marker of disease severity than the cause of worse outcomes.35
When 70 preterm infants (24–34 weeks) with PHVD were randomized to either surgical drainage, irrigation, and fibrinolytic therapy (DRIFT) or serial tapping of a ventricular reservoir, there was no significant difference between the rate of shunt surgery or death, though DRIFT therapy resulted in a significantly higher rate of IVH (35% vs 8%).37 At two year follow up, a smaller proportion of DRIFT recipients had a severe cognitive disability, but sensorimotor disability was not significantly different,14 and the improved cognitive outcomes in the DRIFT group were maintained at 10 years.11 Neuroendoscopic lavage (NEL) for PHVD without fibrinolytic therapy was retrospectively evaluated in 56 premature infants from two institutions, with a 56.6% shunt rate, 63.5% 12-month shunt survival, and low complication rates (3.6% infection, 8.9% rehemorrhage).13 Neurodevelopmental outcomes at 2 years were assessed in 45 of these infants treated with NEL: 30% had normal cognitive development (vs 23% in the DRIFT study) and 44% had severe cognitive disability (vs 31% in DRIFT), though the walking ability was more difficult to directly compare and shunt rates were much different (60% NEL, 38% DRIFT).12
Studies of various surgical techniques and outcomes for the surgical management of PHVD are summarized in Table 1.
Perinatal CNS infection is so devastating to neurologic function that avoidance of post-surgical infection should be considered a primary surgical outcome measure. A study of the outcomes of neonatal meningitis in very low birth weight infants (<1.5 kg) found a 41% rate of major neurologic abnormality in meningitis survivors compared to 11% in those without meningitis after controlling for birth weight, IVH, chronic lung disease, and social risk factors.38 A series of children with myelomeningocele found a mean IQ of 104 for the 18 not-shunted children, 91 for the 41 children shunted without complications, and 70 for the 16 with shunts who had complications; one-half of the shunt complications were ventriculitis.39
A thorough review of PHVD pathophysiology and management was recently published by El-Dib, et al, with recommendations for risk-stratifying infants based on standardized ventricular measurements on cranial ultrasound and clinical signs. A strong case was made for early procedural intervention (LP, ventricular reservoir, ventriculosubgaleal shunt, or VP shunt) depending on risk category and patient characteristics. Pooled data showed a trend towards later treatment (larger ventricle size) and worse neurodevelopmental outcomes in North American vs European infants. Detailed comparisons of the cognitive, motor, and surgical outcomes of the prospective studies of PHVD management were tabulated.8
Neuromonitoring of prematurely born infants
Neuromonitoring covers a broad range of tools for evaluating brain growth and physiology. Below is a summary of monitoring modalities with relevant references.
-
1.
Physical exam: Though not quantitative, interrater reliability for the parameters “bulging fontanelle” and “split sutures” may be very accurate.40 However, physical exam findings occur late in the course of PHVD, and head circumference does not directly correlate with ventricle size.41
-
2.
Cranial ultrasound (CUS): A rapid, noninvasive, bedside test to visualize hemorrhage, measure ventricle size, and perform serial comparisons. Common measurements include: Ventricular Index (VI: distance from the lateral wall of the lateral ventricle to the midline, the coronal plane at the level of the foramen of Monro),42 Evans Ratio (ER: transverse bifrontal horn diameter:transverse internal diameter of the skull),43 and Anterior Horn Width (AHW). Thalamo-occipital distance (TOD) is measured in the parasagittal plane. Normal ranges for CUS measurements are published.44,45,46 Frontal and Temporal Horn Ratio (FTHR), and Frontal and Occipital Horn Ratio (FOHR) correlate well with ventricular volume and have good interobserver reliability.47,48 Multiple measurement types are useful because ventricle morphology can vary. CUS has a lower sensitivity for cerebellar hemorrhage, which is correlated with poorer outcomes.1,49 Though CUS is the most important diagnostic test for managing PHVD, ventricle size and head circumference do not correlate consistently, and surgical decisions ultimately depend on both clinical and imaging factors.41
-
3.
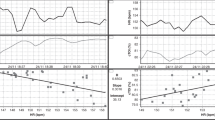
Transcranial doppler (TCD) ultrasound: Systolic and diastolic flow velocities, and the resistive index (RI = (V_peak.systole – V_end.diastole) / V_peak.systole), are commonly-used cerebral hemodynamic parameters. In theory, PHVD causes relatively higher ICP and decreased intracranial compliance, resulting in increased systolic velocity and lower end-diastolic velocity, thereby increasing RI.50 In general, TCDs are not a reliable noninvasive indicator of elevated ICP in infants with hydrocephalus,50 though changes in TCDs over time can be useful for detecting changes in cerebral hemodynamics due to ICP or other causes.51 Consistent changes in RI with temporary fontanelle compression and CSF drainage have been observed, and RI changes may be useful in measuring hemodynamic compensatory reserve when hydrocephalus is present.52 The time to normalization of TCD parameters after shunt placement may vary depending on the rapidity of hydrocephalus onset.53
-
4.
Magnetic resonance imaging (MRI): The most sensitive modality for detecting hemorrhage and prognosticating neurodevelopmental outcome. The developmental predictive yield of MRI at term estimated age (TEA) is increased in high-risk preterm infants (<29 weeks, <1000 g), and MRI is superior to CUS in detecting white matter injury, microhemorrhage (<3 mm), and cerebellar hemorrhage (1–3 mm).49 A methodology described by Kidokoro et al. for grading MRI findings based on white matter, ventricular, and anatomic findings correlates with worse memory and learning function at 7 years.54,55
-
5.
Electrophysiologic monitoring: Amplitude-integrated electroencephalography (aEEG) allows easier interpretation of general brain activity and continuous monitoring of neonatal encephalopathy by reducing the number of scalp electrodes and simplifying the output waveform relative to conventional EEG.56 The technique is not as sensitive as conventional EEG for detecting seizures,57 but is useful in the early management of hypoxic–ischemic encephalopathy and in predicting neurologic outcomes.58 Visual evoked potentials (VEP) monitor the electrical activity of the visual (occipital) cortex in response to a visual stimulus. In 17 infants with PHVD, 100% of VEP latencies were increased above the normal range, aEEG suppression was increased in 76%, and the patterns usually normalized within a week of external ventricular drain placement and continuous drainage,59 though these electrophysiologic changes were not consistently seen in another PHVD population.60 VEPs and brainstem auditory evoked potentials may be predictive of neurodevelopmental outcome in preterm infants, and can identify infants for early therapy and hearing interventions.61
-
6.
Noninvasive ICP measurement with a noninvasive anterior fontanelle pressure transducer: Elevated ICP is a late derangement in progressive PHVD. Tapping a ventricular reservoir reduced non-invasively-measured ICP in a series of 6 premature infants with PHVD with frank signs of hydrocephalus who eventually underwent shunt surgery, but ICP measurements varied widely despite open fontanelles and sutures.62 Anterior fontanelle pressure did not directly correlate with clinical signs of raised ICP in another study of 37 hydrocephalic infants.63
-
7.
Near-infrared spectroscopy (NIRS): NIRS non-invasively measures spectrophotometric properties of oxyhemoglobin and deoxyhemoglobin to calculate cerebral oxygen saturation and fractional cerebral oxygen extraction, and to assess cerebral autoregulation through analysis of its correlation with systemic blood pressure.64 Assuming constant oxygen saturation of afferent cerebral blood and constant global cerebral metabolic rate over the measurement period, changes in cerebral blood flow correlate with changes in oxyhemoglobin and deoxyhemoglobin.65,66 Impaired autoregulation correlates with cerebral hemorrhage,67 and delayed cord clamping after birth results in improved autoregulation and reduced IVH.68 Multiple studies have found correlations between features of cerebral NIRS data within the first few days after birth and the development of IVH.10,69,70,71 PDA is associated with a higher risk of IVH,72 though a PDA can affect NIRS values.73 A study of 185 infants born before 30 weeks found an association between IVH and persistent cerebral desaturation (68 days), and between white matter injury and persistently increased cerebral oxygen extraction (45 days).74 Necrotizing enterocolitis is associated with worse neurodevelopmental outcomes, independent of cerebral hemorrhage, and a study of 48 infants (<30 weeks) followed with weekly NIRS measurements until 36 weeks postconceptual age found lower tissue oxygenation index in the 6 infants who developed NEC and had no cerebral hemorrhage.75 Cerebral NIRS monitored in congenital heart surgery suggests a correlation with neurologic outcomes.76 There are multiple recent (and ongoing) prospective studies evaluating cerebral NIRS for prognostication in premature infants.77,78,79
-
8.
Standardized neurologic exams: The Hammersmith Neonatal (and infant) Neurological Exams,80,81 the Neonatal Intensive Care Unit Network Neurobehavioral Scale,82 and Prechtl’s General Movements Assessment83 track nervous system development, are associated with long term motor, cognitive, and behavioral outcomes, and have generated normative data.84 Serial neurodevelopmental assessments such as the Bayley Scales of Infant and Toddler Development (BSID-III, IV),85 the British Ability Scales,86 Griffiths Mental Development Scales,87 and Wechsler scales88 are commonly-used measures of cognitive development. The Child Behavior Checklist-parent report (CBCL) profiles behavior and social functioning relative to age and sex.89
Effects of neurosurgical intervention on neuromonitoring data in PHVD
A limited number of recent studies exist that directly assess the effects of neurosurgical intervention for PHVD on cerebral physiology, and neurodevelopmental correlations have not yet been evaluated. Following are some representative examples that study the effects of CSF removal on NIRS and TCD data.
In a comparison of 20 premature infants (birth weight < 1500 g and grades III or IV IVH) with 12 infants with normal or mild IVH (Grade I or II), lower cerebral oxygen saturation and higher oxygen extraction were associated with progressive PHVD.90 Nine prematurely born infants with PHVD who underwent EVD placement for signs of increased ICP were monitored with combinations of TCD, regional cerebral oxygen saturation (rcSO2), aEEG, and VEP. The rcO2, aEEG, and VEP improved significantly after ventricular decompression, though the resistive index did not change.91 In 7 prematurely born infants with PHVD and ventricular reservoirs, CSF removal resulted in durable improvement in cerebral oxygenation and hemodynamics after reservoir taps at post-operative days 1, 3–4, and 7–9.92 Improvement in CBF was seen in another study of 9 infants with PHVD managed with ventricular taps, but cerebral oxygen metabolism was not affected.93 A device combining NIRS and diffuse correlation spectroscopy to measure CBF, tissue oxygen saturation, and the oxidation state of cytochrome c oxidase (oxCCO) was applied to four patients with PHVD and found small improvements in CBF and oxCCO after ventricular taps.94 Though NIRS and TCD data usually become deranged relatively late in the course of PHVD, the references in the NIRS neuromonitoring section above suggest that there may be measurable, relevant differences in NIRS data outside of late-stage PHVD that could ultimately correlate with developmental outcomes, but this requires further study.
Proposed evidence-based NICU neuromonitoring algorithm
Our monitoring protocol for infants born before 32 weeks is shown in Fig. 1, and our protocol for surgically treated PHVD is shown in Fig. 2. The goal of the protocol is to identify PHVD and intervene early, while prospectively and non-invasively collecting physiologic data to correlate with the effect of interventions on neurodevelopmental outcome. The neonatal neurology team is consulted when severe IVH (grade III or IV) is detected, and follows these neonates throughout their admission to monitor the neurological exam, to monitor for signs of seizures (EEG if there are clinical signs), and to maintain an ongoing discussion with families regarding neurodevelopmental prognosis, continuing with outpatient follow up.
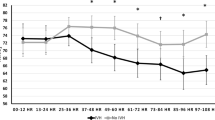
All preterm infants undergo CUS, TCD, and 72 h of NIRS recording within the first 3 days of birth, 10–14 days, 28–30 days, and TEA. New IVH, or AHW > 6 mm and VI > 97th percentile, or physical signs of increased intracranial pressure, trigger twice-weekly CUS and doppler studies, NIRS for 24–72 h, and neurosurgical consultation. Infants <2 kg with progressive PHVD are treated with serial taps of an implanted ventricular reservoir, with the goal of reducing but not fully collapsing the ventricles. To minimize infection risk, the reservoir is implanted in the operating room, a single preoperative dose of prophylactic antibiotics is administered, and careful technique with a wide sterile field, masks, and sterile gloves are used during reservoir taps in the NICU. Taps are stopped when 2 kg is reached. If the ventricle size increases, the reservoir is replaced with a VP shunt with 24–72 h NIRS before the procedure and 1–2 weeks later. If there is no progression over two weeks, CUS frequency is reduced to once weekly until TEA, and outpatient neurosurgical follow-up continues for at least 2–3 years in the absence of progression.
CUS reports include a resistive index, maximum and minimum flow velocities, and ventricular measurements (VI, AHW, TOD), and the measurements are plotted. NIRS measurements are recorded weekly over 24–72 h periods, and include cerebral oxygen saturation, CBV, cerebral vasoreactivity (a marker of autoregulation), and fractional O2 extraction. We follow our published evidence-based CUS and term-equivalent age MRI protocol that risk-stratifies premature infants according to gestational age (<29 weeks) and birth weight (<1000 g).49
NICU graduates with EGA < 30 weeks at birth are followed until age 5 years in the NICU comprehensive “Thrive” clinic, staffed by a developmental specialist, dedicated pediatrician, psychologist, social worker, and dietician, who provide routine well-child care, acute care, 24-h access to a primary caregiver, and periodic neurodevelopmental evaluations. Use of the “Thrive” model significantly reduced life-threatening illnesses for very low birth weight infants between nursery discharge and 1 year compared to routine follow-up care.95 Serial neurologic examinations, biomarkers (NIRS, Doppler), and neuroimaging before hospital discharge, coupled with standardized longitudinal follow-up based on comprehensive evidence-based neurodevelopmental guidelines, allows the most accurate prognostication, early identification of disabilities, and early intervention in order to achieve the best long term outcomes.96,97,98,99
Conclusion
The optimal neurodevelopmental outcome is the most important ultimate goal of PHVD management, but surgical management of this condition and reported outcomes vary considerably. Current evidence suggests that better outcomes are achieved through early detection of PHVD and early timing of surgical intervention based on standardized ventricle measurements with CUS, before advanced ventricle dilation or physical signs of increased ICP develop. However, ventricular measurements are the macroscopic result of a complex physiologic process. The systematic use of multimodal neuromonitoring including NIRS and TCD in the care of premature infants with PHVD has the potential to lead to a better physiologic understanding of the effect of surgical treatment on cerebral physiology and neurodevelopmental outcomes.
Recommendations
Due to the heterogeneity of comorbid conditions and initial treatments at referring institutions, PHVD severity at presentation and best initial surgical treatment options vary. This makes it challenging to exactly follow the same protocol for all infants. The principles of the algorithm should be applied with the goal of early detection and intervention for PVHD, which the collaboration of a multidisciplinary team. Surgical treatment should proceed when the CUS and clinical thresholds for early intervention are met, rather than waiting for NIRS and TCD derangements, which may not occur until later in the course of untreated PHVD. A standardized protocol will allow for the comparison of neuromonitoring data across a range of PHVD stages and surgical treatments. Further improvement in the treatment of PHVD will come from the systematic prospective study of physiologic monitoring data, and the incorporation of standardized neurodevelopmental assessments as surgical outcome measures.
References
Robinson, S. Neonatal posthemorrhagic hydrocephalus from prematurity: pathophysiology and current treatment concepts: a review. J. Neurosurg. Pediatr. 9, 242–258 (2012).
Plessis, A. Jdu The role of systemic hemodynamic disturbances in prematurity-related brain injury. J. Child Neurol. 24, 1127–1140 (2009).
Christian, E. A. et al. Trends in hospitalization of preterm infants with intraventricular hemorrhage and hydrocephalus in the United States, 2000-2010. J. Neurosurg. Pediatr. 17, 260–269 (2016).
Horbar, J. D. et al. Trends in mortality and morbidity for very low birth weight infants, 1991-1999. Pediatrics 110, 143–151 (2002).
Murphy, B. P. et al. Posthaemorrhagic ventricular dilatation in the premature infant: Natural history and predictors of outcome. Arch. Dis. Child. Fetal Neonatal Ed. 87, F37–F41 (2002).
Whitelaw, A. & Aquilina, K. Management of posthaemorrhagic ventricular dilatation. Arch. Dis. Child. Fetal Neonatal Ed. 97, 229–233 (2012).
Leijser, L. M. et al. Posthemorrhagic ventricular dilatation in preterm infants When best to intervene? Neurology 90, E698–E706 (2018).
El-Dib, M. et al. Management of post-hemorrhagic ventricular dilatation in the infant born preterm. J. Pediatr. 226, 16–27.e3 (2020).
Whitelaw, A., Pople, I., Cherian, S., Evans, D. & Thoresen, M. Phase 1 trial of prevention of hydrocephalus after intraventricular hemorrhage in newborn infants by drainage, irrigation, and fibrinolytic therapy. Pediatrics 111, 759–766 (2003).
Noori, S., McCoy, M., Anderson, M. P., Ramji, F. & Seri, I. Changes in cardiac function and cerebral blood flow in relation to peri/intraventricular hemorrhage in extremely preterm infants. J. Pediatr. 164, 264–270.e3 (2014).
Luyt, K. et al. Drainage, irrigation and fibrinolytic therapy (DRIFT) for posthaemorrhagic ventricular dilatation: 10-year follow-up of a randomised controlled trial. Arch. Dis. Child. Fetal Neonatal Ed. 105, 466–473 (2020).
Behrens, P. et al. Neurodevelopmental outcome at 2 years after neuroendoscopic lavage in neonates with posthemorrhagic hydrocephalus. J. Neurosurg. Pediatr. 26, 465–602 (2020).
D’Arcangues, C. et al. Extended experience with neuroendoscopic lavage for posthemorrhagic hydrocephalus in neonates. World Neurosurg. 116, e217–e224 (2018).
Whitelaw, A. et al. Randomized trial of drainage, irrigation and fibrinolytic therapy for premature infants with posthemorrhagic ventricular dilatation: developmental outcome at 2 years. Pediatrics 125, e852–e858 (2010).
Wellons, J. C. I. et al. Shunting outcomes in posthemorrhagic hydrocephalus: results of a Hydrocephalus Clinical Research Network prospective cohort study. J. Neurosurg. Pediatr. 20, 19–29 (2017).
Koschnitzky, J. E. et al. Opportunities in posthemorrhagic hydrocephalus research: outcomes of the Hydrocephalus Association Posthemorrhagic Hydrocephalus Workshop. Fluids Barriers CNS 15, 1–22 (2018).
Papile, L. A., Burstein, J., Burstein, R. & Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: A study of infants with birth weights less than 1,500 gm. J. Pediatr. 92, 529–534 (1978).
Brouwer, A. et al. Neurodevelopmental outcome of preterm infants with severe intraventricular hemorrhage and therapy for post-hemorrhagic ventricular dilatation. J. Pediatr. 152, 648–654 (2008).
Laurence, K. M. & Coates, S. The natural history of hydrocephalus: detailed analysis of 182 unoperated cases. Arch. Dis. Child. 37, 345–362 (1962).
Weller, R. O. & Shulman, K. Infantile hydrocephalus: clinical, histological, and ultrastructural study of brain damage. J. Neurosurg. 36, 255–265 (1972).
Mazzola, C. A. et al. Pediatric hydrocephalus: systematic literature review and evidence-based guidelines. Part 2: Management of posthemorrhagic hydrocephalus in premature infants. J. Neurosurg. Pediatr. 14, 8–23 (2014).
Bauer, D. F. et al. Congress of Neurological Surgeons Systematic Review and Evidence-Based Guidelines on the Treatment of Pediatric Hydrocephalus: update of the 2014 guidelines. Neurosurgery 87, 1071–1075 (2020).
Schulz, M., Buḧrer, C., Pohl-Schickinger, A., Haberl, H. & Thomale, U. W. Neuroendoscopic lavage for the treatment of intraventricular hemorrhage and hydrocephalus in neonates: clinical article. J. Neurosurg. Pediatr. 13, 626–635 (2014).
Taylor, A. G. & Peter, J. C. Advantages of delayed VP shunting in post-haemorrhagic hydrocephalus seen in low-birth-weight infants. Child’s Nerv. Syst. 17, 328–333 (2001).
James, H. E. et al. Ventriculoperitoneal shunts in high risk newborns weighing under 2000 grams: a clinical report. Neurosurgery 15, 198–202 (1984).
Zaben, M., Finnigan, A., Bhatti, M. I. & Leach, P. The initial neurosurgical interventions for the treatment of posthaemorrhagic hydrocephalus in preterm infants: a focused review. Br. J. Neurosurg. 30, 7–10 (2016).
Christian, E. A., Melamed, E. F., Peck, E., Krieger, M. D. & McComb, J. G. Surgical management of hydrocephalus secondary to intraventricular hemorrhage in the preterm infant. J. Neurosurg. Pediatr. 17, 278–284 (2016).
Shankaran, S. et al. Outcomes following post-hemorrhagic ventricular dilatation among infants of extremely low gestational age. J. Pediatr. 226, 36–44.e3 (2020).
Brouwer, A. J. et al. Cognitive and neurological outcome at the age of 5-8 years of preterm infants with post-hemorrhagic ventricular dilatation requiring neurosurgical intervention. Neonatology 101, 210–216 (2012).
Willis, B. et al. Ventricular reservoirs and ventriculoperitoneal shunts for premature infants with posthemorrhagic hydrocephalus: an institutional experience. J. Neurosurg. Pediatr. 3, 94–100 (2009).
Warf, B. C., Campbell, J. W. & Riddle, E. Initial experience with combined endoscopic third ventriculostomy and choroid plexus cauterization for post-hemorrhagic hydrocephalus of prematurity: The importance of prepontine cistern status and the predictive value of FIESTA MRI imaging. Child’s Nerv. Syst. 27, 1063–1071 (2011).
Chamiraju, P., Bhatia, S., Sandberg, D. I. & Ragheb, J. Endoscopic third ventriculostomy and choroid plexus cauterization in posthemorrhagic hydrocephalus of prematurity. J. Neurosurg. Pediatr. 13, 433–439 (2014).
Whitelaw, A. & Lee-Kelland, R. Repeated lumbar or ventricular punctures in newborns with intraventricular haemorrhage. Cochrane Database Syst. Rev. 4, CD000216 (2017).
Vries, L. S. De et al. Treatment thresholds for intervention in posthaemorrhagic ventricular dilation: a randomised controlled trial. Arch. Dis. Child Fetal Neonatal Ed. 104, F70–F75 (2019).
Cizmeci, M. N. et al. Randomized controlled early versus late intervention study in posthemorrhagic ventricular dilation: outcome at 2 years. J. Pediatr. 226, 28–e35.3 (2020).
Cizmeci, M. N. et al. Assessment of brain injury and brain volumes after posthemorrhagic ventricular dilatation: a nested substudy of the randomized controlled ELVIS trial. J. Pediatr. 208, 191–197.e2 (2019).
Whitelaw, A. et al. Randomized clinical trial of prevention of hydrocephalus after intraventricular hemorrhage in preterm infants: brain-washing versus tapping fluid. Pediatrics 119, e1071–e1078 (2007).
Doctor, B. A. et al. Clinical outcomes of neonatal meningitis in very-low-birth-weight infants. Clin. Pediatr. 40, 473–480 (2001).
Mapstone, T. B. et al. Relationship of CSF shunting and IQ in children with myelomeningocele: a retrospective analysis. Childs Brain 11, 112–118 (1984).
Wellons, J. C. et al. The assessment of bulging fontanel and splitting of sutures in premature infants: An interrater reliability study by the Hydrocephalus Clinical Research Network - Clinical article. J. Neurosurg. Pediatr. 11, 12–14 (2013).
Ingram, M. C. E., Huguenard, A. L., Miller, B. A. & Chern, J. J. Poor correlation between head circumference and cranial ultrasound findings in premature infants with intraventricular hemorrhage: clinical article. J. Neurosurg. Pediatr. 14, 184–189 (2014).
Levene, M. I. Measurement of the growth of the lateral ventricles in preterm infants with real-time ultrasound. Arch. Dis. Child. 56, 900–904 (1981).
Evans, W. A. Jr An encephalographic ratio for estimating ventricular enlargement and cerebral atrophy. Arch. Neurol. Psychiatry 47, 931–937 (1942).
Davies, M. W., Swaminathan, M., Chuang, S. L. & Betheras, F. R. Reference ranges for the linear dimensions of the intracranial ventricles in preterm neonates. Arch. Dis. Child. Fetal Neonatal Ed. 82, 218–223 (2000).
Brouwer, M. J. et al. New reference values for the neonatal cerebral ventricles. Radiology 262, 224–233 (2012).
Levene, M. I. & Starte, D. R. A longitudinal study of post-haemorrhagic ventricular dilatation in the newborn. Arch. Dis. Child. 56, 905–910 (1981).
Radhakrishnan, R. et al. Frontal occipital and frontal temporal horn ratios: comparison and validation of head ultrasound- derived indexes with MRI and ventricular volumes in infantile ventriculomegaly. Am. J. Roentgenol. 213, 925–931 (2019).
Kulkarni, A. V., Drake, J. M., Armstrong, D. C. & Dirks, P. B. Measurement of ventricular size: Reliability of the frontal and occipital horn ratio compared to subjective assessment. Pediatr. Neurosurg. 31, 65–70 (1999).
Ibrahim, J., Mir, I. & Chalak, L. Brain imaging in preterm infants < 32 weeks gestation: a clinical review and algorithm for the use of cranial ultrasound and qualitative brain MRI. Pediatr. Res. 84, 799–806 (2018).
Hanlo, P. W. et al. Value of transcranial Doppler indices in predicting raised ICP in infantile hydrocephalus: a study with review of the literature. Child’s Nerv. Syst. 11, 595–603 (1995).
Cardim, D. et al. Non-invasive monitoring of intracranial pressure using transcranial doppler ultrasonography: is it possible? Neurocrit. Care 25, 473–491 (2016).
Taylor, G. A. & Madsen, J. R. Neonatal hydrocephalus: Hemodynamic response to fontanelle compression—correlation with intracranial pressure and need for shunt placement. Radiology 201, 685–689 (1996).
Sanker, P., Richard, K. E., Weigl, H. C., Klug, N. & van Leyen, K. Transcranial Doppler sonography and intracranial pressure monitoring in children and juveniles with acute brain injuries or hydrocephalus. Child’s Nerv. Syst. 7, 391–393 (1991).
Kidokoro, H., Neil, J. J. & Inder, T. E. New MR imaging assessment tool to define brain abnormalities in very preterm infants at term. Am. J. Neuroradiol. 34, 2208–2214 (2013).
Omizzolo, C. et al. Hippocampal volume and memory and learning outcomes at 7 years in children born very preterm. J. Int. Neuropsychol. Soc. 19, 1065–1075 (2013).
Glass, H. C. & Wusthoff, C. J. Amplitude integrated EEG: the child neurologist’s perspective. J. Child Neurol. 28, 1342–1350 (2013).
Rakshasbhuvankar, A. et al. for detection of neonatal seizures: a systematic review. Seizure 33, 90–98 (2015).
Chandrasekaran, M., Chaban, B., Montaldo, P. & Thayyil, S. Predictive value of amplitude-integrated EEG (aEEG) after rescue hypothermic neuroprotection for hypoxic ischemic encephalopathy: a meta-analysis. J. Perinatol. 37, 684–689 (2017).
Klebermass-Schrehof, K. et al. Can neurophysiological assessment improve timing of intervention in posthaemorrhagic ventricular dilatation? Arch. Dis. Child. Fetal Neonatal Ed. 98, 291–297 (2013).
De Vries, L. S., Brouwer, A. J. & Groenendaal, F. Posthaemorrhagic ventricular dilatation: When should we intervene? Arch. Dis. Child. Fetal Neonatal Ed. 98, 284–285 (2013).
Shepherd, A. J., Saunders, K. J., McCulloch, D. L. & Dutton, G. N. Prognostic value of flash visual evoked potentials in preterm infants. Dev. Med. Child Neurol. 41, 9–15 (1999).
Behmanesh, B. et al. First clinical experience with the new noninvasive transfontanelle ICP monitoring device in management of children with premature IVH. Neurosurg. Rev. 43, 681–685 (2019).
Hanlo, P. W. et al. Relationship between anterior fontanelle pressure measurements and clinical signs in infantile hydrocephalus. Child’s Nerv. Syst. 12, 200–209 (1996).
Rhee, C. J. et al. Neonatal cerebrovascular autoregulation. Pediatr. Res. 84, 602–610 (2018).
Dempsey, E. M., Kooi, E. M. W. & Boylan, G. It’s all about the brain—neuromonitoring during newborn transition. Semin. Pediatr. Neurol. 28, 48–59 (2019).
Lloyd-Fox, S., Blasi, A. & Elwell, C. E. Illuminating the developing brain: The past, present and future of functional near infrared spectroscopy. Neurosci. Biobehav. Rev. 34, 269–284 (2010).
O’Leary, H. et al. Elevated cerebral pressure passivity is associated with prematurity-related intracranial hemorrhage. Pediatrics 124, 302–309 (2009).
Vesoulis, Z. A., Liao, S. M. & Mathur, A. M. Delayed cord clamping is associated with improved dynamic cerebral autoregulation and decreased incidence of intraventricular hemorrhage in preterm infants. J. Appl. Physiol. 127, 103–110 (2019).
Sortica da Costa, C. et al. Complexity of brain signals is associated with outcome in preterm infants. J. Cereb. Blood Flow. Metab. 37, 3368–3379 (2017).
Cimatti, A. G. et al. Cerebral oxygenation and autoregulation in very preterm infants developing IVH during the transitional period: a pilot study. Front. Pediatr. 8, 1–8 (2020).
Sortica da Costa, C. et al. Changes in hemodynamics, cerebral oxygenation and cerebrovascular reactivity during the early transitional circulation in preterm infants. Pediatr. Res. 86, 247–253 (2019).
Khanafer-Larocque, I. et al. Intraventricular hemorrhage: risk factors and association with patent ductus arteriosus treatment in extremely preterm neonates. Front. Pediatr. 7, 1–9 (2019).
Arman, D. et al. The association between NIRS and Doppler ultrasonography in preterm infants with patent ductus arteriosus. J. Matern. Neonatal Med. 33, 1245–1252 (2020).
Vesoulis, Z. A., Whitehead, H. V., Liao, S. M. & Mathur, A. M. The hidden consequence of intraventricular hemorrhage: persistent cerebral desaturation after IVH in preterm infants. Pediatr. Res. 1–9, https://doi.org/10.1038/s41390-020-01189-5 (2020).
Howarth, C. et al. Cerebral oxygenation in preterm infants with necrotizing enterocolitis. Pediatrics 146, e20200337 (2020).
Oliveira, S. R. De et al. Near-infrared spectroscopy as an auxiliary tool in the study of child development. Rev. Paul. Pediatr. 33, 230–240 (2015).
Hansen, M. L. et al. Cerebral near-infrared spectroscopy monitoring versus treatment as usual for extremely preterm infants: a protocol for the SafeBoosC randomised clinical phase III trial. Trials 20, 1–11 (2019).
Katheria, A. C. et al. The neu-prem trial: neuromonitoring of brains of infants born preterm during resuscitation—a prospective observational cohort study. J. Pediatr. 198, 209–213.e3 (2018).
Chock, V. Y. et al. Cerebral oxygenation and autoregulation in preterm infants (Early NIRS Study). J. Pediatr. 227, 94–100.e1 (2020).
Haataja, L. et al. Optimality score for the neurologic examination of the infant at 12 and 18 months of age. J. Pediatr. 135, 153–161 (1999).
Dubowitz, L., Dubowitz, V., Palmer, P. & Verghote, M. A new approach to the neurological assessment of the preterm and full-term newborn infant. Brain Dev. 2, 3–14 (1980).
Lester, B. M., Tronick, E. Z. & Brazelton, T. B. The neonatal intensive care unit network neurobehavioral scale (NNNS): introduction. Pediatrics 113, 641–667 (2004).
Einspieler, C. & Prechtl, H. F. R. Prechtl’s assessment of general movements: a diagnostic tool for the functional assessment of the young nervous system. Ment. Retard. Dev. Disabil. Res. Rev. 11, 61–67 (2005).
Spittle, A. J. et al. Neurobehaviour and neurological development in the first month after birth for infants born between 32-42 weeks’ gestation. Early Hum. Dev. 96, 7–14 (2016).
Bayley, N. & Aylward, G. P. Bayley Scales of Infant and Toddler Development (2019).
Elliot, C. & Smith, P. British Ability Scales (2012).
Griffiths, R. The abilities of young children: a comprehensive system of mental measurement for the first eight years of life (1984).
Wechsler, D. Wechsler Intelligence Scale for Children (2003).
Achenbach, T. & Rescorla, L. Manual for the ASEBA Preschool Forms & Profiles (2000).
Kochan, M. et al. Changes in cerebral oxygenation in preterm infants with progressive posthemorrhagic ventricular dilatation. Pediatr. Neurol. 73, 57–63 (2017).
Norooz, F. et al. Decompressing posthaemorrhagic ventricular dilatation significantly improves regional cerebral oxygen saturation in preterm infants. Acta Paediatr. Int. J. Paediatr. 104, 663–669 (2015).
van Alfen-van der Velden, A. A. E. M. et al. Cerebral hemodynamics and oxygenation after serial CSF drainage in infants with PHVD. Brain Dev. 29, 623–629 (2007).
McLachlan, P. J. et al. Investigating the effects of cerebrospinal fluid removal on cerebral blood flow and oxidative metabolism in infants with post-hemorrhagic ventricular dilatation. Pediatr. Res. 82, 634–641 (2017).
Rajaram, A. et al. Perfusion and metabolic neuromonitoring during ventricular taps in infants with post-hemorrhagic ventricular dilatation. Brain Sci. 10, 1–13 (2020).
Broyles, R. S. et al. Comprehensive follow-up care and life-threatening illnesses among high-risk infants, a randomized controlled trial. JAMA 284, 2070–2076 (2000).
Benninger, K. L. et al. Perspectives from the Society for Pediatric Research. Neonatal encephalopathy clinical trials: developing the future. Pediatr. Res. 89, 74–84 (2021).
Maitre, N. L. et al. Network implementation of guideline for early detection decreases age at cerebral palsy diagnosis. Pediatrics 145, e20192126 (2020).
Novak, I. et al. Early, accurate diagnosis and early intervention in cerebral palsy: Advances in diagnosis and treatment. JAMA Pediatr. 171, 897–907 (2017).
Spittle, A., Orton, J., Anderson, P. J., Boyd, R. & Doyle, L. W. Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database Syst. Rev. 11, CD005495 (2015).
Ventriculomegaly Trial Group. Randomised trial of early tapping in neonatal posthaemorrhagic ventricular dilatation. Arch. Dis. Child 65, 3–10 (1990).
Ventriculomegaly Trial Group. Randomised trial of early tapping in neonatal post haemorrhagic ventricular dilatation: results at 30 months. Arch. Dis. Child. Fetal Neonatal Ed. 70, F129–F136 (1994).
Kulkarni, A. V. et al. Endoscopic third ventriculostomy and choroid plexus cauterization in infants with hydrocephalus: a retrospective Hydrocephalus Clinical Research Network study. J. Neurosurg. Pediatr. 14, 224–229 (2014).
Srinivasakumar, P. et al. Posthemorrhagic ventricular dilatation-impact on early neurodevelopmental outcome. Am. J. Perinatol. 30, 207–213 (2013).
Acknowledgements
L.C. is supported by NIH grant 1R01NS102617-01.
Author information
Authors and Affiliations
Contributions
B.A.W.: conception, design, acquisition and interpretation of information, drafting and revision, and final approval. D.M.S.: critical revision and final approval. J.T.: drafting and critical revision, and final approval. L.C.: conception, design, acquisition and interpretation of information, drafting and revision, and final approval.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Whittemore, B.A., Swift, D.M., M. Thomas, J. et al. A neonatal neuroNICU collaborative approach to neuromonitoring of posthemorrhagic ventricular dilation in preterm infants. Pediatr Res 91, 27–34 (2022). https://doi.org/10.1038/s41390-021-01406-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01406-9
This article is cited by
-
Spontaneous resolution of post-hemorrhagic ventricular dilatation in preterm newborns and neurodevelopment
Pediatric Research (2023)
-
Degree of ventriculomegaly predicts school-aged functional outcomes in preterm infants with intraventricular hemorrhage
Pediatric Research (2022)
-
Ventriculomegaly thresholds for prediction of symptomatic post-hemorrhagic ventricular dilatation in preterm infants
Pediatric Research (2022)