Abstract
Background
The aim of this study was to understand the challenges experienced by families obtaining a diagnosis and therapy for developmental coordination disorder (DCD).
Methods
Parents of 435 children aged 4–18 years with persistent motor difficulties consistent with a diagnosis of DCD completed an online survey. Diagnostic timeline and diagnostic label/s received were examined, along with therapies accessed.
Results
There was inconsistent diagnostic terminology (nine separate terms) with more children diagnosed with dyspraxia (64.7%) than DCD (48.8%). Even though most parents (87.0%) reported that receiving a diagnosis was helpful, children did not receive a diagnosis until years after seeking help (mean 2.8 ± 2.3 years). Many children were diagnosed with at least one co-occurring neurodevelopmental, language or learning disorder (70.0%). Almost all families had accessed therapy for their child’s movement difficulties (93.9%), but more than half did not have access to funding to support therapy costs (57.8%) and reported that the costs caused financial strain (52.6%). Two out of every three families reported that they did not feel the current level of therapy was sufficient.
Conclusions
This critical advocacy research highlights inconsistent and incorrect terminology and the challenges families experience in obtaining a diagnosis and adequate access to therapy for their child’s movement difficulties.
Impact
-
This is the first comprehensive study to examine the challenges families experience gaining a diagnosis and therapy for their child with DCD.
-
Families regularly experienced prolonged diagnosis; 45% waited between 2 and 4 years.
-
There is no clear diagnostic pathway, with children more likely to be diagnosed with dyspraxia than the correct clinical diagnosis of DCD.
-
More extensive implementation of the diagnostic guidelines into clinical practice is needed.
Similar content being viewed by others
Introduction
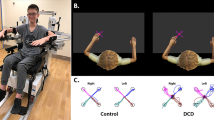
For over 30 years, developmental coordination disorder (DCD) has appeared as a neurodevelopmental disorder within diagnostic manuals.1,2,3,4,5 Classed as a motor disorder, diagnosis currently requires meeting four diagnostic criteria, including (i) impaired ability to acquire and execute motor skills at an age-appropriate level, (ii) significant interference with activities of daily living, academic productivity, leisure and play, (iii) onset early in the developmental period and (iv) the movement difficulties are not better explained by intellectual disability, visual impairment or other neurological conditions affecting movement.1 The disorder affects approximately one in every 20 school-aged children.1
Despite its relatively high prevalence, DCD remains under-recognised and under-supported.6,7 This reflects a combination of factors. The diagnostic terminology is inconsistent, with DCD used synonymously with terms such as dyspraxia and motor delay.8 Unlike a condition such as cerebral palsy, where a symptom like spasticity can be highly visible, the symptoms of DCD are less overt, and as a result, can be perceived to impact functioning to a lesser extent than other movement-related conditions. This is despite the substantial impact on physical, social and emotional health.9,10,11,12 DCD also frequently co-occurs with other neurodevelopmental disorders (e.g. autism (ASD)13 and attention deficit hyperactivity disorder (ADHD)14); however, it is often overlooked because movement difficulties sit outside the diagnostic frameworks for these disorders and are not typically included within the evaluation process. While there have been recent efforts to improve the identification, diagnosis and delivery of evidence-based interventions for children with DCD (e.g. 6), implementation is lacking. At present, there is limited data to demonstrate to key stakeholders, such as clinicians and policymakers why there is a critical need to start practice.
In recent years, there has been an increase in advocacy research to demonstrate the systemic lack of awareness and support for DCD. Previous evidence suggests the clinical pathway is difficult to navigate for caregivers of children with DCD.15 Limited knowledge of DCD by medical professionals has been highlighted in recent research with Wilson et al.16 reporting that only 23% of family physicians and 41% of paediatricians familiar with the label DCD in Canada, United States and the United Kingdom, and in a much smaller sample of Australian medical professionals (paediatricians, general practitioners and a registered nurse), Hunt et al.17 reported 52% of medical professionals are familiar with the label DCD. Increased familiarity with the label dyspraxia was reported in these studies, with 61% of paediatricians familiar with the label dyspraxia across Canada, United States and the United Kingdom16 and 82% of medical professionals familiar with the label dyspraxia in Australia.17 This is in spite of dyspraxia being a label not currently recognised as a discrete diagnosis or appearing in internationally recognised diagnostic manuals. Dyspraxia is also a term that is used to ‘describe’ impaired movement (‘dys-’: dysfunction; ‘-praxia’: movement) rather than a diagnosis18 and has been used to describe generalised movement impairments in other conditions (e.g. Down syndrome, Parkinson’s disease, Alzheimer’s disease and stroke).19,20,21,22,23
Karkling et al.24 evaluated the knowledge of occupational therapists in Canada, revealing that more than a third of these professionals, who play an integral role in the assessment and therapy for people with DCD, were not familiar with the diagnostic guidelines for DCD. Knowledge within the education system is also lacking. Wilson et al.16 reported that only 23% of Canadian school teachers are familiar with the diagnostic label DCD, compared to 96% of school teachers being familiar with ADHD and 92% familiar with ASD. Similar findings were recently reported in Australia, with 35% of teachers familiar with the diagnostic label DCD, compared to 94% being familiar with ADHD and 98% familiar with ASD.17 With such low rates of knowledge and awareness of DCD among medical, allied health and educational professionals, it is unsurprising that families raising children who meet the criteria for this disorder feel frustrated and unsupported.
While demonstrating the lack of knowledge and awareness by professionals is an important component of advocacy research, an equally important aspect is the lived experience of families. Studies examining the parental experience are limited but reveal that parental concerns are often disregarded by medical professionals, with parents often told their child will most likely ‘grow out of it’.25 These challenges result in children with DCD falling through the gaps of healthcare systems worldwide, causing families considerable stress.26 The lived experience of families in relation to accessing care for their child with DCD is largely unknown. There is a critical need for large-scale research efforts to identify areas in which families experience the greatest challenges and to advocate for change. The primary aim of the present study was to describe the development and delivery of a survey (Impact for DCD) and present diagnostic and service provision findings.
Methods
Participants
Primary caregivers of children and adolescents aged 4–18 years in Australia with persistent movement difficulties, consistent with a diagnosis of DCD and synonymous labels (e.g., dyspraxia, motor dyspraxia, motor delay), were invited to complete the Impact for DCD survey.
Survey
The Impact for DCD survey27 incorporated a mixed-methods design, developed in collaboration with parent, educator and clinician consultation groups, along with Australia’s family advocacy group, DCD Australia Incorporated. The survey consisted of 95 multiple-choice and open-ended questions to allow for both quantitative and qualitative investigations. Questions were clustered across five impact domains: (1) diagnosis; (2) therapy; (3) activity and participation; (4) education; and (5) social and emotional impact. The survey was launched online via Qualtrics in February 2018 and remained open for a 12-month period, promoted through social media platforms. The study was approved by the Human Research Ethics Committee at the University of Western Australia (RA/4/20/1045) and all participants gave informed consent.
This paper focuses on responses related to diagnosis and therapy domains. Questions within the diagnosis domain included the age of their child when they first became concerned or aware of their child’s movement difficulties, the setting in which these difficulties were observed (i.e. home, child health services, early learning and childcare centres, kindergarten, school), the age at which they first sought help, and the age at which their child first received a diagnosis for their movement difficulties. The diagnostic labels that their child had been given in relation to their movement difficulties were collected, along with the medical and/or allied health professional(s) who provided the diagnosis. Given that movement difficulties co-occur with other neurodevelopmental disorders and learning difficulties, we collected data on co-occurring conditions. Families were also asked if receiving a diagnosis for their movement difficulties had been helpful. Questions within the therapy domain included information on therapy attendance, both past and present, types of therapies currently accessed and duration and regularity of attendance. Parents reported on whether they felt supported to maintain therapy at home, and if they felt the therapy their child received was sufficient to support their movement difficulties. Out-of-pocket costs of therapy and access to funding were also evaluated.
Analysis
Data were entered into SPSS Statistics version 25 and descriptive statistics were generated. For questions with response rates of at least 80%, percentages are reported. For items where multiple responses were possible, percentages can exceed 100% (i.e. diagnosis received, therapy attendance). One-way analyses of variance were used to examine if sex or position in family (i.e. only child, eldest, middle or youngest child) was associated with differences in the age of child at first concern, the age of child when parents first sought help and the age of child at diagnosis. One-way analyses of variance were also used to examine if the diagnostic label received for a child’s movement difficulties (e.g. DCD, dyspraxia) or presence of a co-occurring condition altered the age of their motor diagnosis. Significance level was set at p < 0.05.
Results
Sample characteristics
Data were available for 403 families, with responses relating to 435 children (374 reporting on one child in their family, 26 reporting on two children in their family, 3 reporting on three children in their family). Most responses related to a male child (73.7%), with a relatively even distribution in responses across age groups (Table 1). Almost one-half of participants completed the survey with respect to their eldest child (45%). Index of Socio-Economic Advantage and Disadvantage quintiles were obtained based on geographic location, with 9.0% of families falling in quintile 1 (most disadvantaged areas), 13.3% quintile 2, 15.1% quintile 3, 29.1% quintile 4 and 33.5% in quintile 5 (most advantaged areas). In addition, family income was examined, with 13.2% classified as low income (<$48,000 per annum), 51.0% as middle income ($48,500–145,000 per annum) and 35.8% classed as high income (>$145,000 per annum).
Nearly one-third (30.0%) of parents reported a history of movement difficulties in their family, and 36.8% reported a family history of other neurodevelopmental, language or learning disorders. More specifically, 17.6% of families reported that they had a family history of ADHD, 17.6% ASD and 14.4% dyslexia.
Identification and diagnosis
On average, children were aged 2.5 ± 2.0 years when parents first became concerned about their movement and, in most cases, this concern related to parents observing their child in the home environment (63.2%). The average age parents first sought help was 3.4 ± 2.0 years, with 55.6% of families seeking help less than a year after first experiencing concern. For the 87.3% of children who had received a diagnosis for their movement difficulties (n = 385), the average age of diagnosis for their movement difficulties was 5.3 ± 2.6 years. The time between seeking help and diagnosis was comparatively large, with 2–4 years not uncommon (mean 2.8 ± 2.3 years). Almost half (45.7%) of respondents who received a diagnosis waited over 2 years for a diagnosis after first seeking help, 29.3% waited between 1 and 2 years and 25.9% were diagnosed less than a year after seeking help. There were no significant differences between sex of the child or position in the family and the age of the child at first concern, the age of the child when parents first sought help and the age of the child at diagnosis (all p > 0.05).
Thirty-eight percent of parents reported receiving one diagnostic label for their child’s movement difficulties, 31% two diagnostic labels, 16% three diagnostic labels and 15% four or more diagnostic labels. The most common diagnosis was dyspraxia (64.7%), followed by DCD (48.8%), motor dyspraxia (28.4%) and sensory integration disorder (17.6%). Nine separate diagnostic terms were reported (Fig. 1). Most parents (86.8%) reported that receiving a diagnosis was helpful.
To evaluate if the diagnostic label had an impact on the age of diagnosis, children who received a singular diagnosis of DCD (n = 72) or dyspraxia (n = 115) were compared. Children diagnosed with DCD were diagnosed at a significantly later age (mean = 6.60 ± 3.0 years) than those diagnosed with dyspraxia (mean = 5.05 ± 2.1 years) (F(1,185) 16.89, p < 0.001).
Diagnosing profession
Most children received their first diagnosis from either an occupational therapist (38.2%) or paediatrician (30.8%). Professionals providing diagnoses are outlined in Fig. 2. Of the children who received a diagnosis of DCD, 39.5% received this diagnosis from an occupational therapist and 39.5% from a paediatrician. Slightly more children with dyspraxia were diagnosed by an occupational therapist (42.9%) and fewer by a paediatrician (31.2%).
Co-occurring conditions
Comorbidity was commonly reported for children in the study, with 70.0% (n = 309) diagnosed with at least one co-occurring neurodevelopmental, language or learning disorder. Twenty-eight percent of children had one co-occurring diagnosis, 18.1% two, 12.1% three, and 11.1% four or more. The most common co-occurring diagnosis (Fig. 3) were childhood apraxia of speech (CAS) diagnosed in 39.7% of children, followed by ADHD (21.6%), ASD (18.0%), dysgraphia (16.2%), dyslexia (9.0%) and dyscalculia (1.8%).
To determine if co-occurring conditions might be associated with an earlier or later movement-related diagnosis, age of diagnosis was examined. The average age of diagnosis for a movement-related co-occurring with CAS was 4.41 ± 1.96 years, ASD 5.06 ± 2.17 years and ADHD 5.24 ± 2.24 years. Children without a co-occurring condition had their movement difficulties diagnosed slightly later, 5.93 ± 2.81 years (F(1,329) 3.05, p = .082).
Therapy
Almost all families (93.9%) had accessed therapy to assist their child’s movement difficulties, with 63.9% of children currently receiving therapy. Most children currently receiving therapy were younger in age, with attendance declining with increasing age. A total of 76.7% of children aged 4–6 years were currently receiving therapy, 72.6% of children aged 7–9 years, 60.7% of children aged 10–12 years and 26.8% of children aged 13 years and over. Of those currently receiving therapy, 70.4% were seeing an occupational therapist, 49.2% a speech therapist, 29.0% a physiotherapist, 29.0% a psychologist and 21.8% an exercise specialist. The regularity of attendance was also recorded (i.e. weekly, fortnightly, monthly, yearly), with most children attending occupational therapy (72.0%), speech therapy (76.1%) and exercise specialists (94.9%) on a weekly basis, with physiotherapy (45.0%) and psychology (55.7%) more likely to be accessed fortnightly.
While 68.5% of parents felt supported to maintain the progress that their child made in therapy at home, 67.6% reported that they felt the therapy received was not sufficient to support their child’s movement difficulties. The cost was the major limiting factor for families who had not accessed therapy for their child and less than half of the families (42.2%) reported receiving funding to support therapy costs.
Discussion
The current study provides the first large-scale investigation of parents’ experiences of their child’s diagnosis and treatment of DCD. Findings revealed parents are generally concerned about their child’s movement during early childhood and seek help early. While most children in the study had received a diagnosis, almost half waited >2 years after initially seeking help and 13% had not received a diagnosis yet. The study revealed there is no clear diagnostic process, with nine separate diagnostic terms used, more children diagnosed with dyspraxia than with the currently accepted clinical diagnosis of DCD, and a range of health professionals making these inconsistent diagnoses. Comorbidity was common, with 70% of children diagnosed with at least one comorbid condition, and those with a comorbid condition slightly more likely to have their movement difficulties formally recognised at a younger age than those with a movement difficulty alone. While most families accessed therapy to support their child’s movement difficulties, therapy type and frequency varied. Finally, many families reported that the therapy received was not sufficient to support their child’s movement difficulties. Overall, the findings of this study demonstrate that families experience considerable challenges when seeking assistance for their child’s movement difficulties, with significant implications for clinical practice and public health policy.
In 2012, the European Academy of Childhood Disability published international guidelines for the definition, diagnosis and intervention of DCD,28 with a revised version released in 2019.6 In these guidelines, DCD was recommended as the preferred diagnostic term, a term first appearing in the Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised (DSM-III-R)3 and still appearing in the current versions of the DSM1 and International Classification of Diseases.4 A diagnosis is not generally recommended until 5 years age (unless family history) and that diagnosis should be made by a medical professional or a multidisciplinary team that includes a medical professional to ensure the movement difficulties are not related to another medical condition (e.g. genetic, vision, neuromuscular). Unfortunately, based on the current data, the international guidelines are not being implemented. Children were more likely to have their movement difficulties labelled as dyspraxia and to receive this label from an occupational therapist.
Although the average age of diagnosis in our study cohort was close to the minimum age recommended by international guidelines,6 age of diagnosis was largely dependent on the diagnostic label children received. Children diagnosed with (motor) dyspraxia on average received this diagnosis close to 5 years, while those receiving the correct clinical diagnosis of DCD were diagnosed closer to 6.5 years. It is possible that the label dyspraxia, which is not bound by diagnostic criteria or a distinct evaluation process,18 is being provided to families early in life as a way of describing a child’s movement challenges without realising that this label is likely interpreted as a formal diagnosis. Given that previous research has also demonstrated that medical and allied health professionals have increased familiarity with the term dyspraxia,16 it is likely that this is also a factor contributing the early and increased diagnosis of dyspraxia within Australia.
The high prevalence of comorbidity within the sample is not unexpected. While the prevalence of DCD with ASD and/or ADHD was slightly lower than that reported in previous studies,13,29,30 this likely reflects the survey’s recruitment strategy with the study only advertised across media platforms specific to DCD. The condition with the highest rate of co-occurrence with DCD reported in the present study was CAS. Like DCD, CAS is a motor disorder. While the two disorders are viewed as two separate conditions, they likely share similar aetiological mechanisms.31 One disorder involves the disruption of actions involved in the production of speech (i.e. strength of expiration, movements of the muscles in the jaw, tongue and lips), while the other involves disruption of actions coordinating movements in the rest of the body.
Interestingly, children with co-occurring conditions had their movement difficulties diagnosed, on average, 12 months earlier than children with movement difficulties alone. This may reflect exposure to multidisciplinary clinicians (e.g. speech therapists, occupational therapists, psychologists) for treatment of some neurodevelopmental conditions (e.g. ASD), increasing the likelihood of movement difficulties being identified. Children presenting with movement difficulties alone (i.e. in one developmental domain) may be less likely to have had these difficulties formally identified. In addition, given there is the possibility of some children presenting with early motor delays shifting into a typically developing trajectory,32 medical professionals are possibly more likely to employ a ‘watch and wait’ approach. Unfortunately, this means those children who are likely to go on a receive an isolated diagnosis of DCD do not receive a diagnosis limiting opportunity for early intervention.
While most families had accessed therapy for their child, less than half had access to funding to support therapy. Occupational therapy was the most regularly accessed, with almost three-quarters of families with children aged 4–6 and 7–9 years attending weekly. Attendance to occupational therapy declined with age beyond this point and this possibly reflects a change in priorities with age. The most commonly accessed therapy in children aged 10–12 years and 13+ years were psychology-related services, potentially reflective of increased social and emotional health difficulties experienced with age.33 With two out of three families reporting that the therapy received to support their movement difficulties was inadequate, further research is needed to understand what therapy services are being delivered and if they are meeting the needs of families (e.g. evidence-based, available, affordable).
The findings of this study provide important insights into the challenges families experience in relation to obtaining a diagnosis and therapy for their child’s DCD. There is a clear need for targeted awareness campaigns and professional development opportunities for medical and allied health professionals to adopt the correct clinical diagnostic term and ensure a clear role for clinical experts involved in the diagnostic process. While guidelines previously developed are a valuable resource, more extensive implementation of these guidelines into clinical practice is needed to ensure children with DCD do not fall through the gaps of the healthcare system. In addition, as some therapies do not achieve meaningful outcomes for families (see refs. 28,34) and many families struggle with the financial burden of therapy, delivery of interventions that are family-centred, evidence-based, and affordable are urgently needed for children with DCD.
Limitations of the study include self-selection bias possibly limiting the generalisability of survey results and over/under-representation in some regions within Australia. In addition, while data were obtained on the type of services accessed (e.g. OT, physiotherapy) and regularity of attendance, data on the type of intervention children were receiving was not obtained. This certainly would be an interesting area to investigate through a survey of clinicians. There is also scope for future research to further the understanding the experiences and current needs of adults with DCD, including a pathway after the intervention. Although the findings of this study are based on the experiences of Australian families, the survey is currently being implemented internationally to increase the representativeness and generalisability of results and to be able to make comparisons in practices and experiences across countries.
References
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM 5 (American Psychiatric Association, 2013).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV (American Psychiatric Association, 1994).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-III-R (American Psychiatric Association, 1987).
World Health Organization. The ICD-11 International Statistical Classification of Diseases and Related Health Problems (World Health Organization, 2020).
World Health Organization. The ICD-10 Classification of Mental and Behavioral Disorders: Clinical Descriptions and Diagnostic Guidelines (World Health Organization, 1992).
Blank, R. et al. International clinical practice recommendations on the definition, diagnosis, assessment, intervention, and psychosocial aspects of developmental coordination disorder. Dev. Med. Child Neurol. 61, 242–285 (2019).
Schell, S., Roth, K. & Duchow, H. Developmental coordination disorder in Alberta: a journey into knowledge translation. Phys. Occup. Ther. Pediatr. 40, 294–310 (2020).
Gibbs, J., Appleton, J. & Appleton, R. Dyspraxia or developmental coordination disorder? Unravelling the enigma. Arch. Dis. Child. 92, 534–539 (2007).
Caçola, P. Physical and mental health of children with developmental coordination disorder. Front. Public Health 4, 224 (2016).
Karras, H. C., Morin, D. N., Gill, K., Izadi-Najafabadi, S. & Zwicker, J. G. Health-related quality of life of children with developmental coordination disorder. Res. Dev. Disabil. 84, 85–95 (2019).
Zwicker, J. G., Harris, S. R. & Klassen, A. F. Quality of life domains affected in children with developmental coordination disorder: a systematic review. Child Care Health Dev. 39, 562–580 (2013).
Zwicker, J. G., Suto, M., Harris, S. R., Vlasakova, N. & Missiuna, C. Developmental coordination disorder is more than a motor problem: children describe the impact of daily struggles on their quality of life. Br. J. Occup. Ther. 81, 65–73 (2018).
Licari, M. K. et al. Prevalence of motor difficulties in autism spectrum disorder: analysis of a population‐based cohort. Autism Res. 13, 298–306 (2020).
Kadesjö, B. & Gillberg, C. Attention deficits and clumsiness in Swedish 7‐year‐old children. Dev. Med. Child Neurol. 40, 796–804 (1998).
Rodger, S. & Mandich, A. Getting the run around: accessing services for children with developmental co-ordination disorder. Child Care Health Dev. 31, 449–457 (2005).
Wilson, B. N., Neil, K., Kamps, P. H. & Babcock, S. Awareness and knowledge of developmental co-ordination disorder among physicians, teachers and parents. Child Care Health Dev. 39, 296–300 (2013).
Hunt, J., Zwicker, J., Godecke, E. & Raynor, A. Awareness and knowledge of developmental coordination disorder: a survey of caregivers, teachers, allied health professionals and medical professionals in Australia. Child. Care Health Dev. (2020).
Henderson, S. E. & Henderson, L. Toward an understanding of developmental coordination disorder: terminological and diagnostic issues. Neural Plast. 10, 1–13 (2003).
Anderson-Mooney, A. J., Schmitt, F. A., Head, E., Lott, I. T. & Heilman, K. M. Gait dyspraxia as a clinical marker of cognitive decline in Down syndrome: a review of theory and proposed mechanisms. Brain Cogn. 104, 48–57 (2016).
Onder, H. Dyspraxic gait due to right posterior cerebral artery stroke. J. Neurosci. Rural Pract. 9, 162 (2018).
Kumar, A. & Tsao, J. W. Alzheimer disease. https://europepmc.org/article/NBK/NBK499922 (2019).
Yu, Y. T. et al. A psychometric study of the Bayley Scales of Infant and Toddler Development—3rd Edition for term and preterm Taiwanese infants. Res. Dev. Disabil. 34, 3875–3883 (2013).
Esmail, S. The diagnosis and management of Parkinson’s disease. Sch. J. Appl Sci. Res. 1, 13–19 (2018).
Karkling, M., Paul, A. & Zwicker, J. G. Occupational therapists’ awareness of guidelines for assessment and diagnosis of developmental coordination disorder: Mesure selon laquelle les ergothérapeutes connaissent les lignes directrices relatives à l’évaluation et au diagnostic du trouble du déve. Can. J. Occup. Ther. 84, 148–157 (2017).
Missiuna, C., Moll, S., Law, M., King, S. & King, G. Mysteries and mazes: parents’ experiences of children with developmental coordination disorder. Can. J. Occup. Ther. 73, 7–17 (2006).
Jijon, A. M. & Leonard, H. C. Parenting stress in parents of children with developmental coordination disorder. Res. Dev. Disabil. 104, 103695 (2020).
Licari, M. K. & Williams, J., Impact for DCD Team. National survey evaluating the impact of developmental coordination disorder in Australia: summary of results. https://www.telethonkids.org.au/globalassets/media/documents/projects/impact-for-dcd-report.pdf (2020).
Blank, R., Smith-Engelsman, B., Polatajko, H. & Wilson, P. European academy for childhood disability (EACD): recommendations on the definition, diagnosis and intervention of developmental coordination disorder (long version). Dev. Med. Child Neurol. 54, 54–93 (2012).
Green, D. et al. Impairment in movement skills of children with autistic spectrum disorders. Dev. Med. Child Neurol. 51, 311–316 (2009).
Pitcher, T. M., Piek, J. P. & Hay, D. A. Fine and gross motor ability in males with ADHD. Dev. Med. Child Neurol. 45, 525–535 (2003).
Ho, A. K. & Wilmut, K. Speech and oro-motor function in children with developmental coordination disorder: a pilot study. Hum. Mov. Sci. 29, 605–614 (2010).
Jenni, O. G., Chaouch, A., Caflisch, J. & Rousson, V. Infant motor milestones: poor predictive value for outcome of healthy children. Acta Paediatr. 102, e181–e184 (2013).
Missiuna, C., Moll, S., King, G., Stewart, D. & Macdonald, K. Life experiences of young adults who have coordination difficulties. Can. J. Occup. Ther. 75, 157–166 (2008).
Novak, I. & Honan, I. Effectiveness of paediatric occupational therapy for children with disabilities: a systematic review. Aust. Occup. Ther. J. 66, 258–273 (2019).
Acknowledgements
We are grateful to the families who participated in this study. We acknowledge the contribution made to this project by DCD Australia Incorporated, the national peak body supporting people with DCD and their families in Australia. We would also like to thank the individuals and health services across Australia that helped to develop and promote the survey.
Author information
Authors and Affiliations
Contributions
M.K.L. and J.W. conceptualised and designed the study, with feedback on the design received from C.B., C.E., S.L.R. and A.J.S. Data acquisition and analysis were overseen by M.K.L. and J.W. All authors contributed to the interpretation of results. Drafting of the article was performed with by M.K.L., with all authors revising it critically for important intellectual content. All authors approved the final version of this article for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Statement of consent
All participants gave informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Licari, M.K., Alvares, G.A., Bernie, C. et al. The unmet clinical needs of children with developmental coordination disorder. Pediatr Res 90, 826–831 (2021). https://doi.org/10.1038/s41390-021-01373-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01373-1