Abstract
Background
Screening studies have shown that 0.7–4.5% of generally healthy children have isolated diastolic high BP. We therefore studied the characteristics of children with diastolic BP in the elevated and hypertensive ranges according to current guidelines in US children from the National Health and Nutrition Examination Survey (NHANES, 1999–2016).
Methods
We studied 17,362 children (8–18 years) with BP measured by sphygmomanometry. High BP was categorized as isolated systolic (iSH), isolated diastolic (iDH), or Mixed.
Results
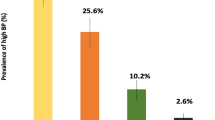
Overall, 86.0% (95% CI = 85.0–87.0) of the population had normal BP, 8.7% (8.0–9.3) elevated BP, 4.9% (4.4–5.5) Stage 1, and 0.4% (0.4–0.6) Stage 2. Moreover, 11.1% (10.3–12.0) had iSH, 1.9% (1.5–2.2) iDH, and 1.0% (0.8–1.2) Mixed. Children with iDH were more likely to be female, younger, white, and leaner than those with iSH, with lower rates of overweight/obesity. iDH was generally between normals and iSH. Resting heart rate was significantly higher in iDH even after adjustment for known covariates.
Conclusions
Children with iDH may have a distinct clinical picture. A leaner habitus and higher resting heart rate may reflect differences in underlying pathophysiology. Longitudinal follow-up studies are needed to better define the pathogenesis, progression, and long-term prognosis in iDH.
Impact
-
Using gold-standard auscultation and 2017 guidelines, isolated diastolic high BP (iDH) is found in 1.9% (95% CI 1.5–2.2) of American children; these children are younger, leaner, more female, and have fewer cardiometabolic risks.
-
Resting heart rate is significantly higher in iDH compared to both normals and iSH even after adjustments for known covariates. Autonomic hyperactivity in iDH may speak to both etiology and therapeutic approaches.
-
iDH appears to be a distinct clinical phenotype characterized by differences in anthropometric measures, sex, age, and resting heart rate. Follow-up studies are clearly needed to clarify its pathogenesis, progression, and prognosis.
Similar content being viewed by others
Introduction
High blood pressure (BP)—where single-visit BP levels are consistent with elevated BP, stage 1, or stage 2 hypertension—is poorly understood in children. Nevertheless, AAP guidelines highlight the importance of single-visit BPs in the elevated or hypertensive range, which generally require earlier follow-up (with auscultation) and consideration of referral for nutrition and weight management if appropriate.1,2
In a longitudinal 2002 survey of 2460 American children aged 12–16 years, Sorof et al. documented isolated diastolic high BP (iDH) at initial screen in 0.7% of the population. These children had diastolic BP (DBP) > 90th percentile based on 1996 standards, combining categories “high normal” and “hypertension”. In contrast, isolated systolic high BP (iSH, systolic BP (SBP) > 90th percentile) was found in 15% of the population at initial screen; these children were more likely to be obese (33% vs. 11%, p < 0.001). In sustained isolated systolic hypertension, increased resting heart rates and SBP variability reflected sympathetic nervous system hyperactivity.3
More recent studies have assessed the prevalence of these three high-BP phenotypes using standardized single-visit BP measurements with BP in the elevated/hypertensive range.4,5,6 iSH was the most common, with iDH in 4.5% of Greek children aged 9–13 years and 3.2% of Chinese children between 6 and 18 years.4,5 Moreover, these studies consistently showed that children with iDH are less likely to be overweight or obese (OW/OB) than children with iSH, with lower z-scores (z) for body mass index (BMIz) and waist circumference (WC).7 To our knowledge, there have been no comparable studies in American children based on gold-standard auscultation or the new 2017 American Academy of Pediatrics (AAP) guidelines.2 Although the long-term consequences of iDH in children are not well known, DBP is generally superior to SBP as a predictor of cardiovascular morbidity in adults <50 years.8
The current study seeks to fill lacunae in our understanding of pediatric iDH in an American context using current diagnostic criteria. Our primary objective is to define the population prevalence of the three different high-BP phenotypes in 17,362 US children aged 8–18 years in the National Health and Nutrition Examination Survey (NHANES, 1999–2016). Secondarily we will explore their clinical characteristics and cardiometabolic risk factors.
Patients and methods
Data were derived from nine biennial NHANES cycles (A–I) collected between 1 January 1999 and 31 December 2016 by the Centers for Disease Control and Prevention (CDC).9,10 Of 19,093 children aged 8.0–18.0 years, 17,362 could be assigned a BP stage based on the 2017 AAP guidelines.2 Additional details as to NHANES data collection will be found in references. 9,10,11 Socioeconomic status is reported as the Index for the Ratio of Family Income to Poverty (INDFMPIR) as defined by the Department of Health and Human Services.9,10 Race/ethnicity categories were defined by self-identification as follows: European American (White), African American (Black), Hispanic (“Mexican-American” or “Other Hispanic”), and Other.9,10
Age- and sex-specific z-scores were calculated for height (Htz, height measured by calibrated stadiometer to the nearest 0.1 cm), weight (Wtz, weight measured on a digital scale to the nearest 0.1 kg), and body mass index (BMIz, BMI in kg/m2) using tables from both the CDC and the World Health Organization (WHO).12,13 Z-scores for waist circumference (WCz) and waist:height ratio (WtHz) were based on NHANES III reference data.14 Z-scores for triceps and subscapular skinfold thicknesses, mid-upper arm circumference, and upper arm fat and muscle areas were based on charts from the same reference population used to create the CDC 2000 growth charts.15,16
BP was measured by auscultation after resting quietly in a seated position for 5 min in the NHANES mobile examination center. After determination of maximum inflation pressures, three and sometimes four consecutive BP readings were recorded, with DBP marked by the fifth Korotkoff sound. SBP and DBP means were calculated after dropping the first measurement. Age-, sex-, and height-specific percentiles were calculated for SBP and DPB using the 2017 AAP references.2 High BP was defined as a mean single-visit BP value consistent with elevated, stage 1, or stage 2 levels by AAP guidelines.2 iSH was present if SBP was elevated, stage 1, or stage 2. For participants <13 years, iDH was similarly defined. For those ≥13 years, there is no category for elevated DBP, and iDH was diagnosed when DBP was stage 1 or 2. Subjects meeting both criteria were designated Mixed. Heart rate (HR) was recorded in beats per minute (bpm) from two 30 s measurements.
Blood was analyzed for total cholesterol (TCHOL) and high-density lipoprotein (HDL) cholesterol. Fasting low-density lipoprotein (LDL) (Friedewald) cholesterol and triglycerides (TRIG) were measured in participants aged 12–18 years, as was hemoglobin A1c (A1C). For each measure, abnormal cut points were defined by the NIH/NHLBI Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents and the American Diabetes Association.17,18 Defining criteria were TCHOL ≥ 5.2 mmol/L, LDL ≥ 3.4 mmol/L, HDL < 1.0 mmol/L, and TRIG ≥ 1.1 mmol/L for age ≤9 years or ≥1.5 mmol/L for >9 years. For all ages, the ADA defines A1C > 5.6% (>38 mmol/mol) as abnormal, with 5.6–6.4% (39–47 mmol/mol) as prediabetes and >6.5% (>48 mmol/mol) as overt diabetes mellitus. The estimated glomerular filtration rate (eGFR) was calculated by the Bedside Schwartz equation and the Full Age Spectrum (FAS) equation of Pottel et al.19,20 Values less than 90 mL/min/1.73 m2 are diagnosed as chronic kidney disease.19
Statistical analyses
All analyses were performed in R version 3.6.2 with a two-sided p < 0.05 considered statistically significant.21 To properly account for multistage sampling, NHANES provides identifiers for primary sampling units and strata. To account for non-response and under-coverage and permit valid population inferences, they also furnish inverse-probability sample weights for the mobile examination centers. These were combined as recommended for NHANES subsets using the R survey package.22
Categorical variables are reported as percentages and 95% confidence intervals (CI). Continuous variables are reported as medians and interquartile ranges or means and 95% CI as appropriate. Population means were compared across groups using generalized linear models for survey data, and proportions (counts) were compared with survey-weighted chi-square tests or logistic regression.
Ethics
Ethics approval was obtained from the Health Research Ethics Board at the University of Manitoba’s Faculty of Medicine for the use of anonymized data from an existing database.
Results
Demographic and clinical characteristics from 17,362 subjects are presented in Table 1. In general, the sample reflected the population except for ethnic composition, where NHANES deliberately over-samples minorities.10 Using weighted population estimates, the mean age was 13.2 years with a near-equal distribution of sexes. Population proportions with different BP phenotypes are given in Table 1. Of the 14.0% with high BP (13.0–15.0), 79.5% (95% CI: 76.9–82.0) had iSH, 13.3% (95% CI: 11.2–15.4) had iDH, and 7.2% (95% CI: 5.8–8.6) were Mixed (not shown). The study population was slightly taller and heavier than the CDC and WHO reference populations. By CDC criteria, slightly more than a third were OW/OB. Other measures of adiposity (e.g. WCz and skinfold thicknesses) generally followed BMIz. Both arm fat area and arm muscle area exceeded that of the reference population.
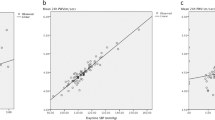
In Fig. 1, mean SBP percentile in iDH was between normals and iSH. In contrast, the mean DBP percentile was significantly higher in iDH than iSH, with the latter indistinguishable from normotensives; the Mixed group shared features with both iSH and iDH. Table 2 summarizes additional characteristics by BP phenotypes. Although males were significantly more likely to be affected in all high BP phenotypes compared to normals, iDH and Mixed had significantly fewer males than iSH. There was a small but significant difference in age between iSH and iDH. Racial composition in iDH did not differ from normotensives, while iSH were less likely to be white. Both iDH and Mixed had significantly higher heart rates compared to normals and iSH. The iDH and Mixed phenotypes were also associated with more advanced BP stages, particularly stage 1. Body habitus was comparable in iSH and Mixed and differed significantly from normotensives. Those with iDH were generally between iSH and normal and differed significantly from both. Other anthropometric parameters followed a similar pattern, as did rates of OW/OB. Compared to normals, arm fat and muscle area z-scores were significantly increased in iSH and Mixed and intermediate in iDH.
Table 3 presents laboratory characteristics by BP phenotype. Children with iDH resembled normotensives in terms of known cardiometabolic risk factors except for an increased incidence of elevated TCHOL. Those with iSH experienced a significantly higher incidence of abnormal A1C, HDL, LDL, TCHOL, and TRIG. They were also associated with an increased mean concentration of LDL and comparable HDL (not shown), and the LDL/HDL ratio was significantly increased in both iSH and iDH. Regarding other analytes, some differences are unlikely to be clinically meaningful, e.g., higher total calcium and lower phosphorus in the second decimal place. While within normal limits, a significant reduction in mean eGFR was noted in all high BP groups compared to normals and was comparable in iSH and iDH. The same was true for FAS eGFRs, and serum urate was significantly increased in all high BP phenotypes compared to normals.
Since heart rate in healthy children normally declines with age and increases with obesity, regression adjustment is summarized in Table 4A.3,23 Compared to normals, iDH was associated with a significant increase in heart rate by almost 5 bpm, which persisted even after adjustment for age, sex, BMIz, and race. Resting heart rate was also increased in iSH compared to normals, but children with iDH were significantly higher still. To explore potential interactions between age and BP phenotype, patients were divided by Age ≥ 13 years. The expected decline in heart rate in older children again persisted after covariate adjustment, but significant interaction terms attest to further declines in adolescents with iSH, which did not happen with iDH (Table 4B). In contrast, elevated serum uric acid in children with high BP resolved after regression adjustment for known covariates age, sex, race, and BMIz (Supplementary Table 1).24
Discussion
When the new AAP 2017 guidelines and gold-standard auscultation were applied to US children,1,2 iDH was found in 1.9% of the population. Earlier reports range from 0.7% on initial screening in the United States, 4.5% in Greece, and 3.2% in China.3,4,5
Of note, the study of American children by Sorof et al. used the 1996 blood pressure guidelines; moreover, they used oscillometry, which may underestimate DBP, particularly in children (mean bias 3.1 mmHg, 95% limits of agreement −22.4 to 28.6).3,25 The two other studies in non-American children relied on auscultation, still the gold-standard for the AAP guidelines.1,2 However, they were based on older 2004 guidelines.4,5 As previously reported, 86% of the pediatric population had normal BP:11 iSH is still the most common phenotype in 11.9% of the population, followed by iDH (1.9%) and Mixed (1.0%).
Primary pediatric hypertension is consistently associated with increased BMI and OW/OB status, and its prevalence is increasing.26 It is postulated that increased visceral fat augments adipokines and leads to sympathetic hyperactivity with increased heart rate and BP (reviewed by Flynn27).
We noted significantly higher measures of central and peripheral adiposity in those with iSH and Mixed high BP compared to normotensives. Interestingly, most of these measures for iDH were lower than for iSH and Mixed, but still significantly higher than normals. Others have reported a “leaner” phenotype in iDH, suggesting differences in pathogenesis or susceptibility,5,7,28 although the precise mechanism remains unclear. In keeping with differences in body habitus, children with iDH were significantly less likely than those with iSH to have other metabolic risk factors, such as prediabetes and hyperlipidemia. Since previous studies of BP phenotypes did not include laboratory results, we do not know whether this pattern is typical.3,5,6,7 Nevertheless, iSH appears to drive much of the risk profile usually attributed to high BP in children.26 Although we noted that those with iDH were more likely to be female and somewhat younger than the iSH group, there is considerable variation in age and sex distributions across studies.
The observed increase in resting heart rate in all BP phenotypes is consistent with the obesity-adipokine hypothesis.27 Nevertheless, the iDH and Mixed groups were also found to have significantly increased HR compared to both normals and iSH despite significantly lower body fat measures and rates of OW/OB. These differences persist even after adjustment for potential confounders. Further studies are needed to characterize autonomic hyperactivity in these phenotypes, which may have treatment implications, e.g., adrenergic blockade.
Although the diagnosis of hypertension typically requires confirmation over multiple visits, the AAP highlights the clinical importance of single-visit measurements in the elevated or hypertensive range, which require earlier follow-up with auscultatory measurements and possible referral for nutrition or weight management (for details, see Section 4.3b in ref. 2). Moreover, in a recent US study based on oscillometry and the 2017 guidelines, Bell et al. put the incidence of high BP at 29.3% at the first visit, with persistent high BP in 18.6% across three visits. This speaks to the persistence of high BP, at least in the short term. Importantly, the proportion with sustained Stage 1 or 2 hypertension was only 2.3%.29
The evolution of iDH in children and young adults has been less well characterized. DBP clearly tracks in childhood, particularly in leaner children.28,30 Tracking of DBP from childhood into adulthood has also been reported, with typical correlations of 0.2–0.4 depending on race, sex, and age.31The latter may be particularly worrisome given clustering and tracking of BP with other risk factors, such as obesity.32
In terms of prognosis, a study of 1.2 million male Swedish army recruits (mean age 18.4 years, followed for a median of 24 years) demonstrated a monotonic relationship between cardiovascular mortality and DBP that was stronger than for SBP, with a steep increase for DBP > 90 mmHg.33 The latter is relevant to current definitions of iDH, which for children ≥13 years are based on absolute thresholds (normal if DBP < 80 mmHg, stage 1 for 80–90 mmHg, and stage 2 if ≥90 mmHg).2 In fact, our observed association between iDH/Mixed phenotypes and more advanced BP stages in Table 2 may simply be an artifact of this definition, since there is no “elevated” DBP category for adolescents. In the Framingham Study of adults (reviewed by Berney et al.8), iDH peaked between 50 and 60 years with a population prevalence of 4–6%, higher in males. Moreover, BP changes preceded changes in vascular compliance by years,34 suggesting that iDH may be a precursor for subsequent systolic or mixed hypertension. Based on prospective intervention trials,35 the American Heart Association and American College of Cardiology have subsequently adopted target DBP < 80 mmHg to reduce cardiovascular mortality. In a meta-analysis of 61 trials involving almost one million patients, each 10 mmHg increase in DBP was associated with a doubling in the risk of death from cardiovascular disease.36 Clearly, the prognosis of elevated DBP in childhood merits further attention.
Although we observed a significant decrease in eGFR (mL/min/1.73 m2, adjusted for body-surface area) in all high BP phenotypes compared to normals, all means were within normal limits, and a cross-sectional survey cannot determine causality. Moreover, eGFR was only available in a subset of older children ≥12 years. Its potential seriousness is underscored by a study of 2.2 million Israeli army recruits followed for a median of 16.8 years, in which pre- or overt hypertension in adolescence was associated with an increased incidence of end-stage renal disease with hazard ratios of 1.32 (1.11–1.58) and 1.44 (1.17–1.79), respectively.37
The strengths of this study include a large sample with 3–4 BP readings measured by trained staff using gold-standard sphygmomanometry. Auscultation may be particularly important here, since oscillometric DBP is often biased and imprecise,25 particularly in children. Participants in NHANES are generally unselected and at low risk for secondary hypertension. Detailed anthropometric and laboratory measures allowed for comprehensive assessment of cardiovascular risk, and survey weights were provided for generalizing to the US population. Limitations include no repeated visits; insufficient numbers for a detailed assessment of race-, sex-, and age-specific differences; lack of information pertaining to personal or family history and comorbidities; and collection of laboratory data in only a subset of older children ≥12 years. Although our unselected sample is generally healthy, it is also possible that some would be found to have secondary hypertension on further evaluation.
Conclusion
Using gold-standard auscultation and the 2017 AAP diagnostic guidelines, iDH is found in 1.9% (1.5–2.2) of North American children aged 8–18 years and accounts for 13.3% (11.2–15.4) of high BP. Although iDH in young adults may progress to systolic or mixed hypertension8 its relationship to iDH in childhood needs to be clarified. Moreover, these children appear to have a distinct clinical picture in terms of age, sex, ethnicity, and associated cardiometabolic risk factors. A leaner body habitus and higher resting heart rate may also reflect fundamental differences in underlying pathophysiology. With little information as to persistence of these phenotypes over time, further investigations and long-term follow-up of children with iDH are clearly needed to explore the pathogenesis, progression, and prognosis of what may be a distinct clinical disorder.
References
Rosner, B., Cook, N., Portman, R., Daniels, S. & Falkner, B. Determination of blood pressure percentiles in normal-weight children: some methodological issues. Am. J. Epidemiol. 167, 653–666 (2008).
Flynn, J. T. et al. Subcommittee on Screening and Management of High Blood Pressure in Children. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140, e20171904 (2017).
Sorof, J. M., Poffenbarger, T., Franco, K., Bernard, L. & Portman, R. J. Isolated systolic hypertension, obesity, and hyperkinetic hemodynamic states in children. J. Pediatr. 140, 660–666 (2002).
Karatzi, K. et al. Prevalence of hypertension and hypertension phenotypes by age and gender among schoolchildren in Greece: The Healthy Growth Study. Atherosclerosis 259, 128–133 (2017).
Yang, Y. et al. Prevalence of high blood pressure subtypes and its associations with BMI in Chinese children: a national cross-sectional survey. BMC Public Health 17, 598 (2017).
Pileggi, C., Carbone, V., Nobile, C. G. A. & Pavia, M. Blood pressure and related cardiovascular disease risk factors in 6-18 year-old students in Italy. J. Paediatr. Child Health 41, 347–352 (2005).
Manios, Y. et al. Prevalence of childhood hypertension and hypertension phenotypes by weight status and waist circumference: the Healthy Growth Study. Eur. J. Nutr. 57, 1147–1155 (2018).
Berney, M., Burnier, M. & Wuerzner, G. [Isolated diastolic hypertension: do we still have to care about it?]. Rev. Med Suisse 14, 1607–1610 (2018).
NHANES Questionnaires, Datasets, and Related Documentation. https://wwwn.cdc.gov/nchs/nhanes/Default.aspx (2020).
NHANES Examination Data. https://wwwn.cdc.gov/nchs/nhanes/search/datapage.aspx?Component=Examination&CycleBeginYear= (2020).
Sharma, A. K., Metzger, D. L. & Rodd, C. J. Prevalence and severity of high blood pressure among children based on the 2017 American Academy of Pediatrics Guidelines. JAMA Pediatr. 172, 557–565 (2018).
Kuczmarski, R. J. et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat. 11, 1–190 (2002).
de Onis, M. et al. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 85, 660–667 (2007).
Sharma, A. K., Metzger, D. L., Daymont, C., Hadjiyannakis, S. & Rodd, C. J. LMS tables for waist-circumference and waist-height ratio Z-scores in children aged 5-19 y in NHANES III: association with cardio-metabolic risks. Pediatr. Res. 78, 723–729 (2015).
Addo, O. Y., Himes, J. H. & Zemel, B. S. Reference ranges for midupper arm circumference, upper arm muscle area, and upper arm fat area in US children and adolescents aged 1-20 y. Am. J. Clin. Nutr. 105, 111–120 (2017).
Addo, O. Y. & Himes, J. H. Reference curves for triceps and subscapular skinfold thicknesses in US children and adolescents. Am. J. Clin. Nutr. 91, 635–642 (2010).
Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents, National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics 128, S213–S256 (2011).
American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care 43, S14–S31 (2020).
Schwartz, G. J. et al. New equations to estimate GFR in children with CKD. J. Am. Soc. Nephrol. 20, 629–637 (2009).
Pottel, H. et al. An estimated glomerular filtration rate equation for the full age spectrum. Nephrol. Dial. Transpl. 31, 798–806 (2016).
R: The R Project for Statistical Computing. https://www.r-project.org/ (2020).
Lumley, T. Complex Surveys: A Guide to Analysis Using R (Wiley and Sons, Hoboken, New Jersey, 2010).
Fleming, S. et al. Normal ranges of heart rate and respiratory rate in children from birth to 18 years of age: a systematic review of observational studies. Lancet 377, 1011–1018 (2011).
Kubota, M. Hyperuricemia in children and adolescents: present knowledge and future directions. J. Nutr. Metab. 2019, 3480718 (2019).
Miranda, J. J., Stanojevic, S., Bernabe-Ortiz, A., Gilman, R. H. & Smeeth, L. Performance of oscillometric blood pressure devices in children in resource-poor settings. Eur. J. Cardiovasc. Prev. Rehabil. 15, 362–364 (2008).
Rosner, B., Cook, N. R., Daniels, S. & Falkner, B. Childhood blood pressure trends and risk factors for high blood pressure: the NHANES experience 1988-2008. Hypertension 62, 247–254 (2013).
Flynn, J. T. Adiposity, the sympathetic nervous system, and childhood primary hypertension. Hypertension 62, 689–690 (2013).
Burke, G. L., Freedman, D. S., Webber, L. S. & Berenson, G. S. Persistence of high diastolic blood pressure in thin children. The Bogalusa Heart Study. Hypertension 8, 24–29 (1986).
Bell, C. S., Samuel, J. P. & Samuels, J. A. Prevalence of hypertension in children. Hypertension 73, 148–152 (2019).
Kollias, A., Pantsiotou, K., Karpettas, N., Roussias, L. & Stergiou, G. S. Tracking of blood pressure from childhood to adolescence in a Greek cohort. Eur. J. Public Health 22, 389–393 (2012).
Bao, W., Threefoot, S. A., Srinivasan, S. R. & Berenson, G. S. Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: the Bogalusa Heart Study. Am. J. Hypertens. 8, 657–665 (1995).
Nicklas, T. A., von Duvillard, S. P. & Berenson, G. S. Tracking of serum lipids and lipoproteins from childhood to dyslipidemia in adults: the Bogalusa Heart Study. Int. J. Sports Med. 23, S39–S43 (2002).
Sundström, J., Neovius, M., Tynelius, P. & Rasmussen, F. Association of blood pressure in late adolescence with subsequent mortality: cohort study of Swedish male conscripts. BMJ 342, d643 (2011).
Chen, X. & Wang, Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation 117, 3171–3180 (2008).
Whelton, P. K. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 71, e127–e248 (2018).
Lewington, S., Clarke, R., Qizilbash, N., Peto, R. & Collins, R. Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360, 1903–1913 (2002).
Leiba, A. et al. Prehypertension among 2.19 million adolescents and future risk for end-stage renal disease. J. Hypertens. 35, 1290–1296 (2017).
Author information
Authors and Affiliations
Contributions
All authors met the authorship requirements of Pediatric Research. A.S., C.R., and H.B.A. conceptualized and designed the study, carried out the initial analyses, drafted the initial manuscript, and reviewed and revised the manuscript. D.L.M. and T.B.-H. conceptualized and designed the study and reviewed and revised the manuscript. All authors approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Patient consent was obtained at the time of the NHANES survey.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Alsaeed, H., Metzger, D.L., Blydt-Hansen, T.D. et al. Isolated diastolic high blood pressure: a distinct clinical phenotype in US children. Pediatr Res 90, 903–909 (2021). https://doi.org/10.1038/s41390-021-01369-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01369-x
This article is cited by
-
Variation in paediatric 24-h ambulatory blood pressure monitoring interpretation by Canadian and UK physicians
Journal of Human Hypertension (2022)
-
Is Isolated Diastolic Hypertension an Important Phenotype?
Current Cardiology Reports (2021)