Abstract
Background
We investigated whether an association exists between regulatory T cells (Tregs) during initial presentation in children with idiopathic nephrotic syndrome (INS) and later development of frequently relapsing INS.
Methods
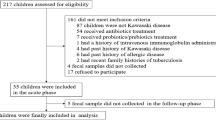
Blood samples were obtained at onset and at remission from 25 patients (median age, 4.0 years) with INS; eight did not show relapse after initial response (non-relapsing [NR]), whereas 17 showed frequent relapses (frequently relapsing [FR]). Tregs were measured by flow cytometry; increases were compared between groups. Fecal samples were obtained at onset from 20 patients with INS, as well as from 20 age-matched healthy children. Gut microbiota composition was assessed using 16S ribosomal RNA (rRNA) sequencing (ion PGM).
Results
The rate of increase in Tregs from onset to remission was significantly lower in the FR group (124.78%) than in the NR group (879.16%; P < 0.001). Additionally, 16S rRNA sequencing of gut microbiota showed that the proportion of butyric acid-producing bacteria was significantly lower in the FR group (7.08%) than in the healthy children (17.45%; P < 0.001).
Conclusions
In children with INS, small increases in Tregs in response to steroid treatment were associated with subsequent increased risk of frequent relapses. In addition, the FR group had a greater degree of dysbiosis at onset.
Impact
-
A low rate of Tregs increase is associated with subsequent frequent relapses of INS.
-
The increase in Tregs in response to steroid treatment was small when dysbiosis was present in patients with INS, particularly when the proportion of butyrate-producing bacteria was considerably reduced
-
We presume that improvement of dysbiosis by administration of probiotics and prebiotics may enhance the rate of Tregs’ increase, thus preventing frequent relapse.
Similar content being viewed by others
Introduction
Regulatory T cells (Tregs) are a class of T lymphocytes that function to suppress excessive immune responses, which would otherwise cause autoimmune diseases, inflammatory diseases, and allergic diseases.1 Research on Tregs has been progressing rapidly since the discovery that the transcription factor forkhead box protein P3 (FoxP3) is a specific molecular marker in Tregs and a master gene for Treg differentiation.2 In addition, it has been reported that butyric acid, mainly produced by Clostridium gut microbes, plays an important role in the differentiation and induction of Tregs.3
The etiology of idiopathic nephrotic syndrome (INS) in children whose histological type is 80–90% with minimal change nephrotic syndrome (MCNS) has not yet been fully elucidated. A relationship between Tregs and MCNS has been noted following a report that MCNS was present in a child with IPEX syndrome caused by a FoxP3 gene mutation.4 Subsequently, patients with INS were reported to exhibit Treg functional decline,5,6 an imbalance between Treg and T-helper type 17 (Th17) cells involved in inflammation,7,8 and a reduction in the proportion of Tregs.9 Recently, patients with steroid-sensitive INS (SSNS) have been reported to exhibit higher proportions of Tregs, compared with patients with steroid-resistant INS (SRNS).10 Previously, we reported that Tregs decreased during the onset and relapse of INS in children, and that they increased upon remission in response to steroid treatment.11 Our study also found that there was a large individual difference in the rate of increase in Tregs in response to steroid treatment for INS. Thus, we conducted this study in children with INS, to clarify the relationship between the rate of increase in Tregs due to treatment and subsequent frequent relapse.
Methods
Study population
This prospective study enrolled 25 Japanese patients with INS (median age: 4.0 years, 21 boys and 5 girls), for whom blood samples were obtained three times (at onset, in the middle of treatment, and at remission). The recruitment period lasted from January 2013 to December 2018 at Kansai Medical University Hospital, Osaka, Japan. All patients were followed up for at least 13 months (median, 47 months). The onset of INS was defined as increased excretion of urinary protein (dipstick >3+ for at least 3 sequential days or urinary protein-to-creatinine ratio >2000 mg/g creatinine) and hypoalbuminemia (<2.5 g/dl). All patients were successfully treated with prednisolone, in accordance with the guidelines of the International Study of Kidney Disease in Children12 (60 mg/[m2·day] for 4 weeks, followed by 40 mg/m2 on alternate days for 4 weeks). Remission was defined as normal serum albumin (>3.0 g/dl) and normal urinary protein excretion (dipstick trace or negative for at least 3 sequential days).13,14
The patients with INS were separated into two groups: eight did not relapse after initial response (non-relapsing [NR] group, median age: 5.4 years), whereas 17 relapsed frequently (frequently relapsing [FR] group, median age: 3.5 years). Frequent relapse was defined as two or more relapses within 6 months after initial remission, or four or more relapses within any 12-month period.13
Written informed consent for inclusion in this study was obtained from the patients’ parents. The Research Ethics Committee of Kansai Medical University approved the study protocol (Approval No. H110272).
Flow cytometry analysis of Tregs, Th1, and Th2 cells
Numbers of circulating Tregs, Th1, and Th2 cells were measured by flow cytometry. One milliliter of blood was collected via venipuncture with an anticoagulant and a 50-μl aliquot of whole blood was transferred into a sterile 6-ml centrifuge tube directly after sampling.
For Treg measurement, a fluorescein isothiocyanate-conjugated (FITC) anti-CD4 antibody (Beckman Coulter, Fullerton, CA, USA) and a cyanine dye-conjugated anti-CD25 monoclonal antibody (Beckman Coulter) were added to the tube. After the membrane had been stained and washed, permeabilization was conducted with IntraPrep™ Reagent 2 (Beckman Coulter). Residual erythrocytes were lysed at the same time. The other cells were incubated with a phycoerythrin (PE)-conjugated anti-FoxP3 monoclonal antibody (EXBIO, Vestec, Czech Republic).
The ratios of Th1 and Th2 cells in populations of peripheral memory T cells were measured by staining for CD4/CD45RO/CXCR3 (Th1) or CD4/CD45RO/CCR4 (Th2).15,16 Further, an anti-CD45RO antibody was used to differentiate between naive and memory T cells in populations of CD4-positive cells. For flow cytometric analysis, cells were incubated with antibodies [5 μl of CXCR3-PE (Cat. No. FAB160P, R&D Systems, Minneapolis, MN, USA) or CCR4-PE (Cat. No. FAB1567P, R&D Systems)/5 μl of CD45RO-FITC (BD Biosciences, San Jose, CA, USA)/5 μl of CD4-cyanine dye-conjugated (Beckman Coulter, Fullerton, CA, USA)] for 15 min.
After staining, the cells were washed twice with phosphate-buffered saline and analyzed immediately by flow cytometry (cytofluorometer Cytomics FC 500; Coulter, Hialeah, FL, USA) and CXP Cytometer Software. Data were acquired from 10,000 events per sample. The percentage of positive cells was measured from a cut-off set using isotype-matched nonspecific control antibodies. Therefore, the number of Tregs, Th1, and Th2 were calculated based on the corresponding lymphocyte count.
Quantification of cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4)
Frozen blood samples were thawed immediately prior to measurement by enzyme-linked immunosorbent assay (ELISA). Serum CTLA-4 is reportedly secreted mainly by Tregs; these levels were measured using the LEGEND MAX™ Human Soluble CTLA-4 ELISA Kit (BioLegend Co., Ltd., San Diego, CA, USA). Five patients in the NR group and 10 in the FR group had measurable CTLA-4 levels.
Fecal sampling and 16S rRNA sequencing
To analyze gut microbiota, specimens of naturally evacuated stools were obtained from 20 age-matched healthy Japanese children (median age: 4.0 years) and at first onset from pediatric patients with INS (20 patients from whom stools could be obtained before treatment), and stored at −80 °C until analysis. After frozen stool specimens were thawed, DNA was extracted from stool samples using the NucleoSpin DNA Stool Kit (Macherey-Nagel, Düren, Germany). Seven hypervariable regions, excluding v1 and v5 of the 16S rRNA region, were amplified using a 16S Metagenome Kit (Thermo Fisher Scientific, Waltham, MA, USA). After purification, libraries were constructed using the Ion Plus Fragment Library Kit (Thermo Fisher Scientific) and the Ion Xpress Barcode Adapters Kit (Thermo Fisher Scientific), in accordance with the manufacturer’s instructions. Barcoded libraries were measured using the Agilent Bioanalyzer 2000 (Agilent, Santa Clara, CA, USA), and then pooled to a final concentration of 30 pM per target. Emulsion PCR and target enrichment for template preparation were conducted using an Ion Chef Instrument and Kit (Thermo Fisher Scientific), in accordance with the manufacturer’s protocol. Sequencing analysis was conducted using an Ion PGM Sequencer (Thermo Fisher Scientific) and Ion 318 Chip (Thermo Fisher Scientific). All resulting sequence data were analyzed using the Ion Reporter Software (Thermo Fisher Scientific).
Statistical analyses
Statistical analyses were performed using the BellCurve for Excel version 3.00 software (Social Survey Research Information Co. Ltd., Tokyo, Japan). Data from each group were expressed as medians and interquartile ranges when there are no annotations. The optimal cut-off value for the rate of increase in Tregs was determined using receiver-operating characteristic curve analyses. Statistical analysis was conducted using the Mann–Whitney U test (between-group comparisons), Wilcoxon’s signed-rank test (comparisons of CTLA-4 before and after treatment), Friedman test (comparisons of Tregs before, in the middle, and after treatment), and Kruskal–Wallis test (between-group comparisons). A value of P < 0.05 was considered indicative of statistical significance.
Results
Patient characteristics and immune cell compositions
Table 1 shows the characteristics of patients with INS. At onset, urine protein level tended to be slightly higher, while serum albumin level tended to be slightly lower in the FR group; however, these differences were not statistically significant. Th1/Tregs, Th2/Tregs, and Th1/Th2 ratios were measured to determine the compositions of immunocompetent cells at the time of onset; however, no significant differences were observed between the NR and FR groups. Serum CTLA-4 (an inhibitory cytokine mainly secreted by Tregs) level tended to be higher in the NR group than in the FR group, but this difference was not statistically significant. The increase rate of CTLA-4 in response to treatment was greater in the NR group than in the FR group, but this difference was also not statistically significant.
Changes in Treg numbers at the time of INS onset and remission
Typical populations of Tregs in peripheral blood by flow cytometry at onset and at remission for INS, compared between NR and FR groups, are shown in Fig. 1a. Figure 1b shows changes in the numbers of Tregs in response to steroid treatment in the NR and FR groups. In the NR group, the median interval of blood sampling from onset to the mid-point was 3.5 days (range: 2–5 days) and that from onset to remission was 10.0 days (range: 5–15 days). In the FR group, the median interval of blood sampling from onset to the mid-point was 4.0 days (range: 3–9 days) and that from onset to remission was 10.0 days (range: 6–22 days). In the NR group, the number of Tregs at onset (69.2 µl, 35.3–85.4 µl) was significantly lower than that at remission (529.1 µl, 359.4–746.9 µl) (P = 0.0025). However, the numbers of Tregs in the middle of treatment (194.1 µl, 97.3–307.1 µl, n = 6) were similar at onset and after remission. In the FR group, the number of Tregs at remission (162.2, 143.8–201.4) also increased significantly compared with onset (74.5, 46.0–122.1, P < 0.001) and compared with the middle of treatment (105.0, 74.7–147.7, n = 12, P = 0.021). It should be noted that the rate of increase in Tregs in response to steroid treatment was significantly greater in the NR group than in the FR group (NR group: 879.2%, 583.7–1439.2%, NR group: 124.8%, 25.7–179.2%, P < 0.001) (Fig. 1c).
a Flow cytometric detection of Tregs cells in NR and FR groups. Peripheral whole-blood samples were stained with fluorescein isothiocyanate (FITC)-conjugated CD4 antibody, cyanine dye-conjugated CD25 antibody, and phycoerythrin (PE)-conjugated anti-FoxP3 antibody. The figure shows representative Treg populations by flow cytometry, before and after treatment for idiopathic nephrotic syndrome in the NR and FR groups. NR non-relapsing, FR frequently relapsing. b Changes in Treg in numbers at onset, in the middle of treatment, and remission in patients with INS. The numbers of Tregs (/µl) were increased at remission in all patients, compared with the numbers at the middle and at the onset of INS. No mid-point data were available for the patients indicated by the dotted lines. The increase in the number of Tregs was also larger in the NR group than in the FR group. In the NR group, the median interval of blood sampling from onset to the mid-point was 3.5 days (range: 2–5 days) and that from onset to remission was 10.0 days (range: 5–15 days). In the FR group, the median interval of blood sampling from onset to the mid-point was 4.0 days (range: 3–9 days) and that from onset to remission was 10.0 days (range: 6–22 days). The numbers of Tregs in healthy children (139.3/µl, 114.3–205.1/µl, n = 25) (rectangular box) were based on our previous report.11 c Rate of Treg increase in response to steroid treatment. The rate of Treg increase from onset to remission was significantly higher in the NR group than in the FR group. Central horizontal line in the box represents the median value, while bottom and top edges of the box represent the first and third quartiles, respectively. Central vertical lines extend from the box to the 90th and 10th percentiles. NR non-relapsing group, FR frequently relapsing group, INS idiopathic nephrotic syndrome.
Gut microbiota composition in patients with INS, compared with age-matched healthy children
Figure 2a shows the results of gut microbiota analysis at onset for patients with INS and age-matched healthy children. When gut microbiota were compared at the order level, there were no statistically significant differences in composition of the top five bacterial orders among the age-matched healthy children, NR group, and FR group. The Shannon index and observed species index, as indicators of bacterial diversity, showed that the median values of the FR group were lower than the median values of the healthy children; however, these differences were not statistically significant (P = 0.64 and P = 0.63, respectively) (Fig. 2b). In contrast, principal coordinate analysis revealed a different distribution of bacteria in the FR group, compared with the healthy children and the NR group (Fig. 2c).
a Relative abundances of taxa at the order level in each sample. Height color bar represents the percentage of each taxon. When gut microbiota were compared at the order level, there were no statistically significant differences in composition of the five most common bacterial orders among the age-matched healthy children, NR group, and FR group. HC healthy children, NR non-relapsing, FR frequently relapsing. b Whisker-plot diagram of Shannon and Simpson indices for each group. Figure shows Shannon and Simpson indices of healthy children, as well as NR and FR groups. There were no significant differences among the three groups for either the Shannon index or the Simpson index. c Principal coordinate analysis of healthy children, as well as NR and FR groups. Principal coordinate analysis revealed that the distributions of the healthy children and the NR group were similar, whereas the distribution of the FR group differed from the distributions of both healthy children and the NR group. HC healthy children, NR non-relapsing, FR frequently relapsing. d Relative abundances of genera to which butyric acid-producing bacteria belong, compared between patients with INS and healthy children. Compared with healthy children, patients in the FR group showed a significant reduction (P = 0.0031) in the proportion of 27 genera* to which gut microbiota butyric acid-producing bacteria belong. *These 27 genera are Propionibacterium, Odoribacter, Porphyromonas, Alistipes, Clostridium, Anaerofustis, Eubacterium, Pseudoramibacter, Anaerostipes, Butyrivibrio, Coprococcus, Lachnoanaerobaculum, Roseburia, Shuttleworthia, Anaerococcus, Peptoniphilus, Peptoclostridium, Anaerotruncus, Faecalibacterium, Subdoligranulum, Holdemanella, Acidaminococcus, Acetonema, Megasphaera, Fusobacterium, Brachyspira, and Treponema. Central horizontal line in box represents the median value, while bottom and top edges of box represent first and third quartiles, respectively. Central vertical lines extend from box to 90th and 10th percentiles. HC healthy children, NR non-relapsing, FR frequently relapsing, INS idiopathic nephrotic syndrome.
Because butyric acid produced by gut microbiota is important for the differentiation and induction of Tregs, we focused on the following 27 genera, which include 61 species of known butyrate-producing bacteria:17 Propionibacterium, Odoribacter, Porphyromonas, Alistipes, Clostridium, Anaerofustis, Eubacterium, Pseudoramibacter, Anaerostipes, Butyrivibrio, Coprococcus, Lachnoanaerobaculum, Roseburia, Shuttleworthia, Anaerococcus, Peptoniphilus, Peptoclostridium, Anaerotruncus, Faecalibacterium, Subdoligranulum, Holdemanella, Acidaminococcus, Acetonema, Megasphaera, Fusobacterium, Brachyspira, and Treponema.17 The results showed that the proportion of the 27 genera to which butyrate-producing bacteria belong was significantly reduced in the FR group (4.3%), compared with the healthy children (15.6%) (P = 0.0031). In contrast, there was no significant difference in the proportion of butyric acid-producing bacteria between the NR group (8.7%) and healthy children (Fig. 2d).
Receiver-operating characteristic curve of the rate of Treg increase for predicting subsequent development of frequently relapsing INS
The receiver-operating characteristic curve of the increase rate of Tregs is shown in Fig. 3. A cut-off value of <400% in the increase rate of Treg at onset yielded a sensitivity of 94% and a specificity of 88% for predicting risk of subsequent development of frequently relapsing INS (FRNS) (area under receiver-operating characteristic curve = 0.93).
Discussion
In patients with MCNS with high proteinuria, Shalhoub18 hypothesized that proteinuria appears due to T cell dysfunction and associated changes in vascular permeability-enhancing factor; to the best of our knowledge, there have been no consistent results indicative of these changes. The current theory is that the pathogenesis of MCNS is due to a complicated mechanism, which includes the involvement of immunocompetent cells.
Tregs are a class of T lymphocytes that negatively regulate abnormal and excessive immune responses; they are responsible for maintaining immune tolerance and immune homeostasis by suppressing pathological immune responses, such as autoimmunity, inflammation, and allergies.1 The transcription factor Foxp3 is essential for Tregs differentiation and functions as a master transcription factor.19 Regarding the relationship between Tregs and MCNS, Shimada et al.20 proposed a “two-hit” podocyte immune disorder underlying MCNS. Briefly, the “first hit” involves induction of podocyte expression of CD80 (also known as B7-1) in response to a circulating factor (such as a cytokine, allergen, or microbial product). The increased CD80 expression results in transient podocyte shape changes and proteinuria, which can be restored by CTLA-4 and interleukin-10, mainly secreted by Tregs. The “second hit” involves dysfunction of this autoregulatory mechanism controlled by Tregs. Functional or quantitative reductions in Tregs lead to persistent CD80 expression on podocytes and prolonged proteinuria in MCNS. Consistent with this hypothesis, the urinary soluble CD80/CTLA-4 ratio was reported to be >100-fold higher in patients with MCNS relapse than in patients with remission,21 and SSNS patients in remission had lower urinary CD80 levels and higher CTLA-4 levels than patients in relapse22 In addition, there have been many reports of functional decline and reduced numbers of Tregs in patients with INS.5,6,7,8,23 We also reported that the number of Tregs at the onset of INS was significantly lower than the number in age-matched healthy control children; however, the number of Tregs at the time of steroid-induced remission was significantly higher than at the onset of INS. In addition, the change in serum CTLA-4 levels from onset to remission exhibited a statistically significant positive correlation with Tregs number.11 In this study, the increased rate of CTLA-4 in response to steroid treatment did not significantly differ between groups; however, it was greater in the NR group than in the FR group, similar to the rate of Tregs increase. Jaiswal et al.24 compared Th1/Tregs and Th2/Tregs ratios in both SSNS and SRNS groups; they found that the Th1/Tregs and Th2/Tregs ratios were significantly greater in the SRNS group than in the SSNS group. In contrast, we found no significant differences in the Th1/Tregs or Th2/Tregs ratios between the NR and FR groups. We presume that no significant difference was observed because all of our patients with INS had SSNS. Mounting evidence, including our previous study, has suggested that functional or quantitative reductions in Tregs are strongly associated with proteinuria in MCNS, although the cause of this abnormality in Tregs is unclear.
Butyric acid, a type of short-chain fatty acid mainly produced by Clostridium in the gut microbiota, has been reported to play an important role in inducing Tregs differentiation.3 Butyric acid is known to have a strong histone deacetylase inhibitory effect,25 and significantly enhances histone acetylation in the promoter and enhancer regions of the Foxp3 gene, which encodes the Tregs master transcription factor. As mentioned above, our previous study revealed that the number of Tregs at the onset of INS was lower than that in healthy children, but the cause of this reduction was unclear. Therefore, we investigated whether butyric acid-producing bacteria were reduced due to dysbiosis of the gut microbiota, thus reducing differentiation of Tregs. Analysis of the gut microbiota in the healthy children, as well as in the NR and FR groups, showed no statistically significant differences in α diversity. However, the distribution of β-diversity differed between the FR group and the other two groups, as shown in Fig. 2c; this suggested that patients with FRNS had dysbiosis, compared with the other two groups of children. Furthermore, our results showed that the relative abundances of genera including butyric acid-producing bacteria were significantly lower in the stools of patients with INS than in the stools of healthy children. Consistent with these findings, we previously reported that the amounts of butyrate in stools were also reduced in children with relapsing INS.26 Taken together, our current and prior results suggest that gut dysbiosis is related to the onset of INS.27 Genetic and environmental factors may contribute to dysbiosis in patients with INS. Both types of factors have been postulated to affect the gut microbiota in children, including human leukocyte antigen and dietary differences: genetic differences in major histocompatibility complex (MHC) antigens have been reported to affect the gut microbiota and to be involved in the development of various diseases,28,29 while several studies have reported that the diet content can change the gut microbiota.30,31 In addition, other studies have suggested an association between genetic factors, especially MHC class II molecules, and the etiology of MCNS,32,33,34,35,36 including a recent report in Japanese MCNS patients.37 A further study found that dietary measures, such as an elemental diet or removing milk and gluten, could induce remission in patients with MCNS.38 Dysbiosis observed in Japanese children with relapsing INS, as in our current and previous study, was therefore likely to be caused by genetic and environmental factors, including diet, suggesting that dietary management may therefore be a useful relapse-prevention measure. In terms of clinical significance, the present study demonstrated that a rate of Treg increase in response to steroid treatment ≤400% was associated with a high risk of developing frequent relapse in children with INS; these patients exhibited gut dysbiosis, including a marked reduction in the proportion of butyric acid-producing bacteria. These results suggest that patients with FRNS exhibit dysbiosis characterized by a reduction in the proportion of butyrate-producing bacteria, which may lead to insufficient differentiation and induction of Tregs specifically within the intestinal tract.
The present study had several limitations. First, in this study, Treg numbers and proportions of Tregs were only measured in INS children, and no data for healthy children could be obtained. However, we presumed that the Tregs data for healthy children obtained in our previous study11 could be used for comparison because the previous data were acquired with the same method and equipment. Second, measurement of Th17 cells (i.e., activated T cells) together with Tregs would be more useful for understanding the pathogenesis of INS; however, this measurement was not performed in the present study. Third, butyric acid-producing bacteria were analyzed at the genus level, rather than at the species level, due to performance limitations of the sequencer.
In conclusion, a low rate of Tregs increase was associated with subsequent frequent INS relapse. The increase in Tregs in response to steroid treatment was small when dysbiosis was present in the gut microbiota of patients with INS, particularly when the proportion of butyrate-producing bacteria was considerably reduced. Therefore, we presume that improvement of dysbiosis by administration of probiotics and prebiotics may enhance the rate of Tregs increase, thus preventing frequent relapse.
References
Sakaguchi, S., Yamaguchi, T., Nomura, T. & Ono, M. Regulatory T cells and immune tolerance. Cell 133, 775–787 (2008).
Hori, S., Nomura, T. & Sakaguchi, S. Control of regulatory T cell development by the transcription factor Foxp3. Science 299, 1057–1061 (2003).
Furusawa, Y. et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature 504, 446–450 (2013).
Hashimura, Y. et al. Minimal change nephrotic syndrome associated with immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome. Pediatr. Nephrol. 24, 1181–1186 (2009).
Araya, C. et al. T regulatory cell function in idiopathic minimal lesion nephrotic syndrome. Pediatr. Nephrol. 24, 1691–1698 (2009).
Yildiz, B., Cetin, N., Kural, N. & Colak, O. CD19+ CD23+ B cells, CD4+ CD25+ T cells, E-selectin and interleukin-12 levels in children with steroid sensitive nephrotic syndrome. Ital. J. Pediatr. 39, 42 (2013).
Shao, X. S. et al. The prevalence of Th17 cells and FOXP3 regulate T cells (Treg) in children with primary nephrotic syndrome. Pediatr. Nephrol. 24, 1683–1690 (2009).
Liu, L. L. et al. Th17/Treg imbalance in adult patients with minimal change nephrotic syndrome. Clin. Immunol. 139, 314–320 (2011).
Bertelli, R. et al. Regulatory T cells and minimal change nephropathy: in the midst of a complex network. Clin. Exp. Immunol. 183, 166–174 (2016).
Guimaraes, F. T. L. et al. Pediatric patients with steroid-sensitive nephrotic syndrome have higher expression of T regulatory lymphocytes in comparison to steroid-resistant disease. Front. Pediatr. 7, 114 (2019).
Tsuji, S. et al. Regulatory T cells and CTLA-4 in idiopathic nephrotic syndrome. Pediatr. Int. 59, 643–646 (2017).
Tarshish, P., Tobin, J. N., Bernstein, J. & Edelmann, C. M. Jr Prognostic significance of the early course of minimal change nephrotic syndrome: report of the International Study of Kidney Disease in Children. J. Am. Soc. Nephrol. 8, 769–776 (1997).
Lombel, R. M., Gipson, D. S. & Hodson, E. M. Kidney Disease: Improving Global O. Treatment of steroid-sensitive nephrotic syndrome: new guidelines from KDIGO. Pediatr. Nephrol. 28, 415–426 (2013).
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group. KDIGO Clinical Practice Guideline for Glomerulonephritis. Kidney Int. Suppl. 2, 139–274 (2012).
Sallusto, F., Lenig, D., Mackay, C. R. & Lanzavecchia, A. Flexible programs of chemokine receptor expression on human polarized T helper 1 and 2 lymphocytes. J. Exp. Med. 187, 875–883 (1998).
Bonecchi, R. et al. Differential expression of chemokine receptors and chemotactic responsiveness of type 1 T helper cells (Th1s) and Th2s. J. Exp. Med. 187, 129–134 (1998).
Haak, B. W. et al. Impact of gut colonization with butyrate-producing microbiota on respiratory viral infection following allo-HCT. Blood 131, 2978–2986 (2018).
Shalhoub, R. J. Pathogenesis of lipoid nephrosis: a disorder of T-cell function. Lancet 2, 556–560 (1974).
Sakaguchi, S., Miyara, M., Costantino, C. M. & Hafler, D. A. FOXP3+ regulatory T cells in the human immune system. Nat. Rev. Immunol. 10, 490–500 (2010).
Shimada, M. et al. Minimal change disease: a “two-hit” podocyte immune disorder? Pediatr. Nephrol. 26, 645–649 (2011).
Garin, E. H. et al. Urinary CD80 excretion increases in idiopathic minimal-change disease. J. Am. Soc. Nephrol. 20, 260–266 (2009).
Zhao, B. et al. CD80 and CTLA-4 as diagnostic and prognostic markers in adult-onset minimal change disease: a retrospective study. PeerJ 6, e5400 (2018).
Bertelli, R. et al. Regulation of innate immunity by the nucleotide pathway in children with idiopathic nephrotic syndrome. Clin. Exp. Immunol. 166, 55–63 (2011).
Jaiswal, A. et al. Regulatory and effector T cells changes in remission and resistant state of childhood nephrotic syndrome. Indian J. Nephrol. 24, 349–355 (2014).
Davie, J. R. Inhibition of histone deacetylase activity by butyrate. J. Nutr. 133, 2485S–2493S (2003).
Tsuji, S. et al. Gut microbiota dysbiosis in children with relapsing idiopathic nephrotic syndrome. Am. J. Nephrol. 47, 164–170 (2018).
Kaneko, K., Tsuji, S. & Kimata, T. Role of gut microbiota in idiopathic nephrotic syndrome in children. Med. Hypotheses 108, 35–37 (2017).
Kubinak, J. L. et al. MHC variation sculpts individualized microbial communities that control susceptibility to enteric infection. Nat. Commun. 6, 8642 (2015).
Bolnick, D. I. et al. Major histocompatibility complex class IIb polymorphism influences gut microbiota composition and diversity. Mol. Ecol. 23, 4831–4845 (2014).
De Filippo, C. et al. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc. Natl Acad. Sci. USA 107, 14691–14696 (2010).
Wu, G. D. et al. Linking long-term dietary patterns with gut microbial enterotypes. Science 334, 105–108 (2011).
Lane, B. M., Cason, R., Esezobor, C. I. & Gbadegesin, R. A. Genetics of childhood steroid sensitive nephrotic syndrome: an update. Front. Pediatr. 7, 8 (2019).
Adeyemo, A. et al. HLA-DQA1 and APOL1 as risk loci for childhood-onset steroid-sensitive and steroid-resistant nephrotic syndrome. Am. J. Kidney Dis. 71, 399–406 (2018).
Debiec, H. et al. Transethnic, genome-wide analysis reveals immune-related risk alleles and phenotypic correlates in pediatric steroid-sensitive nephrotic syndrome. J. Am. Soc. Nephrol. 29, 2000–2013 (2018).
Kobayashi, Y. et al. Association of HLA-DRw8 and DQw3 with minimal change nephrotic syndrome in Japanese adults. Kidney Int. 28, 193–197 (1985).
Cheung, W. et al. Increased HLA- A*11 in Chinese children with steroid-responsive nephrotic syndrome. Pediatr. Nephrol. 17, 212–216 (2002).
Jia, X. et al. Strong association of the HLA-DR/DQ locus with childhood steroid-sensitive nephrotic syndrome in the Japanese population. J. Am. Soc. Nephrol. 29, 2189–2199 (2018).
Uy, N., Graf, L., Lemley, K. V. & Kaskel, F. Effects of gluten-free, dairy-free diet on childhood nephrotic syndrome and gut microbiota. Pediatr. Res. 77, 252–255 (2015).
Simone, R. et al. A soluble form of CTLA-4 is present in paediatric patients with acute lymphoblastic leukaemia and correlates with CD1d+ expression. PLoS ONE 7, e44654 (2012).
Acknowledgements
We thank Ryan Chastain-Gross, Ph.D., from the Edanz Group (https://en-author-services.edanzgroup.com) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
K.K and S.T.: research idea and study design; S.T., S.A., Y.A., S.Y., T.K., and M.H.: data acquisition; S.T., S.A., T.Y., and J.K.: data analysis/interpretation; S.T. and S.A.: statistical analysis; K.K. and A.A.: supervision or mentorship. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Written informed consent was obtained from the parents of the patients enrolled in this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tsuji, S., Akagawa, S., Akagawa, Y. et al. Idiopathic nephrotic syndrome in children: role of regulatory T cells and gut microbiota. Pediatr Res 89, 1185–1191 (2021). https://doi.org/10.1038/s41390-020-1022-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-1022-3
This article is cited by
-
Clostridium butyricum inhibits the inflammation in children with primary nephrotic syndrome by regulating Th17/Tregs balance via gut-kidney axis
BMC Microbiology (2024)
-
The immunopathogenesis of idiopathic nephrotic syndrome: a narrative review of the literature
European Journal of Pediatrics (2022)
-
Structural and functional changes in the kidney caused by adverse fetal and neonatal environments
Molecular Biology Reports (2022)