Abstract
Background
Mechanisms of chemotherapy-associated neurotoxicity are poorly understood, and therefore, prevention strategies have not been developed. We hypothesized that a subgroup of children receiving intrathecal cytarabine develops subclinical vasospasm, which may contribute to long-term neurocognitive sequelae of cancer.
Methods
We used transcranial Doppler ultrasound to serially evaluate cerebral blood flow velocities in participants ≤25 years old receiving intrathecal cytarabine for hematologic malignancies.
Results
Four of 18 participants (22%) met the criteria for subclinical vasospasm within 4 days of intrathecal cytarabine administration. The distribution of oncologic diagnoses differed between the vasospasm and non-vasospasm groups (p = 0.02). Acute myeloid leukemia was identified as a potential risk factor for vasospasm. Children with vasospasm were more likely to have received intravenous cytarabine (75% versus 0%, p = 0.01) and less likely to have received steroids (25% versus 100%, p = 0.01).
Conclusions
A subpopulation of children with hematologic malignancies develops subclinical vasospasm after intrathecal cytarabine treatment. Future research is needed to determine the long-term clinical consequences of cerebral vasospasm in this population.
Impact
-
A subset of children with hematologic malignancies who receive intrathecal cytarabine experience subclinical cerebral vasospasm, as measured by transcranial Doppler ultrasound.
-
Of children receiving intrathecal cytarabine, those who develop cerebral vasospasm are more likely to have diagnosis of acute myeloid leukemia, more likely to receive concurrent intravenous cytarabine, and less likely to receive steroids as part of their chemotherapy regimen, as compared with children without vasospasm.
-
Future research is needed to determine if vasospasm during chemotherapy is associated with higher rates of neurocognitive dysfunction, and if so, to focus on prevention of these long-term sequelae of childhood cancer.
Similar content being viewed by others
Introduction
The burden of cancer-related neurological sequelae is growing as chemotherapeutic agents become more effective and survivorship increases.1,2 Childhood cancer treatment regimens are associated with significant neurotoxicity.3 However, because mechanisms of chemotherapy-associated neurotoxicity are not well-understood, appropriate prevention strategies have not been developed. Treatment-related side effects continue to produce long-term morbidity and sometimes compel modification of chemotherapy regimens to alternatives that may be less effective.
Cytarabine (cytosine arabinoside or ara-C) is a pyrimidine nucleoside analog antineoplastic agent that is an integral part of combination chemotherapy regimens for childhood cancer. As the central nervous system (CNS) can act as a sanctuary site for malignant cells where they can elude the effects of systemically administered chemotherapy, cytarabine is commonly administered intrathecally (IT) on the first day of induction chemotherapy for childhood hematologic malignancies for prophylaxis against CNS relapse. Cytarabine is associated with significant neurotoxicity, both with intravenous (IV) and IT administration.4,5 High-dose IV cytarabine has been associated with an array of neurotoxic effects including peripheral neuropathy, seizures, encephalopathy, and acute cerebellar syndrome.4,6,7 Intrathecal cytarabine most commonly has been reported to cause myelopathy of variable severity, with some cases resulting in permanent paraplegia, but has also been associated with stroke and posterior reversible encephalopathy syndrome (PRES).4,8,9,10,11,12,13,14 Neurocognitive impairment is also substantial after chemotherapy for childhood leukemia,15 though the contribution of IT cytarabine to cognitive and behavioral dysfunction is not known.
The mechanism of cytarabine-associated neurotoxicity is unknown, but multiple recent clinical case reports and series describe severe diffuse cerebral vasospasm leading to stroke and/or PRES in children 4–16 days after IT cytarabine administration.9,10,11,12,13 These cases suggest a possible role for cerebrovascular dysfunction in the pathogenesis of cytarabine toxicity. Chemotherapy-associated cerebral vasospasm may be significantly under-recognized given that angiography is not routinely performed unless it leads to overt neurologic manifestations such as stroke. Subclinical vasospasm may lead to more subtle forms of neurotoxicity such as silent cerebral infarcts, headache, or neurocognitive impairment in a larger group of patients. Subtle neurotoxicity has been demonstrated to result from subclinical vasospasm in other disease processes. For example, in patients with aneurysmal subarachnoid hemorrhage, cerebral vasospasm has been identified as a predictor of cognitive impairment after discharge.16,17 Interestingly, this association has not been demonstrated in more recent studies, which some authors have suggested may be related to improved vasospasm treatment with calcium channel blockade and induced hypertension, hypervolemia, and hemodilution (“triple H” therapy).18 Subclinical cerebral vasospasm has also been reported to play a role in neurologic disability and silent radiographic brain injury in the settings of traumatic brain injury19 and cocaine use,20 respectively. Similar to these patients in other settings, recognition and treatment of subclinical vasospasm could potentially prevent both overt and subtle downstream adverse neurologic consequences.
We hypothesized that a subgroup of children receiving IT cytarabine would have evidence of subclinical vasospasm on transcranial Doppler (TCD) ultrasound. In addition, we aimed to identify potential risk factors for vasospasm.
Methods
In this prospective self-controlled case series, we enrolled subjects ≤25 years old admitted to the Johns Hopkins Children’s Center for initiation of chemotherapy with IT cytarabine for newly diagnosed hematologic malignancy. Exclusion criteria included history of stroke or PRES, prior neuroimaging abnormalities, prior chemotherapy, or administration of IT medications other than cytarabine. All families signed informed consent and the study was approved by the institutional review board.
Using TCD ultrasound, we measured cerebral blood flow velocity (CBFV) in seven cerebral vessels at baseline (pretreatment) and at 1, 4, and 8 days after administration of IT cytarabine. These days were chosen because they were in a window when vasospasm was expected to be maximal based on prior literature and because they are prior to administration of different IT medications on day 8, so as to isolate the effects of IT cytarabine on the intracranial vasculature. Each TCD examination included insonation of at minimum the basilar artery and the bilateral intracranial internal carotid arteries (ICA), middle cerebral arteries (MCA) at the M1 segment, and anterior cerebral arteries (ACA). The primary outcome was the change in MCA CBFVs averaged over both sides. Demographic, laboratory, medication, and clinical data were collected at enrollment and throughout the duration of the study. Systemic blood pressure, body temperature, and heart rate were measured at baseline and with each TCD study. Participants or their parents were called approximately 1 month after enrollment to administer a standardized questionnaire about neurological symptoms since discharge, including specific inquiries regarding stroke, headaches, seizures, vision changes, and focal neurologic deficits.
We determined the proportion of subjects who had significant elevations in CBFV compared with their own baseline pretreatment measurements. Given the hematologic abnormalities inherent in untreated leukemia, such as anemia, abnormal baseline TCD studies were expected. We therefore defined vasospasm as an increase of two standard deviations (based on age-based normative data21) above each child’s baseline MCA CBFV. When data were available, we calculated the Lindegaard ratios, though we did not use this to define vasospasm as external ICA velocities were not obtained for all participants.
Data were compared between study participants and children that were eligible but not enrolled, as well as between participants with and without vasospasm, using Wilcoxon rank sum tests for continuous variables and Fisher’s exact tests for categorical variables. For statistical comparison between children with and without vasospasm, CBFVs in the M1 segment of the MCA were used. Results were considered statistically significant if p < 0.05.
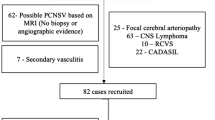
Results
Between March 2016 and September 2019, 73 patients were screened, 65 were eligible, and 18 enrolled and completed the study. Reasons for nonenrollment included: insufficient time to complete baseline TCD prior to IT cytarabine administration (n = 39) and declined participation (n = 8). There were no significant differences between enrolled subjects and eligible patients that did not enroll (Table 1). The 18 enrolled subjects were ages 2–23 years with diagnoses of pre-B acute lymphocytic leukemia (ALL) (n = 10), T-cell ALL (n = 3), acute myeloid leukemia (AML) (n = 3), and B-cell lymphoma (n = 2). No subject had exposures known to cause cerebral vasospasm, including marijuana, selective serotonin reuptake inhibitors, and decongestants. All data points were acquired for 12 subjects; the remaining participants had one (n = 5) or two (n = 1) missing TCD studies due to agitation in one instance and unavailability/early discharge of the other five subjects.
All 18 subjects had significantly globally elevated CBFVs (MCA, ACA, intracranial ICA, basilar artery) at baseline compared to age-based norms, with median CBFV 22 cm/s (interquartile range [IQR] 12–33 cm/s) above reference values (p < 0.01).21 Baseline median velocity was 107.5 cm/s (IQR 94.1–114.4 cm/s) in the MCA and 58 cm/s (IQR 46–60 cm/s) in the basilar artery.
With respect to post-cytarabine CBFVs, four participants (22%) met criteria for vasospasm during induction chemotherapy (Fig. 1; see Table 2 for chemotherapy regimens). Their TCD studies revealed substantial increases in anterior circulation CBFVs after administration of IT cytarabine, with peak MCA CBFVs increasing 45% (44.5 cm/s), 43% (35.5 cm/s), 40% (44.5 cm/s), and 34% (38.5 cm/s) above baseline values. Lindegaard ratios, when performed, confirmed vasospasm with ratios between 3 and 4, though this could not be calculated for all studies as external ICA velocities were not routinely measured. In contrast to anterior circulation velocities, basilar artery CBFV did not change after cytarabine. The other 14 subjects (78%) did not meet the criteria for vasospasm. In most subjects who did not meet the criteria for vasospasm, over the course of the four studies, there was a slow decline in CBFVs over time (Fig. 1). Among subjects who did not meet the criteria for vasospasm, mean M1 CBFV decreased from 103.5 cm/s at baseline to 95.2 cm/s by day 8. Of note, over this same time period, median hematocrit increased from 27.6 to 30.3%.
Age and sex were not significantly different between the vasospasm and non-vasospasm groups, though there was a nonsignificant trend toward younger children (6.2 versus 10.9 years, p = 0.19) and more females (75% versus 36%, p = 0.27) in the vasospasm group (Table 3). Race and ethnicity did not differ between the vasospasm and non-vasospasm groups. The distribution of oncologic diagnoses differed between groups (p = 0.02); all children with AML and only one other child met the criteria for vasospasm. Children with vasospasm were more likely to receive IV cytarabine (75% versus 0%, p = 0.01) and less likely to receive steroids (25% versus 100%, p = 0.01) prior to reaching peak CBFV. There was no difference in proportions of children who received additional IT cytarabine during the study period, baseline CBFVs, hematocrit, or change in hematocrit from baseline between the vasospasm and non-vasospasm groups. No child in either group received calcium channel blockers or other antihypertensive medication, selective serotonin reuptake inhibitors, or decongestants during the study period.
There was no clear relationship between systemic blood pressure, body temperature, or heart rate and CBFV in children who met the criteria for vasospasm. In the vasospasm group, at the time of each participant’s peak CBFV, the systolic blood pressure was on average 14 points higher than at baseline. In three of the four subjects, blood pressure was elevated for age at the time the CBFV peaked. However, in all three of those subjects, CBFV remained elevated (and continued to meet criteria for vasospasm) on subsequent studies despite blood pressure returning to normal values. With regards to temperature and heart rate, one child who met the criteria for vasospasm was febrile and tachycardic at the time his CBFV peaked. However, his CBFV remained elevated on a subsequent TCD study despite normalization of heart rate and temperature to baseline values. At the time the CBFV peaked for each of the other three participants, temperature was within 1 °C of baseline and heart rate was within 15 points of baseline, with all temperatures and heart rates within normal limits for age.
No serious neurologic complications were discovered during telephone follow-up. Headache was the only reported neurologic event and occurred with similar frequency in children with and without vasospasm (25% versus 21%, p = 0.9). In all cases of headache, the subjects’ parents reported temporal association of the headaches to lumbar punctures, though the description of the headache was variable. There were no reported seizures, focal neurological deficits, episodes of confusion or decreased responsiveness, vision changes, or other neurologic concerns.
Discussion
In this study of children undergoing induction chemotherapy for new onset hematologic malignancy, we identified a subgroup of children who developed subclinical cerebral vasospasm after receiving IT cytarabine. Three of the four children with cerebral vasospasm in this study had AML and consequently received twice-daily IV cytarabine throughout the study and did not receive steroids, unlike children with other oncologic diagnoses. Of note, one child with AML (subject “D”) received a single dose of IV methylprednisolone (as a pretreatment for IV gemtuzumab) but only after meeting the criteria for vasospasm. It is therefore unclear if vasospasm in these children is related to treatment effects versus malignancy subtype. IT cytarabine initial and cumulative doses did not differ between children with and without vasospasm, though additional IT doses were not given until after study day 4. The short duration of this study limited our analysis of the effects of cumulative intrathecal cytarabine exposure on the cerebral vasculature. However, systemic cytarabine, which was administered more frequently in children who developed vasospasm, crosses the blood−brain barrier and could propagate effects of intrathecal cytarabine. Interestingly, concomitant IV and IT cytarabine administration has previously been postulated as a risk factor for neurotoxicity.4,22,23 Pharmacokinetic studies demonstrate that after IV cytarabine infusion, the CSF drug concentration exceeds the plasma concentration due to the long half-life of cytarabine in the CSF.24 Therefore, twice-daily administration of systemic cytarabine could propagate the effects of IT cytarabine by supplementing CSF levels through continuous dosing. It is noteworthy that the study participant with delayed elevation of CBFV (subject “D” in Fig. 1) received IV cytarabine only after the TCD on day 1 was performed; this may potentially explain why this subject did not meet the criteria for vasospasm until day 4, in contrast to participants “A” and “C” who received twice-daily IV cytarabine starting prior to the TCD on day 1. The three subjects that received twice-daily IV cytarabine also received IV daunorubicin every other day starting on day 1 of the study. Daunorubicin is not known to affect cerebral vasculature or blood flow.
Alternatively, steroids may play a protective role against vasospasm. This is supported by one previously published case in which an adolescent with lymphoma who developed PRES after IT cytarabine administration was successfully treated with methylprednisolone.25 However, this diverges from other reports that suggest that methylprednisolone may instead be a risk factor for pediatric PRES.26 These contradictory notions may be explained by pathophysiological differences between PRES associated with cytarabine versus other etiologies, such as hypertension, which would be exacerbated by steroids. Further study is needed to explore the role of underlying malignancy versus therapies in the development of vasospasm.
All subjects had elevated CBFVs at baseline. Lindegaard ratios at baseline, when calculated, ranged from 1.4 to 2.7, which in the setting of elevated CBFVs is suggestive of hyperemia.27,28 Therefore, these elevations are likely secondary to hematologic abnormalities associated with leukemia, such as severe anemia. Baseline CBFV did not differ between children who ultimately developed vasospasm versus those who did not. Among subjects who did not meet the criteria for vasospasm, the decline in CBFV from baseline to day 8 was paralleled by an increase in hematocrit over the same time frame. While the gradual CBFV normalization over time may be related to transfusions and oncologic therapies, future study is needed to explore the reasons for this observation.
We also explored the relationship between physiologic parameters, including blood pressure, temperature, and heart rate, and CBFV in participants in our sample. Measured blood flow velocity can be higher with higher systemic blood pressures despite an intact autoregulatory system.29 The effect of temperature on cerebral blood flow velocities is not well established. Although one study showed an inverse relationship between temperature and flow velocities,30 a more recent study of CBFV in postcardiac arrest patients treated with hypothermia does not support a relationship between temperature and flow velocities.31 In our cohort, children who met the criteria for vasospasm did on average have higher blood pressure and temperature at the time of peak CBFV when compared to baseline, but the differences were not sufficient to explain the observed drastic increase in CBFV and the children continued to meet the criteria for vasospasm days after the hemodynamic parameters normalized. Therefore, the changes in systemic physiologic parameters observed in the four children who met the criteria for vasospasm are highly unlikely to explain the observed CBFV elevations.
No participant experienced significant neurological complications at 1-month follow-up. It is possible that with extended follow-up, formal neuropsychological assessment, or in a larger sample, neurologic sequelae would emerge. Though the current study cannot link the presence of vasospasm during induction chemotherapy with subsequent neurocognitive deficits, it is possible that subclinical vasospasm may contribute to neurocognitive impairment in a subset of children through impaired cerebral perfusion or silent cerebral infarcts, akin to the sickle cell population in which silent cerebral infarctions are associated with cognitive impairment.32 A larger study with extended follow-up is needed to determine if vasospasm during chemotherapy is associated with higher rates of neuropsychological dysfunction in children with hematologic malignancies. If so, this may be an opportunity for therapeutic intervention; high-risk patients could be screened with TCD and vasospasm could be treated, for example with calcium channel blockers, to prevent or mitigate the cognitive sequelae of childhood cancer.
Limitations of this study include small sample size and multiple potential confounders (such as hematocrit) that could not adequately be adjusted for in our analysis, though no differences in these parameters across groups were seen. Additionally, while pediatric studies have defined vasospasm as 2 standard deviations above age-based normative values,21,33 significant baseline CBFV elevations precluded our use of this definition. We therefore defined vasospasm as MCA CBFV increase ≥2 standard deviations from each subjects’ baseline velocity. It is possible that CBFV elevations seen in this study may be due to general treatment effects, the mere act of accessing the intrathecal space, or anxiety at the time of TCD testing. Lindegaard ratios were not routinely measured, so CBFV elevations in some cases may have been related to hyperemia instead of vasospasm. However, hyperemia is an unlikely cause for sudden changes in CBFV after IT cytarabine as we saw in the vasospasm group, especially in the absence of significant changes in other laboratory or hemodynamic parameters. In future studies, we will standardly perform Lindegaard ratios to definitively differentiate between hyperdynamic blood flow and vasospasm. Future studies will also include vascular imaging such as magnetic resonance or computed tomography angiography. This will be critical to confirm the presence of intracranial vasospasm, particularly in light of data in children with sickle cell disease that CBFV do not always correlate with the presence and severity of vascular stenosis in this population.34 Furthermore, neuroimaging could assess for silent cerebral infarcts, which are known to impact cognition in children with sickle cell disease.32 Finally, future studies including participants receiving IV cytarabine without IT administration are needed to isolate the effect of IV cytarabine.
These data suggest that there may be a subpopulation of children at risk for subclinical vasospasm in the days after IT cytarabine treatment, and that it may be possible to identify high-risk patients and prevent treatment-related CNS consequences. Our data suggest that children with AML are at highest risk for subclinical vasospasm, though whether that is due to underlying malignancy-specific factors or differences in treatment remains unknown. As chemotherapeutic regimens continue to become more effective and cancer survivorship increases, recognition and prevention of treatment-related neurotoxicity become more essential. Future research is needed to determine if subclinical vasospasm in leukemia patients receiving chemotherapy may be a harbinger of neurologic sequelae, and if so, to focus on prevention of these complications in cases of cerebral vasospasm.
References
Bright, C. et al. Risk of cerebrovascular events in 178 962 five-year survivors of cancer diagnosed at 15 to 39 years of age: The TYACSS (teenage and young adult cancer survivor study). Circulation 135, 1194–1210 (2017).
Armstrong, C. & Sun, L. R. Neurological complications of pediatric cancer. Cancer Metastasis Rev. https://doi.org/10.1007/s10555-020-09847-0 (2020).
Sun, L. R. & Cooper, S. Neurological complications of the treatment of pediatric neoplastic disorders. Pediatr. Neurol. 85, 33–42 (2018).
Baker, W. J., Royer, G. L. & Weiss, R. B. Cytarabine and neurologic toxicity. J. Clin. Oncol. 9, 679–693 (1991).
Resar, L. M. S. et al. Acute neurotoxicity after intrathecal cytosine arabinoside in two adolescents with acute lymphoblastic leukemia of B‐cell type. Cancer 71, 117–123 (1993).
Openshaw, H., Slatkin, N. E., Stein, A. S., Hinton, D. R. & Forman, S. J. Acute polyneuropathy after high dose cytosine arabinoside in patients with leukemia. Cancer 78, 1899–1905 (1996).
Saito, T. et al. Peripheral neuropathy caused by high-dose cytosine arabinoside treatment in a patient with acute myeloid leukemia. J. Infect. Chemother. 12, 148–151 (2006).
Werner, R. A. Paraplegia and quadriplegia after intrathecal chemotherapy. Arch. Phys. Med. Rehabil. 69, 1054 (1988).
Tibussek, D. et al. Severe cerebral vasospasm and childhood arterial ischemic stroke after intrathecal cytarabine. Pediatrics 137, e20152143 (2016).
Pound, C. M., Keene, D. L., Udjus, K., Humphreys, P. & Johnston, D. L. Acute encephalopathy and cerebral vasospasm after multiagent chemotherapy including PEG-asparaginase and intrathecal cytarabine for the treatment of acute lymphoblastic leukemia. J. Pediatr. Hematol. Oncol. 29, 183–186 (2007).
Yoon, J. H. et al. Diffuse cerebral vasospasm with infarct after intrathecal cytarabine in childhood leukemia. Pediatr. Int. 56, 921–924 (2014).
Hiraide, T. et al. Recurrent posterior reversible encephalopathy due to vasospasm and cerebral hypoperfusion in in acute leukemia: a case report. No. To. Hattatsu. 47, 449 (2015).
Henderson, R. D., Rajah, T., Nicol, A. J. & Read, S. J. Posterior leukoencephalopathy following intrathecal chemotherapy with MRA-documented vasospasm. Neurology 60, 326–328 (2003).
Saito, B. et al. Reversible posterior leukoencephalopathy syndrome after repeat intermediate-dose cytarabine chemotherapy in a patient with acute myeloid leukemia. Am. J. Hematol. 82, 304–306 (2007).
Cheung, Y. T. & Krull, K. R. Neurocognitive outcomes in long-term survivors of childhood acute lymphoblastic leukemia treated on contemporary treatment protocols: a systematic review. Neurosci. Biobehav. Rev. 53, 108–120 (2015).
Stenhouse, L. M., Knight, R. G., Longmore, B. E. & Bishara, S. N. Long-term cognitive deficits in patients after surgery on aneurysms of the anterior communicating artery. J. Neurol. Neurosurg. Psychiatry 54, 909–914 (1991).
Richardson, J. T. E. Cognitive performance following rupture and repair of intracranial aneurysm. Acta Neurol. Scand. 83, 110–122 (1991).
Kreiter, K. T. et al. Predictors of cognitive dysfunction after subarachnoid hemorrhage. Stroke 33, 200–209 (2002).
Lee, J. H. et al. Hemodynamically significant cerebral vasospasm and outcome after head injury: a prospective study. J. Neurosurg. 87, 221–233 (1997).
Bartzokis, G. et al. Magnetic resonance imaging evidence of “silent” cerebrovascular toxicity in cocaine dependence. Biol. Psychiatry 45, 1203–1211 (1999).
Bode, H. & Wais, U. Age dependence of flow velocities in basal cerebral arteries. Arch. Dis. Child. 63, 606–611 (1988).
Alsdorf, W. H. et al. Severe and irreversible myelopathy after concurrent systemic and intrathecal nucleoside analogue treatment for refractory diffuse large B-cell lymphoma: a case report and review of the literature. J. Oncol. Pharm. Pract. 22, 523–527 (2016).
Hwang, T. L., Yung, W. K., Lee, Y. Y., Borit, A. & Fields, W. S. High dose ara-C related leukoencephalopathy. J. Neurooncol. 3, 335–339 (1986).
Slevin, M. L. et al. Effect of dose and schedule on pharmacokinetics of high-dose cytosine arabinoside in plasma and cerebrospinal fluid. J. Clin. Oncol. 1, 546–551 (1983).
Honkaniemi, J. et al. Reversible posterior leukoencephalopathy after combination chemotherapy. Neuroradiology 42, 895–899 (2000).
Ghali, M. G. Z., Davanzo, J., Leo, M. & Rizk, E. Posterior reversible encephalopathy syndrome in pediatric patients: pathophysiology, diagnosis, and management. Leuk. Lymphoma 60, 2365–2372 (2019).
Lindegaard, K. F., Nornes, H., Bakke, S. J., Sorteberg, W. & Nakstad, P. Cerebral vasospasm diagnosis by means of angiography and blood velocity measurements. Acta Neurochir. 100, 12–24 (1989).
Kirsch, J. D., Mathur, M., Johnson, M. H., Gowthaman, G. & Scoutt, L. M. Advances in transcranial doppler US: imaging ahead. Radiographics 33, E1–E14 (2013).
Tzeng, Y. C. et al. Cerebrovascular regulation during transient hypotension and hypertension in humans. Hypertension 56, 268–273 (2010).
Doering, T. J., Brix, J., Schneider, B. & Rimpler, M. Cerebral hemodynamics and cerebral metabolism during cold and warm stress. Am. J. Phys. Med. Rehabil. 75, 408–415 (1996).
Bisschops, L. L., van der Hoeven, J. G. & Hoedemaekers, C. W. Effects of prolonged mild hypothermia on cerebral blood flow after cardiac arrest. Crit. Care Med. 40, 2362–2367 (2012).
DeBaun, M. R. et al. Silent cerebral infarcts: a review on a prevalent and progressive cause of neurologic injury in sickle cell anemia. Blood 119, 4587–4596 (2012).
O’Brien, N., Maa, T. & Yeates, K. The epidemiology of vasospasm in children with moderate-to-severe traumatic brain injury. Crit. Care Med. 43, 674–685 (2015).
Croal, P. L. et al. Assessment of cerebral blood flow with magnetic resonance imaging in children with sickle cell disease: a quantitative comparison with transcranial doppler ultrasonography. Brain Behav. 7, e00811 (2017).
Acknowledgements
The authors would like to thank Bobby Ergin and Vladimir Ponomarev for their technical assistance. This study was funded by the Thrasher Research Fund.
Author information
Authors and Affiliations
Contributions
L.R.S. conceived of and designed the study. L.R.S., W.Z., P.B., and A.G.T. acquired the data. L.R.S., W.Z., P.B., S.C., R.F.G., and R.J.F. analyzed and interpreted the data. L.R.S. drafted the manuscript. L.R.S., W.Z., P.B., R.F.G., and R.J.F. critically revised the manuscript of important intellectual content. L.R.S., W.Z., P.B., A.G.T., S.C., R.F.G., and R.J.F. approved of the final version to be published.
Corresponding author
Ethics declarations
Competing interests
R.F.G. is an associate editor for Neurology; otherwise, we have no relevant conflicts of interest or disclosures to report.
Consent and approval
This study was approved by the institutional review board. All families signed informed consent, and all children 7 years of age or older gave verbal assent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sun, L.R., Ziai, W., Brown, P. et al. Intrathecal chemotherapy-associated cerebral vasospasm in children with hematologic malignancies. Pediatr Res 89, 858–862 (2021). https://doi.org/10.1038/s41390-020-1008-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-1008-1
This article is cited by
-
Neuromonitoring in Children with Cerebrovascular Disorders
Neurocritical Care (2023)
-
Cytarabine
Reactions Weekly (2021)