Abstract
Background
The prognostic significance of hyperlactatemia in young children with liver injury suspected to be attributed to repeated supratherapeutic doses of acetaminophen remain understudied.
Methods
We conducted a retrospective medical chart review including children aged <5 years admitted with hepatocellular injury. The study was conducted in Bardnesville Junction Hospital operated by Médecins Sans Frontières in Monrovia, Liberia.
Results
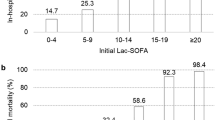
We analyzed 95 children with liver injury in whom a blood lactate measurement on admission was available. Eighty children (84%) were aged <2 years; 49 children (52%) died during hospitalization. The median acetaminophen concentration on admission was 20 mg/L with 60 (70%) children presenting concentrations exceeding 10 mg/L. Median lactate was significantly higher in children who died (10.7 mmol/L; interquartile range (IQR): 8.5–15.7) than those who survived (6.1 mmol/L; IQR: 4.1–8.5), P value < 0.001). The optimal threshold obtained was 7.2 mmol/L with a sensitivity of 84% and specificity 70% (area under curve = 0.80). The previously established thresholds of 3.5 and 4 mmol/L lactate had very low specificity identifying non-survival in children included in this study.
Conclusion
In this setting, young children with ALF possibly attributed to acetaminophen toxicity were unlikely to survive if the venous blood lactate concentration exceeded 7.2 mmol/L.
Similar content being viewed by others
Introduction
Pediatric acute liver failure (ALF) is a complex clinical syndrome that is the final common pathway for many disparate conditions. One of these conditions is acetaminophen-induced ALF.1 Although intended to determine whether patients should be referred or transferred to a liver transplantation center, prognostic evaluation using the modified King’s College Hospital criteria (KCC) may also be useful for patient’s care in the absence of transplant facilities. The performance of the original KCC2 was criticized owing to the imbalance between the sensitivity and specificity;3,4 hence, the criteria were modified. Currently, the modified KCC includes measurement of arterial lactate concentrations, with levels >3.5 mmol/L prior to fluid resuscitation associated with a high likelihood of death.5 Further modifications of the KCC took place, and the United Kingdom Registration criteria (UKRC) for super urgent liver transplantation included modified measurements and criteria including blood lactate >5 mmol/L on admission or >4 mmol/L 24 h after in the presence of liver injury.6 Notably, the UKRC outperformed the modified KCC in predicting hospital mortality.7 Other studies have proposed different threshold values,8 but the prognostic value of arterial lactate in predicting death in adults with acetaminophen-induced ALF is well accepted.5,9 In contrast, the prognostic value of venous lactate measurements in children with acetaminophen-induced ALF remains unclear.10 Since collection of blood can be challenging in children, using venous lactate concentrations, which is less invasive than arterial blood collection, could be an attractive alternative,11 particularly in settings where other measurements including measurement of blood gases and pH are not available.
Documented acetaminophen-induced hepatotoxicity among children is rare and, when reported, is mostly attributed to accidental or self-inflicted exposure in developed countries.12 From July to December 2015, Bardnesville Junction Hospital (BJH) in Monrovia, Liberia reported a case series of 77 children aged <5 years who had liver injury. Data were incomplete, but severe transaminase elevations, respiratory distress without hypoxemia, encephalopathy, deep hypoglycemia, and metabolic acidosis with increased anion gap were common findings. This constellation of findings continued to be reported throughout 2016 and 2017, with acetaminophen toxicity confirmed only in a minority of cases but suspected in others. Here we aimed to examine the prognostic value of venous blood lactate concentration on inpatient mortality among sample of children admitted with liver injury suspected to result from supratherapeutic acetaminophen overdose at BJH. We used venous lactate concentration as a more feasible alternative to arterial concentration.
Materials and methods
The study was approved by the Liberian National Research Ethical Board (ref NREB-003-16).
Study setting
In April 2015, Médecins Sans Frontières (MSF) opened a pediatric hospital within BJH in Monrovia, Liberia. The 82-bed facility serves as a referral hospital for complicated pediatric cases in the greater Monrovia area and has general pediatrics, intensive care, and inpatient nutritional activities. In 2016, among the 4500 admissions, the most common admitting diagnoses were malaria, severe malnutrition, dehydration induced by non-bloody diarrhea, and respiratory tract infections.
Study population
We performed a retrospective chart review of patients admitted between August 2016 and June 2017 with suspected hepatocellular injury. Identifying the etiology of liver injury was challenging, due to the scarcity of biochemical analyses and absence of on-site toxicological laboratories.
Hepatocellular injury was clinically suspected if a child presented any two of the following symptoms: hepatomegaly, hypoglycemia, respiratory distress without hypoxemia on pulse oximetry, and gastric bleeding. Upon clinical suspicion, hepatocellular injury was confirmed if the children presented with an alanine aminotransferase (ALT) activity more than three times the upper limit of normal (ULN), a total bilirubin concentration more than twice the ULN, or both.13 Severe liver injury was defined as aspartate transaminase (AST)/ALT >1000 IU/L.13 In case acetaminophen poisoning was suspected as the cause of liver injury, N-acetylcysteine was administered as per protocol at the discretion of the treating physician.
Data collection and definitions
All information was collected from the medical charts archived at BJH after patient discharge. Information extracted from the charts was recorded onto a standardized case report form, which was then entered into Research Electronic Data Capture (RedCap).
Admission data included patients’ age, sex, body weight, vital signs (heart rate, respiratory rate, capillary refill time, and axillary temperature), and respiratory and neurological status. The presence of hepatomegaly was systematically assessed. Children were screened for malnutrition using body weight, height (or length for children <2 years), mid-upper arm circumference (MUAC), and presence of edema upon arrival to the hospital. Severe acute malnutrition (SAM) was diagnosed in children presenting with edema, MUAC < 115 mm, or a weight-for-height z-score <−3.14
History of acetaminophen consumption was also assessed on admission in the preceding 7 days, though accuracy was often limited by caregivers’ inability to provide the names of medications administered at home, the doses given, and the timing of medication administration. If hepatocellular injury was suspected, laboratory analyses were performed on admission and included serum electrolytes, transaminase activities, total bilirubin concentration, creatine kinase activity, and venous blood lactate concentration. Serological tests for HIV and hepatitis A, B, C, and E were performed. Each child was also screened for malaria with the SD Bioline Malaria Ag P.f. (HRP2) rapid diagnostic test.
Specific blood draws for acetaminophen quantification from children with hepatocellular injury were not collected routinely, but residual frozen (−20 °C) plasma samples of selected patients were sent for toxicological analysis at ToxLab, Paris, France in March 2018. Vital signs and biochemical index variables were defined according to standard reference ranges.15,16,17,18 Cardiovascular dysfunction was defined as capillary refill time ≥3 s in the presence of tachycardia or bradycardia.19 Hepatocellular injury or ALF possibly due to acetaminophen ingestion was defined as a suspected hepatocellular injury in the presence of blood acetaminophen concentration >10 mg/L when first measured or a reported cumulative dose of acetaminophen of at least 150 mg/kg (or 75 mg/kg in 24 h).20,21 For this analysis, we used data based on ALT activity, total bilirubin concentration, and availability of blood lactate measurement upon suspicion of the liver injury.
Data analysis
The primary outcome was survival to hospital discharge. We excluded children who were admitted with findings suggestive of hepatocellular injury that upon further investigation was not confirmed. Children who did not have a venous blood lactate measurement documented were also excluded (Fig. 1). We described the frequencies, central values and distributions of clinical signs and symptoms, and biochemical and serological tests. Blood lactate medians were compared between children: (i) surviving to discharge and those who died during hospitalization, (ii) with and without malaria, (iii) severely acutely malnourished and normal nutritional status, and (iv) with and without cardiovascular dysfunction. Differences in medians were tested using Kruskal–Wallis for variables with more than two categories and Mann–Whitney for the ones with two categories.
Associations between lactate concentrations and death were calculated and adjusted for potential confounders using incidence risk ratios (IRR), P values, and 95% confidence intervals (CIs) derived from Poisson regression analysis with robust error variance. We adjusted for age, sex, cardiovascular dysfunction, SAM, and diagnosis of malaria. Time at risk was defined in hours as the time between admission and death or discharge. Only time spent in BJH was included in the analysis. Two-sided tests were considered statistically significant if P value was <0.05. The sensitivity and specificity of venous blood lactate to predict mortality were studied simultaneously for any possible threshold values. The receiver operating characteristic curve was traced for these cut-offs and its area under curve (AUC) was calculated. A sensitivity analysis was conducted including the children who had hepatocellular injury possibly due to acetaminophen ingestion. All analyses were performed using Stata© 13.1 (College Station, TX).
Results
Data from 95 children admitted between August 2016 and June 2017 were analyzed (Fig. 1). The average age at admission was 14.7 months and 49 (52%) were males. Forty-nine (52%) children eventually died during hospitalization (Table 1). The average length of hospital stay was 6 days (range: <24 h, 21 days). The total observation time was 618 person-days. All children were <20 kg and 81 (85%) were <10 kg. At admission, hepatomegaly was the most prevalent symptom followed by lethargy and coma and respiratory distress without hypoxemia (Table 1). AST activity exceeded 1000 IU/L in 85 (90%) children, and ALT exceeded 1000 IU/L in 70 (74%). Hypoglycemia was present in 72 (78%) children. Median venous lactate concentration was 8.5 mmol/L, interquartile range (IQR) 5.4–13.1, and 60/86 children with measurements (70%) had a plasma acetaminophen concentration >10 mg/L.
Among all children, 70/95 (74%) reported acetaminophen consumption. Caregivers of 59 children were able to quantify the dose given prior to hospitalization. Of these, the mean reported dose was 88 mg/kg/day (range 10–625) and the median was 66 mg/kg/day [IQR 50–100], with 23/59 (39%) reporting supratherapeutic doses prior to hospitalization. When considering both the plasma acetaminophen concentration and doses reported by caregivers, hepatocellular injury possibly due to acetaminophen ingestion was present in 67/95 children (44 by concentration, 7 by history, 16 by both). The clinical profile presented by these children was similar (Table S1).
Among the serological tests performed, no child had hepatitis B (n = 93) or Hepatitis C (n = 92). One child had hepatitis A (n = 64) and one child had hepatitis E (n = 72). The child with hepatitis A had a history of acetaminophen consumption; however, his blood plasma was measured on the third day of hospitalization resulting in a non-detectable level. The child presenting with hepatitis E had a plasma acetaminophen level of 61.5 mg/dL ascertaining toxic levels.
Venous lactate concentrations were higher in patients who died (10.7 mmol/L, IQR 8.5–15.7) than those who survived (6.0 mmol/L, IQR 4.1–8.5; P value < 0.001) but were not different among children presenting with either malaria, SAM, or cardiovascular dysfunction in comparison with those without (Table 2). There was no difference in proportions of SAM, cardiovascular dysfunction, and malaria among the patients who met the acetaminophen intoxication criteria (Table S2). Moreover, the risk of death increased by 15% with every increase of 1 mmol/L in blood lactate concentration (95% CI 1.11–1.20, P value < 0.001) among all the children included (Table 3, Model II). Similarly, this risk increased by 16% (95% CI 1.09–1.23) among the children who met the intoxication criteria (Table S3).
Receiver operating characteristic analysis identified an early venous blood lactate concentration of 7.2 mmol/L as the optimal threshold to discriminate risk of mortality among children presenting with hepatocellular injury (AUC = 0.80, Fig. 2a). The AUC was similar for the same threshold value when only considering children with hepatocellular injury possibly due to acetaminophen ingestion (AUC = 0.79, Fig. 2b). In total, 41/55 children (75%) who had lactate concentration >7.2 mmol/L measured early after admission died in comparison to 14/46 children (25%) who did not (Pearson’s chi-squared P value < 0.001). The threshold value of 7.2 mmol/L venous lactate concentration had a sensitivity of 84% and specificity of 70% when considering all children with suspected hepatocellular injury (Fig. 2c) and a sensitivity of 92% and specificity 61% in the subset of patients who had hepatocellular injury possibly due to acetaminophen ingestion (Fig. 2d).
Discussion
We investigated the prognostic implications of venous blood lactate concentrations among children aged <5 years presenting with hepatocellular injury and meeting the case definition for suspicion of acetaminophen poisoning in an urban referral hospital in Monrovia, Liberia. More than two-third of the patients met the criteria for hepatocellular injury due to acetaminophen ingestion.
Previous studies have examined the prognostic value of arterial lactate in hepatocellular injury among adults but with these values remaining unclear for children.5,9 The arterial lactate thresholds identified for adults did not perform well for predicting death when applied to pediatric venous blood samples (Table S4).5,8 Such comparison might be unfeasible due to the contextual differences in addition to the medium of blood used for lactate measurement (venous versus arterial). The optimal threshold of 7.2 mmol/L for venous lactate identified here was a predictor of mortality among all children with hepatocellular injury as well as the group who had hepatocellular injury due to suspected acetaminophen ingestion. The venous lactate values as high as those seen in this pediatric population are associated with severe illness thereby complicating its use as a clinical tool. Nevertheless, the lactate threshold of 7.2 reported here is higher than those reported for other diseases causing lactic acidosis among children in similar contexts including, sepsis (>3 mmol/L),22 shock (>5 mmol/L),23 and malaria (>5 mmol/L).24,25 In a setting where the modified KCC, UKRC, and the Pediatric Sequential Organ Failure Assessment score could not be used because of lack of laboratory capacity, relying on venous lactate alone was a predictor of death, but further investigation is needed.26
Children in the present study showed markedly elevated transaminase activity, suggestive of extensive hepatocellular injury, but only 67/95 met our criteria of hepatocellular injury possibly due to acetaminophen overdose. This is partially due to incomplete and/or unreliable information: plasma acetaminophen levels were only available on a subset of patients, and caregiver reporting may have been unreliable. Although we are unable to attribute acetaminophen ingestion as the cause of the presentation in this case series, it is possible that it was at least a partial cause in many cases.
Indeed, diagnosing chronic acetaminophen poisoning is extremely difficult and requires various tests, which were mostly unavailable in Monrovia nor are they available in similar low-resource settings. In Monrovia and at BJH, diagnosing acetaminophen poisoning started recently when a biochemistry minilab was made available despite the absence of other important laboratory indicators. For instance, toxicology laboratories quantifying acetaminophen are unavailable in Monrovia, making real-time diagnosis impossible. Consequently, in the absence of important laboratory measurements, underdiagnoses remain a possibility not just in Monrovia rather in all contexts where this phenomenon might be taking place. In this study, we unveiled acetaminophen poisoning in children in Monrovia; however, that might not be specific to Liberia only but rather to all countries with unrestricted access to medication especially the ones with prevalent risk factors, for instance SAM. Understanding the prognostic factors is of importance in hospital contexts despite the limited treatment options. Therefore, preventative public health interventions remain the hallmark response in tackling this problem in this context.
This analysis has several key limitations. First, lactate values were recorded upon suspicion, which may have led to higher values, rather than on admission with liver injury. This may have compounded difficulties in obtaining reported acetaminophen consumption from caregivers as well as timely collection of blood samples (and their interpretation) for acetaminophen concentration. Second, the unavailability of some diagnostic tools and laboratory tests made differential diagnosis of hepatocellular injury etiology challenging. As such, we were not able to include several other components of validated predictive scales (such as arterial pH and blood coagulation tests) in our predictive models. It is possible that, with the addition of these other data, our models may have performed differently. Nonetheless, the simplicity of using venous blood lactate alone for predicting death on admission may be useful to classify patients in prognostic categories in resource-limited settings thereby facilitating clinical care. An obvious limitation of these results is that, in a setting like BJH in Monrovia, there are few, if any, therapeutic options for children who have been identified as being at high risk for in-hospital mortality. Finally, the data presented here is hypothesis generating and a specific study aiming to establish a lactate threshold criteria for use in low-resource settings would be needed.
Conclusion
Venous lactate measurement is a value alternative to arterial lactate measurement in resource-limited settings. In the present study, venous lactate value of >7.2 mmol/L identified children at risk of in-hospital mortality, but to examine additional uses of blood lactate thresholds for prognostic classification for suspected acetaminophen overdose in low-resource settings, additional research is needed.
References
Bernal, W., Auzinger, G., Dhawan, A. & Wendon, J. Acute liver failure. Lancet 376, 190–201 (2010).
O’Grady, J. G., Alexander, G. J. M., Hayllar, K. M. & Williams, R. Early indicators of prognosis in fulminant hepatic failure. Gastroenterology 97, 439–445 (1989).
Anand, A. C., Nightingale, P. & Neuberger, J. M. Early indicators of prognosis in fulmitant hepatic failure: an assessment of the King’s criteria. J. Hepatol. 26, 62–68 (1997).
Bernal, W., Wendon, J., Rela, M., Heaton, N. & Williams, R. Use and outcome of liver transplantation in acetaminophen‐induced acute liver failure. Hepatology 27, 1050–1055 (1998).
Bernal, W., Donaldson, N., Wyncoll, D. & Wendon, J. Blood lactate as an early predictor of outcome in paracetamol-induced acute liver failure: a cohort study. Lancet 359, 558–563 (2002).
Donnelly, M. C., Hayes, P. C. & Simpson, K. J. The changing face of liver transplantation for acute liver failure: assessment of current status and implications for future practice. Liver Transpl. 22, 527–535 (2016).
Porteous, J. et al. Outcome of acetaminophen‐induced acute liver failure managed without intracranial pressure monitoring or transplantation. Liver Transpl. 25, 35–44 (2019).
Schmidt, L. E. & Larsen, F. S. Prognostic implications of hyperlactatemia, multiple organ failure, and systemic inflammatory response syndrome in patients with acetaminophen-induced acute liver failure. Crit. Care Med. 34, 337–343 (2006).
McPhail, M. J. W., Wendon, J. A. & Bernal, W. Meta-analysis of performance of Kings’s College Hospital Criteria in prediction of outcome in non-paracetamol-induced acute liver failure. J. Hepatol. 53, 492–499 (2010).
Hadem, J. et al. Prognostic implications of lactate, bilirubin, and etiology in German patients with acute liver failure. Clin. Gastroenterol. Hepatol. 6, 339–345 (2008).
Mikami, A. et al. Can we predict arterial lactate from venous lactate in the ED? Am. J. Emerg. Med. 31, 1118–1120 (2013).
Squires, R. H. et al. Acute liver failure in children: the first 348 patients in the pediatric acute liver failure study group. J. Pediatr. 148, 652–658 (2006).
US Food and Drug Adminstration. Guidance for industry drug-induced liver injury: premarketing clinical evaluation. https://www.fda.gov/downloads/Guidances/UCM174090.pdf (2009).
Tickell, K. D. & Denno, D. M. Inpatient management of children with severe acute malnutrition: a review of WHO guidelines. Bull. World Health Organ. 94, 642 (2016).
Lee, M. Basic Skills in Interpreting Laboratory Data (American Society of Health-System Pharmacists, 2009).
Kaplan, M. M. in Diseases of the Liver (eds Schiff, L. & Schiff, E. R.) 108–144 (Lippincott, Philadelphia, PA, 1993).
Glasper, E. A., McEwing, G. & Richardson, J. Oxford Handbook of Children’s and Young People’s Nursing (Oxford University Press, 2015).
Advanced Life Support Group. Pre-hospital Paediatric Life Support: A Practical Approach to the Out-of-hospital Emergency Care of Children (Blackwell Publishing, 2005).
Jones, K. D. J. & Berkley, J. A. Severe acute malnutrition and infection. Paediatr. Int. Child Health 34, S1–S29 (2014).
Heard, K. et al. Toxicity from repeated doses of acetaminophen in children: assessment of causality and dose in reported cases. Am. J. Ther. 21, 174 (2014).
Kozer, E., Greenberg, R., Zimmerman, D. R. & Berkovitch, M. Repeated supratherapeutic doses of paracetamol in children—a literature review and suggested clinical approach. Acta Paediatr. 95, 1165–1171 (2006).
Duke, T. D., Butt, W. & South, M. Predictors of mortality and multiple organ failure in children with sepsis. Intensive Care Med. 23, 684–692 (1997).
Hatherill, M., Waggie, Z., Purves, L., Reynolds, L. & Argent, A. Mortality and the nature of metabolic acidosis in children with shock. Intensive Care Med. 29, 286–291 (2003).
Karnad, D. R., Nor, M. B. M., Richards, G. A., Baker, T. & Amin, P. Intensive care in severe malaria: report from the task force on tropical diseases by the World Federation of Societies of Intensive and Critical Care Medicine. J. Crit. Care 43, 356–360 (2018).
Herdman, M. T. et al. The role of previously unmeasured organic acids in the pathogenesis of severe malaria. Crit. Care 19, 317 (2015).
Matics, T. J. & Sanchez-Pinto, L. N. Adaptation and validation of a Pediatric Sequential Organ Failure Assessment Score and evaluation of the sepsis-3 definitions in critically ill children. JAMA Pediatr. 171, e172352 (2017).
Acknowledgements
We are indebted to the BJH staff in Liberia for assisting in conducting the study. The authors thank Professor Robin E Ferner for his thoughtful comments and suggestions on earlier drafts of this article. The study was funded by Médecins Sans Frontières − Operational Centre Paris. Epicentre receives core funding from Médecins Sans Frontieres (MSF). The study was performed in the pediatric hospital operated by MSF. Staff members of MSF contributed to designing the study, collecting and analyzing the data, and in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
M.K.H. led the epidemiological and statistical analysis, drafted the manuscript, and contributed to interpretation of the results. K.P. and F.J.B. contributed toward designing the study and the data collection instruments. N.M., S.M., and T.R. contributed substantially toward data analysis and interpretation of the results. L.B. and J.K. contributed to the conception and result interpretation. All authors reviewed, contributed to, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Haidar, M.K., Morton, N., Roederer, T. et al. Evaluating lactate prognostic value in children suspected of acetaminophen-induced liver failure in Liberia. Pediatr Res 88, 605–611 (2020). https://doi.org/10.1038/s41390-020-0783-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0783-z