Abstract
Background
Though prenatal antidepressant exposure has been associated with adverse developmental outcomes, the extent to which the effects are due to prenatal drug exposure or underlying maternal mood disturbances is unclear.
Methods
This was a population-based retrospective cohort study using administrative data from British Columbia, Canada (n = 94,712). Analyses were designed to remove confounding effects of prenatal antidepressant exposure from maternal mood. First, children prenatally exposed to antidepressants were matched to unexposed children using high-dimensional propensity scores (HDPS). Second, children whose mothers had used antidepressants throughout pregnancy were compared against those whose mothers discontinued treatment.
Results
In all, 3.87% (n = 3661) of children in the overall study population were prenatally exposed to antidepressants. In both analyses, we report increased odds for lower levels of physical independence (HDPS: OR, 1.14; 95% CI, 1.00–1.30; continuers/discontinuers: OR, 1.14; 95% CI, 0.99–1.32), and higher levels of anxious behaviors (HDPS: OR, 1.30; 95% CI, 1.01–1.66; continuers/discontinuers: OR, 1.32; 95% CI, 1.01–1.72) associated with antidepressant use in pregnancy. All other relationships were not significant using these methods.
Conclusions
Prenatal antidepressant exposure was selectively associated with worse anxious behaviors and physical independence at kindergarten age, with no effects on other developmental domains. Effects are also likely attributable to maternal mental illness severity or other unmeasured confounding factors.
Impact
-
Selective associations between prenatal antidepressant exposure and children’s anxiety and physical independence at kindergarten were identified, with no impact on other developmental domains.
-
Contradictory reports have emerged regarding the association of adverse child outcomes with prenatal antidepressant exposure. These inconsistencies may be due to differences in control for confounding.
-
Effects of prenatal antidepressant exposure on anxious behaviors and physical independence are likely also attributable to severity of underlying maternal mood disorders, highlighting the importance of maternal mental health for developmental health.
Similar content being viewed by others
Introduction
Depression during pregnancy affects up to 17% of women,1 making it among the top complications of pregnancy. Almost a third of treatment-seeking women are prescribed antidepressants, the most commonly used class of which is selective serotonin reuptake inhibitors (SSRIs).2,3 The decision to pursue or continue pharmacotherapy for depression during pregnancy raises challenging questions for women and their clinicians due to the need to balance maternal mental health needs with concerns of adverse fetal and developmental effects. While discontinuing antidepressant treatment may increase the risk of relapsing depression during pregnancy,4,5 which in turn, carries risk for maternal and fetal health,6 there are legitimate concerns that taking antidepressants during pregnancy may adversely impact child development. Elucidating the effects of prenatal antidepressant exposure on development, in order to better understand potential risks to the developing child and help guide treatment decisions, thus remains an important research objective.
Antidepressants readily cross the placenta and the fetal blood–brain barrier, and thus, it is plausible that early shifts in monoamine transmitters during developmentally sensitive periods could influence early brain development.7 Yet, reports of long-term effects following such exposure have been inconsistent and contradictory. Studies have reported higher risk for outcomes, including autism spectrum disorder;8 attentional disorders;9 and altered motor, emotional, and language development in children;10,11,12,13,14 while recent findings suggest that a broader range of neurodevelopmental outcomes encompassing overall risk of psychiatric disorders may be affected.15 However, central to understanding the impact of prenatal antidepressant exposure is the need to disentangle the effects of antidepressant exposure from those of the underlying maternal mental illness (“confounding by indication”).7
Confounding by indication is a critical methodological conundrum when addressing questions of fetal pharmacoepidemiology. Untreated, maternal depression in and of itself is an independent risk factor associated with poorer developmental outcomes, including low birth weight, preterm birth, and socio-emotional disorders later in childhood.7,16 Moreover, the treatment pregnant women receive for their depression is also affected by important contextual factors, such as socio-economic status,17 which influence child development.18 Addressing these sources of confounding is vitally important to isolate the unique impact of prenatal antidepressant exposure, yet challenging to do.
The availability of large administrative datasets presents an opportunity in this regard. While there are inherent limitations to using secondarily collected data from health system interactions for the purposes of research, there are also a number of advantages. Especially in a single-payor health system with universal coverage, administrative data allow for population-wide and near-complete data capture of interactions across the spectrum of covered healthcare services. Accordingly, it is possible to gain comprehensive insights into population-level and individual health status. Recent studies have taken advantage of these opportunities and applied methods to administrative data aimed at adjusting for both known and unknown factors related to indication for prenatal antidepressant medication. These studies have found attenuated associations with a range of developmental outcomes compared to previous research, suggesting that the overall mixed state of findings in the literature may reflect differences in control of confounding across studies.19,20,21,22
To what extent child development is affected by prenatal antidepressant exposure, and whether this effect can be distinguished from the impact of prenatal maternal mood disturbances, remain pressing research questions. The present study was undertaken to investigate a broad spectrum of outcomes reflective of typical child development. Using complementary but different analytic approaches with population-level administrative data, this study investigated associations between prenatal antidepressant exposure and multiple domains of child development at kindergarten age, while adjusting for maternal factors associated with antidepressant use in pregnancy.
Methods
Study design and data sources
This was a retrospective cohort study using administrative data from British Columbia, Canada. Canada has universal healthcare coverage and British Columbia collects information from all fee-for-service physician visits (in the Medical Services Plan (MSP) data), hospitalizations (in the Discharge Abstract Database), and prescription drug dispensations (through BC PharmaNet) for registered residents, allowing linkage of individual-level data. Mothers and their offspring were identified through the Perinatal Data Registry that includes 99% of births province-wide. Child development outcomes were available through the Human Early Learning Partnership. Data across all sources were linked at Population Data BC using unique individual-level identifiers. This study received ethics approval from all Data Stewards and the University of British Columbia Children’s and Women’s Research Ethics Board. All inferences, opinions, and conclusions drawn are those of the authors and do not reflect the opinions or policies of the Data Stewards.
Study cohort
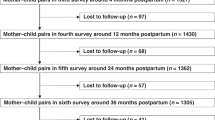
The sampling frame for this study represents children with completed records of child development collected between 2003 and 2013. We included singleton children born in-province to mothers registered in the province for at least 275 days during the year of birth and year prior to birth; this was to ensure that women included in the study were residing in the province during this duration and would have reliable data records. Only maternal–child dyads with complete data on covariates and outcomes were included (n = 94,712; Fig. 1).
Exposure classification
Antidepressant drugs were identified using the Anatomical Therapeutic Chemical (ATC) Classification System codes; antidepressants belonging to different drug classes were included (see eTable 2 in Supplementary for list and categorization of antidepressant drugs by their corresponding ATC codes). Pregnancy trimesters were defined as outlined in eTable 2 in Supplementary. Prenatal antidepressant exposure was defined as either two or more dispensations for antidepressants throughout pregnancy or at least one dispensation from the second trimester of pregnancy until delivery. Though antidepressants are generally prescribed for extended durations, we were concerned that including only single dispensations would include pregnancies where exposure ceased shortly after conception due to concerns of adverse fetal effects, whereas single dispensations occurring during the second trimester onward were included as they were likely filled with knowledge of pregnancy status.
Outcome measures
Child development outcomes were assessed with the Early Development Instrument (EDI). The EDI is a validated teacher-report measure of children’s school readiness used in Canada and Australia.23 The EDI has been administered in British Columbia every 1–3 years since the 1999/2000 academic year. School and teacher participation in the EDI is voluntary and child participation occurs through passive parental consent; if parents choose to withdraw their consent, their child will not be rated. The EDI collection captures the majority of the kindergarten population (92% of the kindergarten population from all public-school districts), and approximately 88% of children in British Columbia are enrolled in public schools for kindergarten.
The EDI measures 16 subscales of early childhood development that fall into five distinct domains: physical health and well-being (which are comprised of subscales measuring gross and fine motor skills, physical independence, and physical readiness for the school day), emotional maturity (with subscales for aggressive, anxious and fearful, hyperactive and inattentive, and prosocial and helping behaviors), social competence (with subscales for overall social competence, approaches to learning, readiness to explore new things, and respect and responsibility), language and cognitive development (with the subscales of basic literacy, advanced literacy, basic numeracy, and interest in literacy, numeracy, and memory), and communication skills and general knowledge (no subscales). Its psychometric properties and validity have been well studied, and EDI scores have been associated with concurrent and later measures of developmental outcomes.24,25,26 Children were classified as developmentally “vulnerable” if their scores fell below previously defined thresholds designed to capture meaningful differences in developmental status;27 a binary outcome measure was preferable as the distribution of responses is skewed and not readily amenable to transformation. The subscale measuring prosocial and helping behaviors was not used as it had >5% missing responses.
High-dimensional propensity score (HDPS)
We generated HDPSs28 in order to match exposed and unexposed comparison populations, as they can help capture both known and unknown sources of confounding. HDPS takes unknown sources of confounding into account through a data-driven approach: by using large administrative datasets that have thousands of different data fields, or dimensions, this method generates empirical proxies of factors that differentiate the comparison populations of interest.28 The following sources of high-dimensional data, captured in the 365 days prior to conception, were used to determine the empirical covariates to be included in the HDPS: (1) Outpatient diagnoses and fee codes, which were captured in the MSP data. These data include MSP fee codes and up to five diagnoses based on the International Classification of Diseases Clinical Modification, Ninth Revision (ICD-9-CM) for each physician visit. (2) Inpatient diagnoses and procedures, which were captured in the Discharge Abstract Database. These data include up to 12 Canadian Classification of Intervention codes and up to 25 diagnoses from the International Classification of Diseases Clinical Modification, Ninth and Tenth Revisions, (ICD-9/10 codes) for each inpatient hospital admission in the province. (3) Drug dispensations from the BC PharmaNet, which includes details on the exact medicine dispensed for all medicines dispensed through community pharmacies in BC. The HDPS relies on the principle that through measuring many surrogate variables (e.g., procedure codes, fees, diagnoses) they are more likely, in combination, to act as a good proxy for relevant unmeasured confounding. The top 500 variables included in the HDPS are listed in eTable 3 in the Supplementary. In addition to these data-driven covariates, we also included child age at EDI, child sex, gestational age, child English as a second language status, EDI wave, maternal age at birth, parity, neighborhood income quintile, health service delivery area, diagnosis of a mood or anxiety disorder during pregnancy, and use of other psychotropic or antiepileptic medications during pregnancy for HDPS estimation. The HDPS was used for 1:4 (maximum) nearest-neighbor matching (without replacement) of exposed children to those whose mothers did not take any antidepressants during pregnancy, within a caliper of 0.2 standard deviations, per recommendations.29
Main analyses
Demographic characteristics between exposure groups were compared using standardized differences, which consider differences between groups in terms of their standard deviations and thus provide meaningful assessments of differences for large sample sizes across different types of variables.30 First, to provide a baseline comparison for inferential analyses, odds ratios (ORs) and 95% confidence intervals (CIs) in the overall cohort were estimated using multivariable logistic regressions. Included covariates in these analyses were child age at EDI assessment, child sex, gestational age, child English as a Second Language status, year of EDI assessment, maternal age at birth, neighborhood income quintile, health service delivery area, a mood or anxiety disorder diagnosis during pregnancy, and use of other psychotropic or antiepileptic medications during pregnancy. Second, in the HDPS-matched cohort, conditional logistic regressions were conducted to estimate ORs and 95% CIs. These analyses adjusted for other psychotropic or antiepileptic medications taken during pregnancy given that a standardized difference of 0.10, which is considered a meaningful difference,30 remained after matching (Table 1). Third, analyses were conducted in a subsample of women with an existing indication for antidepressants, determined based on dispensations that occurred in the 90–365 days prior to conception. Within this subsample, we compared the developmental outcomes of children whose mothers continued antidepressant treatment during pregnancy, against those whose mothers discontinued treatment, adjusting for the previous full list of covariates. The definition of comparison groups from the overall study cohort is illustrated in Fig. 1.
Sensitivity analyses
Two sensitivity analyses were performed. To address whether effects may have been influenced by misclassification of exposure, exposure was restricted as having had to include dispensations occurring in the second and third trimesters of pregnancy (i.e., eliminating exposures that occurred only in the first trimester). Second, to determine whether effects differed based on drug class, associations were estimated based on exposure to SSRIs only, non-SSRIs only, or both. All data management and statistical analyses were conducted using SAS 9.4.31
Results
Demographic characteristics of study cohorts
The study population sample included a total of 94,712 children born to unique mothers (Fig. 1). Of the overall sample, 3661 children (3.87%) were exposed to antidepressants during pregnancy. Children were 48.7% female (n = 46,086), with a mean gestational age of 38.9 weeks, and a mean age of 5.65 years at the time of EDI completion. Mothers were a mean age of 30.5 years at birth and 55.3% (n = 52,387) were multiparous.
Demographic characteristics of unexposed compared to exposed individuals for the overall and HDPS-matched cohorts are presented in Table 1. A higher proportion of mothers who took antidepressants during pregnancy were multiparous (62.1 vs 55.0%). Exposed children had a lower mean gestational age (38.4 vs 38.9 weeks) and fewer had ESL status (7.3 vs 21.7%) relative to unexposed children. There were significant differences between exposed and unexposed mothers in diagnoses of mood and anxiety disorders (64.2 vs 8.9%) and other psychotropic or antiepileptic medications taken during pregnancy (22.5 vs 3.5%).
After matching based on the HDPS, demographic characteristics became more similar between exposed and unexposed groups; differences were no longer meaningful with the exception of having taken other psychotropic or antiepileptic medications during pregnancy (17.5 vs 15.8%; Table 1). Because the matching strategy restricted to a certain width of the HDPS, not all exposed children were successfully matched. Demographic characteristics of unmatched and matched exposed mother–child dyads and of antidepressant continuation and discontinuation groups can be found in eTables 4 and 5 in Supplementary.
Results from main analyses
Results from the main analyses are presented in Table 2, illustrating the odds of being assessed as vulnerable on each developmental scale associated with prenatal antidepressant exposure. Prior to HDPS matching, children with prenatal antidepressant exposure were significantly more likely to be assessed as vulnerable on most developmental scales. These results were significantly attenuated in analyses that incorporated better control of confounding.
In the HDPS-matched cohort, prenatal antidepressant exposure was associated with developmental vulnerability in physical independence (OR, 1.14; 95% CI, 1.00–1.30), social exploration (OR, 1.64; 95% CI, 1.23–2.20), and anxious behaviors (OR, 1.30; 95% CI, 1.01–1.66). Comparing development in children of mothers who continued antidepressant treatment during pregnancy relative to those who discontinued, only the association with anxious behaviors was significant (OR, 1.32; 95% CI, 1.01–1.72) though the association with physical independence was nearly significant (OR, 1.14; 95% CI, 0.99–1.32) (Table 2).
Sensitivity analyses
Results from analyses that excluded children with prenatal antidepressant exposure occurring only in the first trimester of pregnancy were consistent with the analyses that considered exposure throughout pregnancy, with slightly elevated effect sizes (Table 3). Notably, the association of prenatal antidepressant exposure with vulnerability in physical independence was statistically significant among children whose mothers continued antidepressants during pregnancy compared with those whose mothers discontinued antidepressants (OR, 1.19; 95% CI, 1.03–1.38).
In drug class-specific analyses, directions of effect were consistent with those found in overall analyses, though statistical precision was reduced. Focusing on associations with physical independence, anxious behaviors, and social exploration, there were elevated point estimates with exposure to non-SSRIs and both SSRI and non-SSRI exposure, compared to SSRIs only, though results were not robust across analyses and CIs were wide (eTables 6 and 7 in Supplementary).
Discussion
In this population-based study examining child development outcomes at kindergarten age, we investigated the impact of prenatal antidepressant exposure on a diverse range of behavioral and developmental outcomes, reflecting the overall health of typically developing children. Prenatal antidepressant exposure was associated with small but significant increases in the odds of being assessed as vulnerable in anxious behaviors and physical independence, even after controlling for confounding by underlying maternal mental health. In particular, these associations remained significant following the use of HDPS matching to proxy for relevant unmeasured confounding and the comparisons between antidepressant continuers vs discontinuers also showed a significantly increased risk for anxious behaviors. Associations with the other domains of child development that were investigated were not statistically significant.
Comparison with previous findings
Associations between prenatal antidepressant exposure and anxious behaviors have been previously investigated using various study designs.7 In a prospective cohort study, prenatal antidepressant exposure was associated with higher risk for anxious behaviors at 3 years of age, after adjusting for maternal depression symptoms during pregnancy and after birth, an effect that was sustained when children were 6 years old.32 Similarly, using a discordant-exposure sibling-based study design to control for familial factors, a population-based study reported that prenatal antidepressant exposure was only associated with anxious symptoms at 36 months.33
The association between antidepressant exposure and physical independence, but not motor skills, is inconsistent with previous studies reporting associations between prenatal antidepressant exposure and poorer motor development.10,34,35 This apparent discrepancy may be related to how outcomes were assessed across different studies. It is important to note that, as the EDI is a behavioral assessment, questions related to physical independence capture information beyond the realm of motor skills alone (i.e., “is independent in washroom activities”). It is thus possible that the significant association using the EDI physical independence measure may be driven by yet unaccounted environmental influences that could be related to antidepressant use during pregnancy or maternal mental health. Conversely, it is also possible that any effects of prenatal antidepressant exposure on motor skills are highly differentiated and require assessments beyond the EDI.
The insignificant associations with other developmental outcomes, such as language, cognitive, and communication skills, even where stringent approaches were used to control for confounding suggests that observed associations in the overall cohort may be due to confounding by indication or other unmeasured environmental differences. A similar attenuation of differences has been reported after controling for confounding in studies investigating associations with intellectual disability36 and attention-deficit/hyperactivity disorder.9 The critical need to account for the impact of poor maternal mental health and associated factors that also shape developmental risk has been further highlighted in a recent systematic review illustrating that many developmental outcomes may be driven by factors related to the underlying mood disorder itself, thereby reflecting an impact of maternal illness severity and not SSRI exposure per se.37
Preclinical models present biologically plausible rationales for the effects observed in this study. Antidepressants typically act via manipulations of central levels of key neurotransmitters including serotonin. Serotonin plays a number of different roles during embryogenesis in motor and central nervous system development. Developmental changes in serotonin may later act to influence maturation and function of the serotonin system, explaining why increased intrasynaptic serotonin associated with antidepressant exposure may predispose to affective disorders later in life.7,38,39
Strengths and limitations
This study is strengthened by its population-based nature that included detailed developmental data from the EDI, and the relatively objective nature of teacher-reported behaviors that avoids potential biases inherent to parental or clinical report. Further, investigating developmental subscales allowed for exploration of potential impacts on a comprehensive suite of normative child development outcomes and allows generalizability of findings to general pediatric populations. Our study is also strengthened by the methodology employed to attempt to better control for potential unobserved confounding by other related yet unmeasured factors through the use of HDPS matching. However, despite these efforts, a meaningful difference in use of other psychotropic or antiepileptic medications during pregnancy between the exposed and unexposed groups persisted. A continuer/discontinuer analysis was also conducted to attempt to distinguish a drug effect from a disease effect, as finding no difference between those who discontinued their antidepressant 90 days before conception would suggest an enduring disease effect. We found that risk for anxious behaviors remained elevated in children of mothers who continued treatment throughout pregnancy but cannot rule out that this effect may be due to women who continued treatment having more severe mental illness than those who discontinued. It is likely that the decision to continue antidepressant treatment during pregnancy is related to illness severity necessitating ongoing treatment or remittance of symptoms coinciding with pregnancy.
Across both the HDPS-matched and the discontinuer/continuer analyses, differences between exposure groups reflect an incongruity in maternal illness severity between groups. Despite attempts to control for confounding, we coud not rule out that differences in maternal illness severity underlie the increased risk for anxious behaviors and physical independence. We were unable to control for differences related to factors that were not represented in available data sources, such as education levels, ethnicity, or immigrant status. Moreover, it is not clear how accurately diagnoses captured in administrative datasets reflect differences in the range of psychiatric symptoms or their impact on everyday maternal/family life. We were also unable to address the role of genetic confounding. It is conceivable that prenatal antidepressant exposure may reflect a genetic propensity inherent to a mother’s depression during pregnancy, which itself confers a risk for affective disorders in her child. In this sense, prenatal antidepressant exposure would represent a proxy measure of a yet unidentified genetic risk.
An inherent limitation of studies that rely on administrative data is misclassification of antidepressant exposure, as dispensations may not reflect whether women took their medications, and as such, we used a relatively strict definition of antidepressant exposure. Results from sensitivity analyses that restricted exposure as having to occur in later stages of pregnancy showed increased effect sizes without compromising statistical precision, supporting the use of a stricter definition of exposure. Nonetheless, there are limitations to this approach as filling a prescription later in pregnancy can indicate greater severity of maternal depression, and the timing of exposure occurs during a sensitive period of fetal development.
The results of this study may not be generalizable to all women and children exposed to antidepressants during pregnancy. We applied strict criteria for inclusion in the study cohort by requiring registration in the healthcare system and complete data; however, this likely resulted in excluding maternal–child pairs at the tail ends of the socio-economic distribution who are at higher risk of adverse mental health and developmental outcomes.40 Within the study population, we intentionally chose to restrict our analyses to exposed individuals who could be compared to an appropriate population in the HDPS analysis, thereby excluding women with the most severe depression as they could not be matched. Conversely, the continuer/discontinuer analysis compared women with less severe mental illness to those with more severe illness. Finally, a limitation of using the EDI is that we may have missed associations with child behaviors or symptoms whose onset only occur later in childhood. Applying the results of this study to other populations who differ in terms of baseline demographic and disease characteristics should be done with caution.
Conclusions
To conclude, we report that prenatal antidepressant exposure was selectively associated with more anxious behaviors and poorer physical independence in children at kindergarten age, and not with other domains of child development. While it is possible that these findings reflect effects associated with prenatal antidepressant exposure, we cannot rule out the impact of maternal illness severity and related genetic risk. Our findings concur with a large body of literature highlighting the importance of overall maternal mental health for the long-term health and well-being of mothers and their children. While our findings might point to a development impact of prenatal antidepressant exposure, this association cannot be unambiguously distinguished from exposure to poor maternal mental health during pregnancy and once again highlight the importance of treatment that optimizes maternal mental health and child well-being.
References
Underwood, L., Waldie, K., D’Souza, S., Peterson, E. R. & Morton, S. A review of longitudinal studies on antenatal and postnatal depression. Arch. Womens Ment. Health 19, 711–720 (2016).
Smolina, K., Hanley, G. E., Mintzes, B., Oberlander, T. F. & Morgan, S. Trends and determinants of prescription drug use during pregnancy and postpartum in British Columbia, 2002-2011: a population-based cohort study. PLoS ONE 10, e0128312 (2015).
Hanley, G. E. & Mintzes, B. Patterns of psychotropic medicine use in pregnancy in the United States from 2006 to 2011 among women with private insurance. BMC Pregnancy Childbirth 14, 242 (2014).
Cohen, L. S. et al. Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. JAMA 295, 499–507 (2006).
Roca, A. et al. Unplanned pregnancy and discontinuation of SSRIs in pregnant women with previously treated affective disorder. J. Affect. Disord. 150, 807–813 (2013).
Bonari, L. et al. Perinatal risks of untreated depression during pregnancy. Can. J. Psychiatry 49, 726–735 (2004).
Rotem-Kohavi, N. & Oberlander, T. F. Variations in neurodevelopmental outcomes in children with prenatal SSRI antidepressant exposure. Birth Defects Res. 109, 909–923 (2017).
Boukhris, T., Sheehy, O., Mottron, L. & Berard, A. Antidepressant use during pregnancy and the risk of autism spectrum disorder in children. JAMA Pediatr. 170, 117–124 (2016).
Man, K. K. C. et al. Prenatal antidepressant use and risk of attention-deficit/hyperactivity disorder in offspring: population based cohort study. BMJ 357, j2350 (2017).
Handal, M. et al. Motor development in children prenatally exposed to selective serotonin reuptake inhibitors: a large population-based pregnancy cohort study. BJOG 123, 1908–1917 (2016).
Skurtveit, S., Selmer, R., Roth, C., Hernandez-Diaz, S. & Handal, M. Prenatal exposure to antidepressants and language competence at age three: results from a large population-based pregnancy cohort in Norway. BJOG 121, 1621–1631 (2014).
Hurault-Delarue, C. et al. Psychomotor developmental effects of prenatal exposure to psychotropic drugs: a study in EFEMERIS database. Fundam. Clin. Pharmacol. 30, 476–482 (2016).
Brown, H. K., Hussain-Shamsy, N., Lunsky, Y., Dennis, C. E. & Vigod, S. N. The association between antenatal exposure to selective serotonin reuptake inhibitors and autism: a systematic review and meta-analysis. J. Clin. Psychiatry 78, e48–e58 (2017).
Grzeskowiak, L. E. et al. Prenatal antidepressant exposure and child behavioural outcomes at 7 years of age: a study within the Danish National Birth Cohort. BJOG 123, 1919–1928 (2016).
Liu, X. et al. Antidepressant use during pregnancy and psychiatric disorders in offspring: Danish nationwide register based cohort study. BMJ 358, j3668 (2017).
Jarde, A. et al. Neonatal outcomes in women with untreated antenatal depression compared with women without depression: a systematic review and meta-analysis. JAMA Psychiatry 73, 826–837 (2016).
Bennett, I. M., Marcus, S. C., Palmer, S. C. & Coyne, J. C. Pregnancy-related discontinuation of antidepressants and depression care visits among Medicaid recipients. Psychiatr. Serv. 61, 386–391 (2010).
Cheng, T. L. & Goodman, E. Race, ethnicity, and socioeconomic status in research on child health. Pediatrics 135, e225–e237 (2015).
Brown, H. K. et al. Association between serotonergic antidepressant use during pregnancy and autism spectrum disorder in children. JAMA 317, 1544–1552 (2017).
Sujan, A. C. et al. Associations of maternal antidepressant use during the first trimester of pregnancy with preterm birth, small for gestational age, autism spectrum disorder, and attention-deficit/hyperactivity disorder in offspring. JAMA 317, 1553–1562 (2017).
Hviid, A., Melbye, M. & Pasternak, B. Use of selective serotonin reuptake inhibitors during pregnancy and risk of autism. N. Engl. J. Med. 369, 2406–2415 (2013).
Viktorin, A., Uher, R., Reichenberg, A., Levine, S. Z. & Sandin, S. Autism risk following antidepressant medication during pregnancy. Psychol. Med. 47, 2787–2796 (2017).
Guhn, M. et al. Examining the social determinants of children’s developmental health: protocol for building a pan-Canadian population-based monitoring system for early childhood development. BMJ Open 6, e012020 (2016).
Janus, M. & Offord, D. R. Development and psychometric properties of the Early Development Instrument (EDI): a measure of children’s school readiness. Can. J. Behav. Sci. 39, 1–22 (2007).
Brinkman, S. et al. Associations between the early development instrument at age 5, and reading and numeracy skills at ages 8, 10 and 12: a prospective linked data study. Child Indic. Res. 6, 695–708 (2013).
Forer, B. & Zumbo, B. Validation of multilevel constructs: validation methods and empirical findings for the EDI. Soc. Indic. Res. 103, 231 (2011).
Janus, M., Walsh, C., & Duku, E. Early Development Instrument: Factor structure, sub-domains and Multiple Challenge Index (Offord Centre for Child Studies, McMaster University, Hamilton, ON, 2005).
Schneeweiss, S. et al. High-dimensional propensity score adjustment in studies of treatment effects using health care claims data. Epidemiology 20, 512–522 (2009).
Austin, P. C. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharmacol. Stat. 10, 150–161 (2011).
Austin, P. C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat. Med. 28, 3083–3107 (2009).
SAS System for Windows 9.4 (SAS Institute, Cary, NC, 2014).
Hanley, G. E., Brain, U. & Oberlander, T. F. Prenatal exposure to serotonin reuptake inhibitor antidepressants and childhood behavior. Pediatr. Res. 78, 174–180 (2015).
Brandlistuen, R. E. et al. Behavioural effects of fetal antidepressant exposure in a Norwegian cohort of discordant siblings. Int. J. Epidemiol. 44, 1397–1407 (2015).
Galbally, M., Lewis, A. J. & Buist, A. Child developmental outcomes in preschool children following antidepressant exposure in pregnancy. Aust. NZ J. Psychiatry 49, 642–650 (2015).
Hanley, G. E., Brain, U. & Oberlander, T. F. Infant developmental outcomes following prenatal exposure to antidepressants, and maternal depressed mood and positive affect. Early Hum. Dev. 89, 519–524 (2013).
Viktorin, A. et al. Association of antidepressant medication use during pregnancy with intellectual disability in offspring. JAMA Psychiatry 74, 1031–1038 (2017).
Rommel, A. S., Bergink, V., Liu, X., Munk-Olsen, T. & Molenaar, N. M. Long-term effects of intrauterine exposure to antidepressants on physical, neurodevelopmental, and psychiatric outcomes: a systematic review. J. Clin. Psychiatry 81, 19r12965 (2020).
Ansorge, M. S., Zhou, M., Lira, A., Hen, R. & Gingrich, J. A. Early-life blockade of the 5-HT transporter alters emotional behavior in adult mice. Science 306, 879–881 (2004).
Brummelte, S., Mc Glanaghy, E., Bonnin, A. & Oberlander, T. F. Developmental changes in serotonin signaling: Implications for early brain function, behavior and adaptation. Neuroscience 342, 212–231 (2017).
Hanley, G. E., Park, M. & Oberlander, T. F. Socieconomic status and psychotropic medicine use during pregnancy: a population-based study in British Columbia, Canada. Arch. Womens Ment. Health 23, 689–697 (2020).
Acknowledgements
This research was funded by the Canadian Institutes of Health Research (CIHR) Grant 117135. M.P. was supported by a CIHR Doctoral Research Award. G.E.H. is supported by a Canadian Institutes for Health Research New Investigator Award. T.F.O. is the R. Howard Webster Professor in Brain Imaging and Child Development. The authors also thank Ursula Brain for her careful review of the manuscript.
Author information
Authors and Affiliations
Contributions
M.P. and T.F.O. conceptualized and designed the study and produced the first draft of the manuscript. M.P. conducted all analyses. G.E.H. and T.F.O. were involved in data acquisition. All authors participated in critical review and interpretation of results and revisions and approval of the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent statement
Patient consent was not required as data were de-identified, anonymized, and from secondary sources.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Park, M., Hanley, G.E., Guhn, M. et al. Prenatal antidepressant exposure and child development at kindergarten age: a population-based study. Pediatr Res 89, 1515–1522 (2021). https://doi.org/10.1038/s41390-020-01269-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01269-6