Abstract
Background
Birth weight percentiles provide limited information on qualitative infant growth. Body composition provides estimates of fat mass, fat-free mass, and body fat percentage (adiposity). We sought to implement assessment of body composition at birth into clinical practice using a validated anthropometric equation and to evaluate measurement reliability.
Methods
Body composition was incorporated into newborn nursery admission procedure. Body fat percentage derived from skinfold measurements performed by clinical nurses were compared to a historical database of similar measurements performed on newborns by experienced research staff. Body Mass Index (BMI) and Ponderal Index (PI) were used as surrogates for adiposity. Comparison of correlations between groups assessed measurement reliability. P < 0.05 was considered significant.
Results
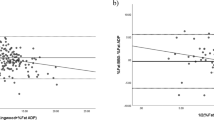
Nine hundred and ninety-one infants had body composition evaluated. Correlations were similar between BMI and %BF for measurements performed by research and clinical nurses (r2 = 0.82 versus r2 = 0.80; P = 0.142 for the difference between correlation coefficients) demonstrating good reliability. Similar results were found using PI (r2 = 0.58 versus r2 0.53; P = 0.105).
Conclusions
Body composition can be assessed at birth using a validated anthropometric equation. Measurements performed by clinical RNs were found to be reliable, allowing for a qualitative measure of growth beyond birth weight.
Impact
-
Assessment of neonatal body composition at birth can be implemented into routine clinical practice using an anthropometric equation to estimate fat free-mass, fat mass, and percentage body fat.
-
It provides a detailed, reproducible protocol to incorporate into routine practice.
-
Assessment of fat mass, fat-free mass, and adiposity at birth allows for a qualitative measure of intrauterine growth beyond birth weight.
-
Routine assessment of body composition provides a foundation for longitudinal follow-up of metabolic health in infancy and childhood.
Similar content being viewed by others
Introduction
The standard clinical anthropometric method to determine adequacy of infant growth endorsed by the Center for Disease Control and the American Academy of Pediatrics is the World Health Organization’s growth charts, with derived sex-specific weight-for-length, head circumference-for-age, length-for-age, and weight-for-age percentiles.1,2 These growth charts do not differentiate the proportion of body weight contributed by fat mass or lean mass and may not be optimal to assess neonatal nutritional status and qualitative growth.3 It is increasingly apparent that the presence of excess or diminished adiposity—i.e., body fat percentage (%BF)—better characterizes undernutrition or overgrowth,3 and although only represents approximately 12–14% of birth weight (BW), it accounts for approximately 50% of BW variance.4 This is seen clinically: two infants with similar BW and length will vary in their proportion of lean or fat mass. Excess or diminished adiposity in newborns is a marker for short- and long-term health outcomes5,6 and aberrant growth in infancy is consistently associated with higher adult cardiometabolic risks.7 Thus it has been suggested that body composition be incorporated into routine care and clinical practice as a measure of infant growth beyond BW.8
Current methods to assess body composition in neonates include: total body electrical conductivity (TOBEC), total body water by isotope dilution, bioelectrical impedance, dual-energy X-ray absorptiometry, magnetic resonance imaging, and air displacement plethysmography (ADP). Adapting these methods to the clinical bedside is challenging because their accessibility is limited, they are expensive and often cumbersome to use, some involve X-ray radiation exposure, and many are not specific for use in infants.9,10,11 Validated anthropometric equations using a skinfold measurement to estimate fat-mass, fat-free mass, and adiposity have been increasingly utilized in large epidemiologic studies but have not been translated into clinical practice. Limitations cited include population-specific equation assumptions, formula validation, and availability of appropriate technical training for clinical staff.8
Hence, our objective was to adapt assessment of body composition at birth into clinical practice, utilizing a previously validated neonatal anthropometric equation developed in our population and to assess the reliability of measurements performed by clinical personnel. Our hypothesis is that body composition can be successfully incorporated into the normal newborn nursery admission procedure and that clinical nurses can reliably perform measurements.
Materials and methods
This study was approved by the Institutional Review Board at MetroHealth Medical Center.
Neonatal anthropometric procedure
We utilized the National Institutes of Health, National Institute of Child Health and Human Development (NICHD), Maternal-Fetal Medicine Unit Network’s “Neonatal Anthropometric Training and Quality Assurance Protocol”, and the National Health and Nutrition Examination Survey (NHANES) III standardized anthropometric procedure12 to develop our institutional protocol. All clinical postpartum nurses underwent anthropometry training by an experienced national expert (P.M.C.). All anthropometrics were performed on admission to the newborn nursery, which is routinely within a few hours after birth.
Weight (kg) was recorded on a calibrated scale per normal nursery protocol. Previously, a tape-measure technique had been utilized for infant length (cm). Length-board measurements have superior accuracy and reproducibility,13 so an infant side-lying recumbent length board, manufactured specifically for measuring newborns (Dynamic Machine, Elyria, OH), was introduced to obtain length as follows: a cloth hospital receiving blanket was placed on the length board for hygiene and comfort. Infant was placed on the right side, and a two person or two-handed technique was used to position the head against the headboard and straighten the infant’s right knee while adjusting the foot slider, ensuring the sole of the foot was flat against the footboard. Measurements were recorded at least twice and rounded to the nearest 0.1 cm. If the two measurements were not within 0.5 cm of each other, a third length was taken. The two closest measurements were averaged and the result recorded into the electronic record. A Harpenden Skinfold Caliper© (Baty International, Sussex, UK) was used to obtain a suprailiac skinfold (mm). A 15-mm calibration block was used to calibrate the instrument prior to each use. Skinfold measurements were taken from the left side of the body, landmarked as a diagonal fold taken just above the iliac crest along the midaxillary line. Skinfolds were recorded to the nearest 0.1 mm. Measurement was recorded at least twice and rounded to the nearest 0.1 mm. If the two measurements were not within 0.5 mm of each other, a third was taken and the average of the two closest measurements was recorded in the electronic health record.
Neonatal body composition estimation
A validated anthropometric equation14 using weight, length, and suprailiac skinfold to estimate fat mass, fat-free mass, and %BF was built into the Newborn Admission Nursing Flowsheet in the Electronic Health Record (Epic, Verona, Wisconsin). This equation was developed at our institution in 1995 by Catalano et al., initially validated by comparison with TOBEC (DJ Medical Instruments Co, Auburn, IL)14 and has been used in a number of large multi-national epidemiologic studies.15,16 It was recently validated for accuracy against the PEA POD© System (Cosmed, Rome, Italy),17 a current reference method that uses ADP to non-invasively determine infant body composition. Nurses (registered nurses (RNs)) were additionally trained on proper input of all variables into the electronic record to calculate %BF from the equation. Specifically, length, weight, and suprailiac skinfold had to be entered in the same column at the same time stamp to calculate estimated neonatal fat mass, fat-free mass, and %BF.
Statistical methods
The clinical dataset for this analysis consisted of a cohort of infants admitted to the routine newborn nursery who had all measurements available (weight, length, suprailiac skinfold) and a calculated %BF. The anthropometric equation was not validated in infants <2000 g,14 so infants below this BW were excluded from our analysis. A comparison group of infants was utilized from a de-identified Institutional Review Board-approved internal research database at our institution. This database includes all research studies we have performed at our institution with neonatal body composition as one of the primary outcomes, over the past 15 years. Infants were similarly measured within a few hours of birth, with %BF calculated from anthropometrics performed by experienced research RNs. These are not the same infants on which the original equation was developed.
To evaluate the reliability of %BF calculated from anthropometric measurements in each group, we used the clinical surrogates for adiposity, Body Mass Index (BMI in kg/m2) and Ponderal Index (PI in kg/cm3). We ran separate analyses with BMI and then PI as both are used in clinical practice. BMI and PI are anthropometric indices on different measurement scales than calculated %BF, so were treated as independent. The coefficients of determination (r2) were derived using linear regression and the Pearson correlation coefficients (r) were calculated for both groups. To enable comparison of correlations from two independent groups of different sample sizes, Fisher’s r to Z transformation was used to transform the r values into z scores. The z scores are compared and analyzed for statistical significance by determining the observed z test statistic. An online statistical calculator was used.18 The z test statistic was set at an alpha level of 0.05. Descriptive statistics were performed using the Data Analysis ToolPak in Excel for Windows (2016). Anthropometric data was expressed as mean ± SD.
Results
Body composition measurements were incorporated into the normal newborn nursery RN admission procedure. A total of 1080 eligible infants were admitted to the newborn nursery during the study period (March to July 2018). Detailed anthropometrics were available for analysis on 991 (92%). Reasons an infant did not have all measurements available included: short interval neonatal intensive care unit transfer (5%), a skinfold was not performed on nursery admission (1%), and all measurements were performed but then entered incorrectly into the electronic record so %BF was not calculated (2%). We excluded one infant with a negative %BF whose BW of 2005 g was just at the threshold of the BW cut-off for validation of the anthropometric equation. Similarly, in the research RN cohort we excluded one infant with a calculated negative %BF, whose BW was 2020 g, otherwise all infants from the historical database were included. Demographics for both groups are described in Table 1. The groups were similar in terms of neonatal anthropometrics, with no differences in fat mass or %BF. The infants in the research cohort had higher mean BWs with more lean mass and thinner skinfolds.
When compared, correlations were similar between BMI and %BF for measurements performed by research (r2 = 0.82; n = 1093) and clinical nurses (r2 = 0.80; n = 991) and were not statistically different (Fig. 1; P = 0.142). Similar results were seen using PI and were not significant between nurse groups (Fig. 2; P = 0.105). A stronger relationship was seen between BMI and %BF (r2 = 0.82, research RN; r2 = 0.80, clinical RN) versus PI and %BF (r2 = 0.58, research RN; r2 = 0.53, clinical RN) in both groups.
Discussion
The key finding of this study is that body composition measurements of the newborn can be implemented into routine clinical practice and measurements performed by clinical personnel are reliable. We confirmed our hypothesis and found similar correlations with anthropometric indices for %BF calculated from skinfold measurements performed by clinical nurses versus experienced research personnel. These results demonstrate that a validated anthropometric equation can be used clinically to assess %BF and that a reproducible protocol can be developed to incorporate this model into routine care.
Utilizing a validated anthropometric equation to assess body composition at birth is a simple, inexpensive method to expand our evaluation of growth beyond BW. Several prediction equations exist to estimate neonatal body composition from skinfold thickness.14,19,20,21 Some involve a single skinfold, while others involve multiple skinfolds in a number of locations (i.e., subscapular, triceps, suprailiac, thigh). Some are limited by the size and demographics of the study population used to develop the model and others by the method used to validate the equation. We chose the Catalano et al. equation, as it was developed in our population, has been used in several large clinical studies conducted by the Maternal-Fetal Network Unit involving a multi-ethnic, multi-national newborn population,15,16 and has the advantage of only involving a single skinfold, minimizing error and facilitating ease of use. Additionally, the equation has been found to be similarly accurate in predicting neonatal fat mass in several populations when evaluated against the PEA POD©,17 which uses air displacement plethysmography to non-invasively determine %BF specifically developed for use in infants,22 and the current research standard for assessment of body composition in this population.23 As the PEA POD© is not practical for routine clinical use, we feel a prediction equation that performs similarly would be an excellent surrogate.
Assessment of body composition at birth enhances our understanding of how maternal metabolic conditions affect in utero acquisition of neonatal lean and fat mass and that adiposity at birth may better characterize the risk of subsequent neonatal morbidity versus BW centile alone. Previous studies have demonstrated that infants exposed to gestational diabetes, poorer glycemic status, and obesity all have increasing adiposity. Durnwald et al. reported that large-for-gestational age infants of women with gestational diabetes (GDM) had increased fat mass as compared to those with normal glucose tolerance, despite no significant differences in BW or lean body mass.24 Durnwald et al. also found that poorer maternal glycemic control was associated with increased fat mass in normal BW newborns.25 Andersson-Hall et al. reported a similar relationship between %BF and GDM and also examined anthropometrics from 1 week to 1 year of life and found infants born to obese women had higher %BF compared with those born to normal weight gravidas.26 Others have investigated the impact of low %BF and demonstrated that, despite an AGA BW, an infant can have clinical evidence of malnutrition when adiposity is examined27,28,29 and that newborn wasting is associated with short-term morbidity and mortality,30 further supporting the importance of an assessment beyond BW. Indeed, the phenomenon of the “thin-fat baby” has been well described in the works of Dr. Ranjan Yajnik, where an infant who is small or thin by body weight is metabolically obese due to increased adiposity. This “muscle-thin but adipose” phenotype is associated with persistent adiposity in childhood with increased insulin resistance.31 All of the above suggest that body composition is an important adjunct measure of fetal growth in addition to BW centiles and small, appropriate, and large for gestational age categorizations.
Finally, assessment of body composition at birth provides a foundation for longitudinal follow-up of metabolic health in infancy and childhood and may provide critical information concerning risks of future disease development, with potential to target earlier interventions. Indeed, in a study by Catalano et al., which examined the perinatal risk factors for childhood obesity, no association was found between BW and body weight at age 8 years; however, a strong correlation was seen between %BF at birth and at 8 years of age.32 Our method utilizing an anthropometric equation could be easily transitioned into outpatient practice to provide ongoing follow-up of body composition throughout infancy, childhood, and beyond.
A strength of our study is that we have provided a model for implementation of body composition into clinical practice. As a large academic center with an ethnically diverse population and approximately 3000 deliveries annually, these results are very generalizable. We also found the body composition results in our sample to be similar to published norms.33,34,35,36,37 Another strength is, in addition to assessment of adiposity or %BF, the anthropometric equation provides estimates of both fat mass and fat-free mass, the latter of which may be as significant as %BF in predicting long-term metabolic risks. Other strengths include the systematic and detailed methodology we utilized for anthropometric training, following the NHANES III and NICHD’s standard procedures. Recent reviews highlight the challenges and limitations of varying body composition methods to assess adiposity10,11,38 Limitations of all anthropometric models utilizing skinfolds to estimate %BF include technical and measurement error, concerns for reliability and accuracy, and methods for quality control. Though we took rigorous measures to minimize these sources of error, including ongoing quality assessment of measurements, retraining sessions, and continuing education, our model is subject to these same limitations. Our previous studies have reported on inter-rater reliability and the coefficient of variation was found to be low for anthropometric measurements performed by trained research personnel.14 We did not assess inter-rater reliability in this study but presume it would be similar among clinical staff. Utilization of anthropometric indices (such as BMI and PI) to assess reliability of measurements is a study limitation, as is the comparison to a historical cohort. Finally, the anthropometric equation is limited to infants >2000 g and cannot be used to estimate body composition in very low BW infants.
Future research will focus on deriving sex- and gestational age-specific reference curves for body composition at birth utilizing the anthropometric equation developed by Catalano et al. Though there are a few published papers providing reference charts for newborn assessment of body composition,33,34,35,36,37 all were derived using the PEA POD©, so may not be applicable to data obtained with an anthropometric equation. An additional goal is to identify the upper and lower limits for newborn body composition associated with increased long-term health risks. More longitudinal outcome data in our population need to be investigated to determine this. Additionally, several studies are underway measuring serum and urine biomarkers to predict body composition. Together with routine anthropometric assessment, this may serve as a pragmatic clinical approach in following body composition in infants over time.
Based on our results, consideration should be given to adapting neonatal body composition into routine clinical practice as an adjunct measure of growth. Assessment of adiposity, fat mass, and fat-free mass enhances our understanding of infant nutritional status. Our experience provides adequate instruction and motivation to replicate this effort on a larger national scale.
References
World Health Organization. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-age, Weight-for-Height and Body Mass Index-for-Age: Methods and Development (World Health Organization, Geneva, 2006).
Grummer-Strawn, L. M. et al. Use of the World Health Organization and CDC growth charts for children aged 0-59 months in the United States. MMWR Recomm. Rep. 59, 1–15 (2010).
Wells, J. C. K., Chomtho, S. & Fewtrell, M. S. Programming of body composition by early growth and nutrition. Proc. Nutr. Soc. 66, 423–434 (2007).
Catalano, P. M., Drago, N. M. & Amini, S. B. Factors affecting fetal growth and body composition. Am. J. Obstet. Gynecol. 172, 1459–1463 (1995).
Ellis, K. J. Body composition in infancy: impact on health later in life. Nestle Nutr. Workshop Ser. Pediatr. Program 65, 213–220 (2010). Discussion 221–224.
Catalano, P. M., Thomas, A., Huston-Presley, L. & Amini, S. B. Increased fetal adiposity: a very sensitive marker of abnormal in utero development. Am. J. Obstet. Gynecol. 189, 1698–1704 (2003).
Woo, J. G. Infant growth and long-term cardiometabolic health: a review of recent findings. Curr. Nutr. Rep. 8, 29–41 (2019).
Johnson, M. J. & Beattie, R. M. Making body composition measurement a part of routine care in children. Clin. Nutr. 37, 763–764 (2018).
Ellis, K. J. Evaluation of body composition in neonates and infants. Semin. Fetal Neonatal Med. 12, 87–91 (2007).
Cornier, M.-A. et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation 124, 1996–2019 (2011).
Wells, J. C. K. & Fewtrell, M. S. Measuring body composition. Arch. Dis. Child. 91, 612–617 (2006).
Johnson, C. L., Dohrmann, S. M., Burt, V. L. & Mohadjer, L. K. National health and nutrition examination survey: sample design 2011–2014. Vital Health Stat. 162, 1–33 (2014).
Corkins, M. R., Lewis, P., Cruse, W., Gupta, S. & Fitzgerald, J. Accuracy of infant admission lengths. Pediatrics 109, 1108–1111 (2002).
Catalano, P. M., Thomas, A. J., Avallone, D. A. & Amini, S. B. Anthropometric estimation of neonatal body composition. Am. J. Obstet. Gynecol. 173, 1176–1181 (1995).
HAPO Study Cooperative Research Group. Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study: associations with neonatal anthropometrics. Diabetes 58, 453–459 (2009).
Landon, M. B. et al. A multicenter, randomized trial of treatment for mild gestational diabetes. N. Engl. J. Med. 361, 1339–1348 (2009).
Josefson, J. L., Nodzenski, M., Talbot, O., Scholtens, D. M. & Catalano, P. Fat mass estimation in neonates: anthropometric models compared with air displacement plethysmography. Br. J. Nutr. 121, 285–290 (2019).
Lenhard, W. & Lenhard, A. Psychometrica. Hypothesis tests for comparing correlations. https://www.psychometrica.de/correlation.html (2014).
Deierlein, A. L., Thornton, J., Hull, H., Paley, C. & Gallagher, D. An anthropometric model to estimate neonatal fat mass using air displacement plethysmography. Nutr. Metab. 9, 21 (2012).
Lingwood, B. E. et al. Prediction of fat-free mass and percentage of body fat in neonates using bioelectrical impedance analysis and anthropometric measures: validation against the PEA POD. Br. J. Nutr. 107, 1545–1552 (2012).
Aris, I. M. et al. Body fat in Singaporean infants: development of body fat prediction equations in Asian newborns. Eur. J. Clin. Nutr. 67, 922–927 (2013).
Urlando, A., Dempster, P. & Aitkens, S. A new air displacement plethysmograph for the measurement of body composition in infants. Pediatr. Res. 53, 486–492 (2003).
Fields, D. A., Gunatilake, R. & Kalaitzoglou, E. Air displacement plethysmography: cradle to grave. Nutr. Clin. Pract. 30, 219–226 (2015).
Durnwald, C., Huston-Presley, L., Amini, S. & Catalano, P. Evaluation of body composition of large-for-gestational-age infants of women with gestational diabetes mellitus compared with women with normal glucose tolerance levels. Am. J. Obstet. Gynecol. 191, 804–808 (2004).
Durnwald, C. P. et al. Glycemic characteristics and neonatal outcomes of women treated for mild gestational diabetes. Obstet. Gynecol. 117, 819–827. (2011).
Andersson-Hall, U. K. et al. Maternal obesity and gestational diabetes mellitus affect body composition through infancy: the PONCH study. Pediatr. Res. 85, 369–377 (2019).
Carberry, A. E., Raynes-Greenow, C. H., Turner, R. M., Askie, L. M. & Jeffery, H. E. Is body fat percentage a better measure of undernutrition in newborns than birth weight percentiles? Pediatr. Res. 74, 730–736 (2013).
Metcoff, J. Clinical assessment of nutritional status at birth. Fetal malnutrition and SGA are not synonymous. Pediatr. Clin. North. Am. 41, 875–891 (1994).
Mehta, S., Tandon, A., Dua, T., Kumari, S. & Singh, S. K. Clinical assessment of nutritional status at birth. Indian Pediatr. 35, 423–428 (1998).
Victora, C. G. et al. Anthropometric characterization of impaired fetal growth: risk factors for and prognosis of newborns with stunting or wasting. JAMA Pediatr. 169, e151431 (2015).
Chan, J. C. et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 301, 2129–2140 (2009).
Catalano, P. M. et al. Perinatal risk factors for childhood obesity and metabolic dysregulation. Am. J. Clin. Nutr. 90, 1303–1313. (2009).
Butte, N. F., Hopkinson, J. M., Wong, W. W., Smith, E. O. & Ellis, K. J. Body composition during the first 2 years of life: an updated reference. Pediatr. Res. 47, 578–585 (2000).
Hawkes, C. P. et al. Gender- and gestational age-specific body fat percentage at birth. Pediatrics 128, e645–e651 (2011).
Norris, T. et al. New charts for the assessment of body composition, according to air-displacement plethysmography, at birth and across the first 6 mo of life. Am. J. Clin. Nutr. 109, 1353–1360 (2019).
Villar, J. et al. Body composition at birth and its relationship with neonatal anthropometric ratios: the newborn body composition study of the INTERGROWTH-21st project. Pediatr. Res. 82, 305–316 (2017).
Hamatscheck et al. Fat and fat-free mass of preterm and term infants from birth to six months: a review of current evidence. Nutrients 12, 1–10 (2020).
Demerath, E. W. & Fields, D. A. Body composition assessment in the infant. Am. J. Hum. Biol. 26, 291–304 (2014).
Acknowledgements
The authors thank the clinical postpartum nurses for incorporating neonatal anthropometrics into their practice. PMC received Eunice Kennedy Shriver National Institute of Child Health and Human Development support from Grant HD 22965-19.
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: all authors. Drafting the article or revising it critically for important intellectual content: D.B.L., P.O.G., S.G.-W., P.M.C. Final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Patient consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Landau, D., Stout, J., Presley, L.H. et al. Reliability of routine anthropometric measurements to estimate body composition in term infants. Pediatr Res 89, 1751–1755 (2021). https://doi.org/10.1038/s41390-020-01136-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01136-4
This article is cited by
-
Body composition in term neonates of mothers with hypertensive disorders of pregnancy
Pediatric Research (2023)