Abstract
Background
The action spectrum for bilirubin photodegradation has been intensively studied. However, questions still remain regarding which light wavelength most efficiently photodegrades bilirubin. In this study, we determined the in vitro effects of different irradiation wavelength ranges on bilirubin photodegradation.
Methods
In our in vitro method, normalized absolute irradiance levels of 4.2 × 1015 photons/cm2/s from light-emitting diodes (ranging from 390–530 nm) and 10-nm band-pass filters were used to irradiate bilirubin solutions (25 mg/dL in 4% human serum albumin). Bilirubin and its major photoisomer concentrations were determined; the half-life time of bilirubin (t1/2) was calculated for each wavelength range, and the spectral characteristics for bilirubin photodegradation products were obtained for key wavelengths.
Results
The in vitro photodegradation of bilirubin at 37 °C decreased linearly as the wavelength was increased from 390 to 500 nm with t1/2 decreasing from 63 to 17 min, respectively. At 460 ± 10 nm, a significantly lower rate of photodegradation and thus higher t1/2 (31 min) than that at 500 nm (17 min) was demonstrated.
Conclusion
In our system, the optimum bilirubin photodegradation and lumirubin production rates occurred between 490 and 500 nm. Spectra shapes were remarkably similar, suggesting that lumirubin production was the major process of bilirubin photodegradation.
Similar content being viewed by others
Introduction
In the historic, frequently quoted classic paper, Cremer et al.1 determined the in vitro photodegradation of bilirubin (a native Z,Z-isomer) in human serum after exposure to light of different wavelength ranges through direct spectrophotometric measurements. In their study, there were only seven data points in the spectrum and the study protocol lacked detail, making replication of their results challenging. In addition, although unknown at the time, the use of a direct spectrophotometric method at 460 nm to determine the amount of bilirubin remaining after light exposure was, in retrospect, inappropriate because at this wavelength, not only bilirubin but also its photodegradative product, lumirubin, absorb light. Lumirubin, also known as cyclobilirubin and photobilirubin II (Supplemental Fig. S1),2 has been shown to be the major product of bilirubin photodegradation with a peak absorption at 453 nm and a molar light absorption coefficient of 33,000 dm3/mol • cm in human serum albumin (HSA) solution, nearly half of that of bilirubin in HSA (63,400 dm3/mol • cm at 460 nm).2,3 Exposure of bilirubin to light results in generation of a variety of other photoproducts, such as configurational E,Z/Z,E-isomers of bilirubin (Supplemental Fig. S1) that have been shown to be more easily excreted from the body than bilirubin, the Z,Z-parent compound4, but less so than lumirubin.5,6,7
Over the decades, researchers have attempted to determine the optimum wavelength range for bilirubin photodegradation through in vitro8,9,10,11 as well as in vivo studies12 in order to design optimal phototherapy devices for the management of neonatal hyperbilirubinemia.13 In fact, most of the devices presently used for phototherapy emit blue light at 460 ± 10 nm that is based on the absorption maximum of bilirubin and recommended by the American Academy of Pediatrics (AAP).4 Other devices incorporate blue–green (turquoise) light with wavelengths ranges >490 nm.14,15,16,17 However, to date many questions still remain to be answered, including safety issues. Although not confirmed in follow-up studies, an increased mortality in extremely low-birthweight neonates (≤750 g) with severe hyperbilirubinemia treated with intensive phototherapy has been demonstrated.18 Surprisingly, lumirubin has been reported to have high pro-inflammatory potential19 that might account for these epidemiological observations.
Previously, we have described an in vitro method for evaluating and comparing the efficacy of clinically used phototherapy devices15 through determination of the half-life of bilirubin in HSA (t1/2) to yield diazo-negative products. We have adapted this method for determining the in vitro effect of the irradiation wavelength on bilirubin photodegradation and the production of photoisomers. With the advent of high-power blue light-emitting diodes (LEDs), there is a wide selection of LEDs with narrow emission wavelength ranges (~24 nm). By using these LEDs together with band-pass filters, we were able to deliver light at 10-nm wavelength slices to identify the most effective wavelength for the photodegradation of bilirubin20 and to also determine the production of some photoisomers (lumirubin; mixtures of Z,E- and E,Z-isomers; and IIIα-, IXα-, and XIIIα-bilirubin). In addition, we also characterized the spectral properties of bilirubin photodegradation products upon exposure to various wavelengths.
Materials and methods
Materials
Unconjugated bilirubin (UCB) (25.0 ± 1.0 dL, [427.5 μmol/L]) was dissolved in 4% (w/v) HSA (both from Sigma-Aldrich, St Louis, MO), pH 7.4, as previously described.15 Bilirubin diazo assay reagents were prepared from stock chemicals as described previously.15 UCB photodegradation was carried out in all-glass microhematocrit tubes (75 × 1.5 outer diameter (OD) × 1.0 mm inner diameter (ID), VWR, Burlingame, CA).15 Light wavelengths and energies were determined with a properly calibrated Fiber Optic Spectrometer (Model S2000, Ocean Optics, Dunedin, FL).
Determination of bilirubin photoisomers
Determination of bilirubin photoisomers was performed using the high-performance liquid chromatography (HPLC) method modified from McDonagh et al.9 Analyses were performed using an HPLC System 1200 with a diode-array detector (Agilent Technologies, Santa Clara, CA) with a Poroshell 120, SB-C18 2.1-µm (4.6 mm (ID) × 100 mm; Agilent Technologies) column and with a mobile phase consisting of 0.1 M di-n-octylamine acetate in methanol and 8% (v/v) of water. In summary, 20 µL of irradiated bilirubin/HSA solutions was mixed with 180 µL of 0.1 M di-n-octylamine acetate in methanol (mobile phase), vortexed, and centrifuged at 3000 rpm for 5 min. Twenty microliters of resulting supernatant was loaded onto the HPLC column. The data are expressed as percentage of the initial bilirubin concentration (25.0 mg/dL).
Experimental set-up
Light exposure device
A diagram of the light exposure device is shown in Supplemental Figure S2. In brief, the device consists of: an LED-light array as a source of a specific narrow wavelength range (Supplemental Fig. 2a); a 10-nm band-pass filter (Supplemental Fig. 2b); and a temperature-controlled light exposure stage (Supplemental Fig. 2c).
The LED light sources (Mouser Electronics, Mansfield, TX; Future Electronics, Pointe Claire, QC, Canada; LED Supply, Randolph, VT, and Bright Light LED, Inc., Canoga Park, CA) consisted of 9 blue to green LEDs (3–5 W), emitting light with the maxima in the range of 380–530 nm, which were mounted with centers 10 mm apart as 3 × 3 arrays on aluminum heat sinks (Supplemental Fig. S2a). These light sources were powered by a V/A-adjustable DC Power Supply (Model 3003B, Protek, Norwood, NJ). The heat sink was cooled with iced water to keep the LED temperature at 22 ± 2 °C to maintain a stable light flux.
The interchangeable LED light sources were mounted on a light-transmitting device (Supplemental Fig. S2b), which consisted of a holder for the appropriate band-pass filter and light-diffusing barrel (50 × 46 × 52 mm, length × ID × OD) fitted with a dimpled aluminum foil around the internal diameter to deliver a field of nearly uniform and stable light flux with a narrow (~10 nm) wavelength range to the reaction tube exposure stage (Supplemental Fig. S2c). Band-pass filters, 50 mm in diameter with 10-nm bandwidths in the 390–530 nm range, were obtained from Andover Corp. (Salem, NH). The band-pass filter significantly limits the spectral bandwidth but not the peak emission wavelength of the light source.
The reaction tube exposure stage consisted of a plate, which had a 5 × 5 array of closely spaced ¼” (6.4 mm) holes so that measurements of the irradiance footprint emitted by each light transmitting device could be made. The complete irradiance footprint map for the 500-nm LED light source shows that the photon irradiance delivered across the footprint is uniform (Supplemental Fig. S3). The inner 5 × 5-cm2 area represents the position where the reaction tubes were exposed to light. During exposure of the reaction tubes, the holes were covered with a 0.25-mm thick, flat black-painted aluminum cover placed over the holes in the irradiance measuring plate in order to provide a uniform, non-reflecting background during light exposure. The entire apparatus was positioned on a Multi-Blok Heater (150 W, No. 2097-1, Lab-Line Instruments, Melrose Park, IL), which maintained the exposure stage temperature at 37 ± 0.5 °C.
Bilirubin irradiation experiments
The entire experimental procedure was carried out under a bilirubin-safe light, consisting of a white light LED lamp light fitted with a filter [Roscolux #312, (Canary), Rosco, Stamford, CT], allowing the transmission of only yellow/red light (>650 nm). Sets of triplicate hematocrit reaction tubes, placed side-by-side with 0.5” (12.5 mm) tape, contained 25.0 µL (~25-mm long column) of 25 ± 0.25 mg of UCB/dL in 4% HSA, pH 7.4. The exposure stage was then illuminated with the desired wavelength of normalized light exposure with 4.2 × 1015 photons/cm2/s as measured with the Ocean Optics spectrometer. This flux of photons is equivalent to an irradiance of 1800 µW/cm2 at 460 nm or 30 µW /cm2/nm as measured with a BiliBlanket II irradiance meter (Ohmeda/GE Health Care, Laurel, MD), which has the spectral sensitivity of 400–520 nm, a bandwidth of 60 nm, and a peak sensitivity at 450 nm. Irradiance levels were adjusted immediately prior to and checked immediately after each exposure period. After exposure of the tubes containing a bilirubin/HSA solution for up to 120 min, 3 tubes were removed periodically, and the bilirubin/HSA solutions in each tube were subsequently transferred to 7-mL glass test tubes (n = 3) containing 650 µL of diazo reagent. After a reaction time of at least 15 min (up to 120 min) and addition of 1350 µL of reverse osmosis water, the absorbance at 560 nm was measured in a spectrophotometer fitted with Micro Flow cuvette (UV-160, Shimadzu Corp., Columbia, MD). The concentration of remaining bilirubin, relative to its concentration at t = 0 min, was calculated, graphed as percentage, and t1/2 values (in min) were determined by interpolation (see Fig. 1c).
Comparison of methods for the bilirubin quantitation. a Time course and t1/2 of in vitro bilirubin photodegradation measured by the direct spectrophotometric method at 460 nm (as used by Cremer et al.1) compared to the present method that measures only the diazo-reactive compounds remaining in the light-exposed reaction tubes, upon the 500-nm light-emitting diode light irradiation in both methodologies. b Reaction temperature and the rate of bilirubin photodegradation. % Bilirubin left was determined by the diazo method at different reaction temperatures using a 500-nm light with constant average flux of 4.2 × 1015 photons/cm2/s. c Representative bilirubin photodegradation time courses. Time courses for bilirubin photodegradation at 460 and 500 nm, representing the presently considered optimal peak, 460 ± 10 nm, and the wavelength peak found to be optimal in the current study. The time courses demonstrate how t1/2 values are obtained through interpolation
Spectral analysis of bilirubin photodegradation products
A solution of HSA (0.40 g) in aqueous 0.1 M phosphate-buffered saline (PBS, 7.5 mL, pH = 7.4) was added to a solution of UCB (2.5 mg, Carl Roth, Karlsruhe, Germany) in aqueous 0.1 M NaOH (200 μL). The resulting mixture was added to PBS (10 mL). This stock solution of UCB (25.4 mg/dL [434.3 µmol/L]) was diluted with PBS to the final concentration of 65.3 µmol/L (3.82 mg/dL), which was used for the following experiments.
A stirred solution of bilirubin with HSA in PBS (pH = 7.4, I = 0.1 M) in a 1-cm matched quartz cuvette was irradiated using LEDs (λmax = 405 or 505 nm). The reaction was simultaneously monitored by UV-Vis spectrometry using a diode-array spectrophotometer Agilent Technologies 8453. The emission spectra were measured on a luminescence spectrometer (FLS920-stm, Edinburgh Instruments Ltd, Edinburgh, UK) in a 1-cm path quartz fluorescence cuvette at 25 ± 1 °C.
Statistical analyses
Statistical significance was calculated using unpaired, two-tailed t tests with differences deemed significant when p ≤ 0.05.
Because this was an in vitro study, no institutional review board approval and informed consent were required.
Results
Factors affecting bilirubin photodegradation
As can be seen in Fig. 1, different experimental parameters can substantially affect the observed rate of bilirubin photodegradation as assessed by t1/2 calculations. The t1/2 for the 500 ± 5 nm spectral slice at 4.2 × 1015 photons/cm2/s using a direct spectrophotometric method at 460 nm as used by Cremer et al.1 was much higher compared with that determined by the diazo bilirubin quantitation method (Fig. 1a). These results indicate a very low accuracy and specificity of direct spectrophotometry for the determination of bilirubin photodegradation. When the same light source was used to determine the effect of temperature on bilirubin photodegradation, a negative correlation between the reaction temperature and t1/2 (18 min at 37 °C) was found, with t1/2 decreasing dramatically with increasing reaction temperature (Fig. 1b). Based on these findings, all subsequent t1/2 measurements were carried out at 37 °C to reflect physiological conditions. Representative t1/2 determined by the diazo method and a comparison of results obtained with exposure to 4.2 × 1015 photons/ cm2/s at 460 and 500 nm is shown in Fig. 1c. We found the mean t1/2 of 31 and 17 min at 460 and 500 nm, respectively.
We also investigated the relationship between bilirubin and HSA concentrations on t1/2. With increasing bilirubin concentrations, we found a nearly linear relationship (r = 0.95) as a function of t1/2 (Fig. 2a). At low bilirubin levels (<4 mg/dL, [68.4 µmol/L]), there was a concentration dependence in t1/2; whereas, at higher bilirubin levels (≥4 mg/dL, [68.4 µmol/L]), the observed rate of bilirubin photodegradation was considerably slower. When HSA concentrations were varied, we also found a direct relationship between HSA concentrations and t1/2 (Fig. 2b), with higher HSA concentrations giving longer t1/2. Based on these findings, we chose to use a solution of 25 mg/dL (427.5 µmol/L) of UCB in 4% HSA for all subsequent studies.
Effect of bilirubin and human serum albumin (HSA) concentrations on t1/2. a Effect of increasing bilirubin concentration (3.125–25.0 mg/dL [53.4–427.5 µmol/L]) on t1/2 with constant HSA concentration [4% (w/v), black line) and constant bilirubin/HSA molar ratios (0.5, dashed line). b Effect of increasing HSA concentrations [0–6% (w/v)] on t1/2 with constant bilirubin concentrations at 25 mg/dL. Values represent the mean of 3 measurements
The effect of light wavelength on bilirubin photodegradation
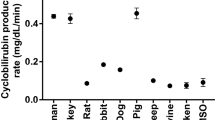
The in vitro photodegradation of bilirubin at 37 °C decreased in a linear fashion as the wavelength increased from 390 to 500 nm with t1/2 decreasing from 63 to 17 min, respectively (Fig. 3). At 460 ± 10 nm, which is currently considered to be an optimum wavelength range for phototherapy (light gray area), we found a clear and significantly lower rate of photodegradation and thus higher t1/2 (31 min) than that at 500 nm (dark gray area, 17 min).
In vitro bilirubin action spectrum. Bilirubin photodegradation as determined by t1/2 measurements over the spectral wavelength range from 390 to 530 nm using light-emitting diodes and band-pass filters in 10-nm increments. Each t1/2 represents the mean ± SD of 2–6 measurements at the specific spectral wavelength. The lightly shaded area illustrates the currently recommended wavelength range of 450–470 nm for phototherapy. The heavily shaded area illustrates the most efficient wavelength range of 490–510 nm determined from the present results. *p < 0.05 vs. 390–470, 520, or 530 nm using Student’s unpaired two-tailed t test
Using HPLC,9 we measured the amounts of photoisomers formed after exposure to different wavelength ranges. We found that the concentration ratios of lumirubin; the mixtures of Z,E- and E,Z-isomers; and IIIα-, IXα-, and XIIIα-bilirubin were dependent on the irradiation light wavelengths (Table 1). Lumirubin formation increased linearly upon exposure to longer wavelengths (from 390 to 500 nm), reaching a maximum at 500 nm, and rapidly decreasing thereafter (Fig. 4a, Table 1). In addition, an increase in lumirubin production was observed after exposure to light at 500 nm compared with that at 450 nm at all exposure times (Fig. 4b, Table 1).
The effect of irradiation wavelengths on the absorption spectra
A solution of UCB and HSA in aqueous PBS was irradiated by blue LEDs (405 nm) and the degradation of UCB was monitored every 5 min by absorption spectroscopy. The decrease of absorption at 460 nm (the major signal of UCB) and formation of photoproducts (the increase of absorptions at 350, 375, and 580 nm, respectively) with the absorption maxima at 350, 375, and 580 nm were observed during continual irradiation (Fig. 5a). These photoproducts were further decomposed (the disappearance of those absorption signals) by a continuous irradiation prolonged to several hours. The UCB sample irradiated by green light (505-nm LEDs) resulted in photoproducts with the similar absorption bands as those formed by blue light irradiation (the absorption maxima at 375 and 580 nm, Fig. 5b); however, the band at 350 nm was less pronounced. Upon prolonged green light irradiation, the photoproducts very slowly decomposed, probably due to an already small absorbance at the excitation wavelength.
Absorption spectra of unconjugated bilirubin (UCB) with human serum albumin (HSA) in phosphate-buffered saline (PBS) irradiated at a 405 and b 505 nm, recorded every 5 min (the last spectrum is shown as a red dot line). Subsequently (a after 90 min and b after 140 min of irradiation), monitoring the course of the reaction by absorption spectroscopy was prolonged to 30 min. c Absorption spectra of UCB with HSA in PBS irradiated at 505 nm (the last spectrum is shown as a green line). Subsequently (after 170 min of irradiation at 505 nm), the sample was irradiated at 405 nm (from spectrum with green thick line), and the spectra were recorded every 5 min (the last spectrum is shown as a red dot line). The irradiation was then monitored every 30 min. Arrow represents the spectral change during irradiation
Irradiation of UCB with green LEDs followed by irradiation with blue LEDs resulted in the same total decomposition pattern (Fig. 5c). The UCB absorption band at 460 nm slightly hypsochromically shifted (i.e., to a shorter wavelength) during green light irradiation when compared to that of blue light irradiation (Fig. 5a).
The fluorescence emission spectra were measured during continuous irradiation of a UCB solution (λexc = 310 nm) by either blue (405 nm, Fig. 6a) or green (505 nm, Fig. 6b) LEDs. Different emission spectra point again to different concentrations of the UCB isomers being formed under different irradiation conditions. The specific emission of lumirubin21 at 415 nm cannot be distinguished in the observed emission spectra due to a signal overlap of the other photoproducts present in the solution, which are also excited at 310 nm (λexc).
Discussion
Our in vitro study focused on the determination of optimal light wavelengths to be used in phototherapy of neonatal jaundice and was performed after a strict control of the major, and possibly confounding, factors. We constructed a special photochemical reactor (Supplemental Fig. S2) that delivers normalized photon flux for the given wavelength. Results from these experiments support the findings of a number of in vitro and in vivo studies, which suggest that longer wavelengths for phototherapy are the most suitable.8,9,10,22,23 These studies, however, used a xenon arc or fluorescent lamps as the light sources, which emit broader wavelength radiation compared with those of the LED/filter combinations used in our study. In addition, other factors were also not controlled properly.
The analytical methods routinely used for bilirubin determination are not optimal. The direct spectrophotometry method of bilirubin determination described by Cremer et al.1 could not be applied for our studies because bilirubin as well as its photoproducts (lumirubin) have nearly identical absorption maxima (~450 nm) and similar molar absorption coefficients, and thus they are not discriminated using this method. Therefore, we measured bilirubin (diazo reaction) (Fig. 1a) and its photoisomers (HPLC) concentrations precisely. In addition, we ensured that the reaction temperature was kept at the physiological temperature of 37 °C. In fact, significantly variable rates of bilirubin photodegradation were observed when the temperature was not properly controlled (Fig. 1b). Furthermore, the rate of bilirubin photodegradation was also affected by the concentrations of HSA or bilirubin in the irradiated solution (Fig. 2), thus serum albumin concentration under in vivo conditions is an important factor to consider.
Because an action spectrum of the initial chromophore most likely reflects its absorption spectrum, the optimum photodegradation rate of bilirubin has usually been believed to occur at 460 ± 10 nm. However, our results clearly demonstrate that bilirubin photodegradation in vitro is greatest at 500 ± 10 nm (Fig. 2), which is considerably higher than that presently used for phototherapy (460 ± 10 nm). This observation is consistent with the finding that exposure to the 500-nm wavelength also resulted in the highest rate of lumirubin formation (Fig. 4a), being nearly linearly correlated with the rate of degradation.
Earlier studies suggested that the increased bilirubin photodegradation at the higher wavelengths is mainly due to an increase in lumirubin formation,24,25,26 which was found to be more rapidly excreted in vivo6,7,27,28 in contrast to the geometric E,Z- and Z,E-isomers that could be converted back to the Z,Z-isomer.29 Since the E,Z- and Z,E-configurational isomers are also diazo-positive,10 our determination of the amount of remaining bilirubin after light exposure use of the diazo method mainly reflects the conversion of bilirubin to lumirubin, which is diazo-negative.10 This was confirmed by HPLC analyses, which showed a nearly identical wavelength-dependent lumirubin production pattern mirroring the rate of disappearance of bilirubin. It has been shown that lumirubin excretion is an important, if not primary, pathway by which bilirubin is eliminated from the body during phototherapy.5 Lumirubin is found in the urine7 as well as in the bile of neonates treated by phototherapy with the mean half-life of 112 min.5
Dependence of the isomerization efficiencies of UCB on the irradiation wavelength can be explained by the bichromophoric nature of UCB (i.e., the molecule consisting of two light-absorbing dipyrrole units) through a geometry-dependent electronic coupling.9 The variations of the isomerization quantum yields (ΦZE) arise from an intramolecular partitioning of the excitation energy between two chromophores (dipyrrole units) in the excited singlet state. The 4Z,15E-isomer is preferentially formed at shorter wavelengths (400 nm); whereas, at longer wavelengths (500 nm), the 4E,15Z-isomer, from which lumirubin is formed, is favored, thus accounting for better efficacies of longer wavelength phototherapy observed in in vitro studies.9,30 The rate-limiting step in the generation of lumirubin thus does not seem to be due to photocyclization but rather to the configurational isomerization of native bilirubin to the 4E,15Z-isomer. Indeed, the higher production rates of the 4E,15Z-isomer (which is thus the driving force for higher production of lumirubin) were reported in human neonates exposed to turquoise compared to blue light, although their efficacies were not different.31 This is also reflected by our data on absorption maxima of bilirubin photoproducts formed after exposure to different light wavelengths (Fig. 5a–c), because different concentration ratios of UCB isomers formed during irradiation or a pronounced formation of the 4E,15Z-isomer by green light irradiation can hypsochromically shift (i.e., to a shorter wavelength) the absorption maxima of these products compared to those of UCB and the 4Z,15E-isomer.32 Our steady-state spectroscopic results revealed the differences in the major photoproducts formation efficiencies, although the data cannot give information about a detailed chemical composition of the irradiated sample.
It should be noted, that our current findings are based on a static in vitro model of bilirubin photodegradation instead of the dynamic in vivo model, where skin optical properties may play an important role.33 Therefore, a proper in vivo validation of our findings using appropriate animal models as well as human clinical studies are still warranted. The importance of identifying the most effective and safe light wavelength for phototherapy arises mainly from a recent report that phototherapy use in extremely low birthweight neonates might be associated with a higher risk of mortality,18 possibly due to pro-inflammatory effects of bilirubin photodegradation products.19 In addition, other in vitro studies16,34,35,36 have reported that exposure to light in the wavelength range of 350–450 nm may be mutagenic to prokaryotic and eukaryotic cells.
Previous experimental and mathematical approaches for determination of the best wavelength for phototherapy took into account skin dynamics and found that the light of 480–510 nm may be the most suitable.9 However, using a semiempirical model of optical skin properties and circulating hemoglobin concentrations,37 it has recently been calculated that a narrow wavelength light of 476 ± 4 nm is the most efficient.33 Therefore, the effects of skin dynamics due to prematurity as well as differing bilirubin concentrations among infants may also affect the efficacy of phototherapy in vivo and should be taken into account.
Furthermore, there are additional biological factors possibly affecting lumirubin production. It has previously been reported38 that the combination of long-chain fatty acids with bilirubin HSA results in a change in the circular dichroism spectrum of bilirubin, a phenomenon associated with an increase in the rate of formation of lumirubin.38 In addition, binding of bilirubin to HSA might modulate the formation rate of lumirubin.30 The role of albumin binding is emphasized by observations by Goncharova et al.,39 who recently reported that lumirubin can bind to HSA at different sites from that of bilirubin and thus alter the lumirubin formation, and the primary binding sites of bilirubin on albumin are still available for binding of another molecule of bilirubin.
It is also important to emphasize that the effect favoring production of the 4E,15Z-isomer occurs in a region where the absorption of bilirubin is low, and thus a narrow irradiation wavelength range at the long wavelength edge of the bilirubin absorption band is probably not better clinically than irradiation wavelengths near the bilirubin absorption maximum.26 This is in line with the observation that, despite a more efficient production of the 4E,15Z-isomer and lumirubin by turquoise light, the overall production of these bilirubin photodegradation products may be too low to be clinically important,31 although an increased conversion to lumirubin followed by its enhanced urinary clearance6 should be considered as well. Based on all these data possibly supporting a greater in vivo efficacy of using longer wavelengths for phototherapy, it is necessary to perform clinical studies to carefully evaluate the kinetics and dynamics of bilirubin and its photoproduct production, including urinary excretion of lumirubin, in the 460–510 nm wavelength range.
According to the 2004 AAP Practice Guideline,4 special blue fluorescent tubes or LEDs should be used for the treatment of neonatal hyperbilirubinemia. If our current in vitro data could be proven to apply in vivo, a shift of wavelength from 460 ± 10 to longer wavelengths could mean a potential decrease in the duration of phototherapy, and the wavelength range for intensive phototherapy of 430–490 nm could be potentially changed to a narrower range of 470–510 nm.
In fact, commercially available phototherapy devices emitting 500-nm turquoise light are being clinically used, such as the BiliBlanket and Wallaby (GE Healthcare and Philips Children’s Ventures, respectively) devices15 as well as turquoise fluorescent lamp-based devices.14 Some studies utilizing these devices have shown that exposure to turquoise light is more effective in lowering the bilirubin levels than exposure to blue light,14 although other studies did not show any difference.31,40
In conclusion, in our in vitro system, the optimum bilirubin photodegradation and lumirubin production rates occurred at 500 nm. Spectral shapes were remarkably similar, suggesting that lumirubin production was the major process of bilirubin photodegradation. Taking into account complex interactions of biological and chemical factors, a similar methodological approach should be used in human studies to reveal all the factors affecting the phototherapy efficacy. Thus studies on human neonates treated with phototherapy should focus on the determination of the concentrations of bilirubin and its photoisomers as well as other photooxidation products not only in sera but also in urine and stool to uncover the factors affecting phototherapy efficacy in vivo.
Change history
27 February 2019
Following publication of this article, the authors noticed that an incorrect affiliation was assigned to the author “Lucie Muchová”. The original article has now been updated so that the author “Lucie Muchová” is associated with the “Institute of Medical Biochemistry and Laboratory Diagnostics, 1st Faculty of Medicine, Charles University, Kateřinská 32, 120 00 Prague, Czech Republic”. This has been corrected in both the PDF and HTML versions of the article.
References
Cremer, R. J., Perryman, P. W. & Richards, D. H. Influence of light on the hyperbilirubinemia of infants. Lancet 271, 1094–1097 (1958).
McDonagh, A. F. & Lightner, D. A. Phototherapy and the photobiology of bilirubin. Semin. Liver Dis. 8, 272–283 (1988).
Mukerjee, P., Ostrow, J. D. & Tiribelli, C. Low solubility of unconjugated bilirubin in dimethylsulfoxide - water systems: implications for pKa determinations. BMC Biochem. 3, 17–17 (2002).
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 114, 297–316 (2004).
Ennever, J. F., Costarino, A. T., Polin, R. A. & Speck, W. T. Rapid clearance of a structural isomer of bilirubin during phototherapy. J. Clin. Invest. 79, 1674–1678 (1987).
Ennever, J. F., Knox, I., Denne, S. C. & Speck, W. T. Phototherapy for neonatal jaundice: in vivo clearance of bilirubin photoproducts. Pediatr. Res. 19, 205–208 (1985).
Knox, I., Ennever, J. F. & Speck, W. T. Urinary excretion of an isomer of bilirubin during phototherapy. Pediatr. Res. 19, 198–201 (1985).
Gutcher, G. R., Yen, W. M. & Odell, G. B. The in vitro and in vivo photoreactivity of bilirubin: I. Laser- defined wavelength dependence. Pediatr. Res. 17, 120–123 (1983).
McDonagh, A. F., Agati, G., Fusi, F. & Pratesi, R. Quantum yields for laser photocyclization of bilirubin in the presence of human serum albumin. Dependence of quantum yield on excitation wavelength. Photochem. Photobiol. 50, 305–319 (1989).
Onishi, S., Itoh, S. & Isobe, K. Wavelength-dependence of the relative rate constants for the main geometric and structural photoisomerization of bilirubin IX alpha bound to human serum albumin. Demonstration of green light at 510 nm as the most effective wavelength in photochemical changes from (ZZ)-bilirubin IX alpha to (EZ)-cyclobilirubin IX alpha via (EZ)-bilirubin. Biochem. J. 236, 23–29 (1986).
Lightner, D. A., Wooldridge, T. A. & McDonagh, A. F. Photobilirubin: an early bilirubin photoproduct detected by absorbance difference spectroscopy. Proc. Natl. Acad. Sci. USA 76, 29–32 (1979).
Agati, G., Fusi, F., Donzelli, G. P. & Pratesi, R. Quantum yield and skin filtering effects on the formation rate of lumirubin. J. Photochem. Photobiol. B. 18, 197–203 (1993).
Seidman, D. S. et al. A prospective randomized controlled study of phototherapy using blue and blue-green light-emitting devices, and conventional halogen-quartz phototherapy. J. Perinatol. 23, 123–127 (2003).
Ebbesen, F., Agati, G. & Pratesi, R. Phototherapy with turquoise versus blue light. Arch. Dis. Child. Fetal Neonatal Ed. 88, F430–F431 (2003).
Vreman, H. J., Wong, R. J., Murdock, J. R. & Stevenson, D. K. Standardized bench method for evaluating the efficacy of phototherapy devices. Acta Paediatr. 97, 308–316 (2008).
Roll, E. B. & Christensen, T. Formation of photoproducts and cytotoxicity of bilirubin irradiated with turquoise and blue phototherapy light. Acta Paediatr. 94, 1448–1454 (2005).
Vandborg, P. K., Hansen, B. M., Greisen, G. & Ebbesen, F. Dose-response relationship of phototherapy for hyperbilirubinemia. Pediatrics 130, e352–e357 (2012).
Morris, B. H. et al. Aggressive vs. conservative phototherapy for infants with extremely low birth weight. N. Engl. J. Med. 359, 1885–1896 (2008).
Jašprová, J. et al. Neuro-inflammatory effects of photodegradative products of bilirubin. Sci. Rep. 8, 7444 (2018).
Yasuda, S., Itoh, S., Imai, T., Isobe, K. & Onishi, S. Cyclobilirubin formation by in vitro photoirradiation with neonatal phototherapy light. Pediatr. Int. 43, 270–275 (2001).
Bacci, M., Linari, R., Agati, G. & Fusi, F. UV excitable fluorescence of lumirubin. J. Photochem. Photobiol. B 3, 419–427 (1989).
Migliorini, M. G., Galvan, P., Sbrana, G., Donzelli, G. P. & Vecchi, C. Bilirubin photoconversion induced by monochromatic laser radiation. Comparison between aerobic and anaerobic experiments in vitro. Biochem. J. 256, 841–846 (1988).
Greenberg, J. W., Malhotra, V. & Ennever, J. F. Wavelength dependence of the quantum yield for the structural isomerization of bilirubin. Photochem. Photobiol. 46, 453–456 (1987).
Ennever, J. F., Knox, I. & Speck, W. T. Differences in bilirubin isomer composition in infants treated with green and white light phototherapy. J. Pediatr. 109, 119–122 (1986).
Itoh, S., Onishi, S., Isobe, K., Manabe, M. & Yamakawa, T. Wavelength dependence of the geometric and structural photoisomerization of bilirubin bound to human serum albumin. Biol. Neonate 51, 10–17 (1987).
Ennever, J. F. & Dresing, T. J. Quantum yields for the cyclization and configurational isomerization of 4E,15Z-bilirubin. Photochem. Photobiol. 53, 25–32 (1991).
Pratesi, R. et al. Laser investigation of bilirubin-photobilirubin photoconversion. Pediatr. Res. 19, 166–171 (1985).
Costarino, A. T. Jr, Ennever, J. F., Baumgart, S., Speck, W. T. & Polin, R. A. Effect of spectral distribution on isomerization of bilirubin in vivo. J. Pediatr. 107, 125–128 (1985).
Onishi, S. et al. Metabolism of bilirubin and its photoisomers in newborn infants during phototherapy. J. Biochem. 100, 789–795 (1986).
Agati, G., Fusi, F., Pratesi, R. & McDonagh, A. F. Wavelength-dependent quantum yield for Z----E isomerization of bilirubin complexed with human serum albumin. Photochem. Photobiol. 55, 185–190 (1992).
Ebbesen, F. et al. Bilirubin isomer distribution in jaundiced neonates during phototherapy with LED light centered at 497 nm (turquoise) vs. 459 nm (blue). Pediatr. Res. 80, 511–515 (2016).
Kanna, Y., Arai, T. & Tokumaru, K. Photoisomerization of bilirubins and the role of intramolecular hydrogen-bonds. Bull. Chem. Soc. Jpn. 66, 1482–1489 (1993).
Parshad, R., Sanford, K. K., Jones, G. M. & Tarone, R. E. Fluorescent light-induced chromosome damage and its prevention in mouse cells in culture. Proc. Natl. Acad. Sci. USA 75, 1830–1833 (1978).
Linfield, D. T. et al. The effect of hematocrit on in vitro bilirubin photoalteration. Pediatr. Res. 79, 387–390 (2016).
Sideris, E. G., Papageorgiou, G. C., Charalampous, S. C. & Vitsa, E. M. A spectrum response study on single strand DNA breaks, sister chromatid exchanges, and lethality induced by phototherapy lights. Pediatr. Res. 15, 1019–1023 (1981).
Speck, W. T. & Rosenkranz, H. S. Base substitution mutations induced in Salmonella strains by visible light (450 nm). Photochem. Photobiol. 21, 369–371 (1975).
Lamola, A. A. & Russo, M. Fluorescence excitation spectrum of bilirubin in blood: a model for the action spectrum for phototherapy of neonatal jaundice. Photochem. Photobiol. 90, 294–296 (2014).
Malhotra, V., Greenberg, J. W., Dunn, L. L. & Ennever, J. F. Fatty acid enhancement of the quantum yield for the formation of lumirubin from bilirubin bound to human albumin. Pediatr. Res. 21, 530–533 (1987).
Goncharova, I., Jasprova, J., Vitek, L. & Urbanova, M. Photo-isomerization and oxidation of bilirubin in mammals is dependent on albumin binding. Anal. Biochem. 490, 34–45 (2015).
Ebbesen, F. et al. Effect of phototherapy with turquoise vs. blue LED light of equal irradiance in jaundiced neonates. Pediatr. Res. 79, 308–312 (2016).
Acknowledgements
We thank Bright Light LED, Inc. for donating some of the sets of LEDs. This study was supported in part by a grant from Children’s Ventures, a Division of Philips Electronics North America Corp., the Christopher Hess Research Fund, the Mary L. Johnson Research Fund, and the H.M. Lui Research Fund. The study was also supported by the Czech Ministry of Health (grants NV18-07-00342 and RVO-VFN64165/2018).
Author information
Authors and Affiliations
Contributions
H.J.V. designed the study and performed all the irradiation efficacy experiments; S.K. contributed to the irradiation efficacy experiments; J.J. performed analyses on HPLC determination of bilirubin photoisomers, B.K.C. contributed to the irradiation efficacy experiments; L.L. performed steady-state absorption and emission spectroscopy of bilirubin and its photodegradation prkoducts; P.K. contributed to the bilirubin photoisomer spectral analyses, L.V., L.M., R.J.W., and D.K.S. contributed to the study design. All authors contributed to the data interpretation and writing and approving the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Vreman, H.J., Kourula, S., Jašprová, J. et al. The effect of light wavelength on in vitro bilirubin photodegradation and photoisomer production. Pediatr Res 85, 865–873 (2019). https://doi.org/10.1038/s41390-019-0310-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0310-2
This article is cited by
-
Urinary lumirubin excretion in jaundiced preterm neonates during phototherapy with blue light-emitting diode vs. green fluorescent lamp
Scientific Reports (2023)
-
Action spectrum of phototherapy in hyperbilirubinemic neonates
Pediatric Research (2022)
-
Characteristics of bilirubin photochemical changes under green light-emitting diodes in humans compared with animal species
Scientific Reports (2021)
-
Effect of blue LED phototherapy centered at 478 nm versus 459 nm in hyperbilirubinemic neonates: a randomized study
Pediatric Research (2021)
-
Blue or green for yellow? Which light is more beneficial for jaundiced newborns?
Pediatric Research (2019)