Abstract
Background
There are critical gaps in our understanding of the temporal relationships between metabolites and subsequent asthma development. This is the first study to examine metabolites from newborn screening in the etiology of early childhood wheezing.
Methods
One thousand nine hundred and fifty one infants enrolled between 2012 and 2014 from pediatric practices located in Middle Tennessee in the population-based birth cohort study, the Infant Susceptibility to Pulmonary Infections and Asthma Following RSV Exposure Study (INSPIRE), were linked with metabolite data from the Tennessee Newborn Screening Program. The association between the levels of 37 metabolites and the number of wheezing episodes in the past 12 months was assessed at 1, 2, and 3 years of life.
Results
Several metabolites were significantly associated with the number of wheezing episodes. Two acylcarnitines, C10:1 and C18:2, showed robust associations. Increasing levels of C10:1 were associated with increasing number of wheezing episodes at 2 years (OR 2.11, 95% CI 1.41–3.17) and 3 years (OR 2.56, 95% CI 1.59–4.11), while increasing levels of C18:2 were associated with increasing number of wheezing episodes at 1 year (OR 1.38, 95% CI 1.12–1.71) and 2 years (OR 1.47, 95% CI 1.17–1.84).
Conclusions
Identification of specific metabolites and associated pathways involved in wheezing pathogenesis offer insights into potential targets to prevent childhood asthma morbidity.
Similar content being viewed by others
Background
Childhood asthma is a serious chronic condition that incurs long-term medical and financial burdens for affected children and their families. Asthma is one of the most common chronic childhood diseases, affecting 7 million children in the United States alone.1 Asthma is the result of gene-by-environment interactions resulting in a disease that is characterized by inflammation and reversible airflow obstruction with symptoms that include coughing, wheezing, shortness of breath, and tightness in the chest.2 Evidence indicates that maternal environmental exposures including diet, obesity, tobacco smoke, and stress during pregnancy are strongly associated with asthma development in the child.3,4,5
While steps can be taken to control the disease and prevent its symptoms, no effective strategies for the prevention of asthma development are currently available and there is no cure.1, 2 While decades of research have focused on identifying risk factors for childhood asthma, few biological markers that predict who will develop asthma in childhood have been identified.6 Developing non-invasive predictive models of asthma risk in infants and preschoolers is critical as standard diagnostic testing using sputum inflammatory markers and lung-function testing are labor intensive and impractical in young children.7, 8
Metabolomics, the systematic analysis of molecular products of metabolism that drive cellular functions, provides insights into the underlying mechanisms of complex chronic diseases.6, 9 Metabolic profiles encompass genetic and environmental interactions, which makes this approach ideal for elucidating the biologic mechanisms of asthma.6 In a recent review summarizing the results of 21 existing metabolomic studies of asthma in humans, metabolites involved in pathways related to hypoxia response, oxidative stress, immunity, inflammation, lipid metabolism, and the tricarboxylic acid cycle were identified as significant.6 While findings from these studies are promising, their inability to assess temporal relationships between metabolites and subsequent asthma development limits their value in prediction modeling and clinical translation.
Newborn metabolic screening, a public health initiative aimed at screening every infant at birth for endocrine disorders, hemoglobinopathies, and inborn errors of metabolism, captures a variety of biomarkers involved in beta oxidation, amino acid and fatty acid metabolism, and mitochondrial dysfunction. Because these same pathways have been implicated in asthma pathogenesis,10, 11 newborn metabolic screening serves as an untapped resource to identify biomarkers for use in asthma prediction. To our knowledge, this is the first study to examine mitochondrial and metabolic dysfunction, represented by metabolites from newborn screening, in the etiology of early childhood respiratory illness.
The objective of this study was to determine whether newborn screening metabolites are associated with wheezing later in childhood, an early marker of asthma. Identifying specific metabolites and pathways involved in asthma pathogenesis may offer insights into potential preventive and therapeutic targets in early childhood to those susceptible, from birth, to respiratory illnesses.
Methods
Study population
We examined the association of newborn screening metabolite levels with wheezing at 1, 2, and 3 years of age in the Infant Susceptibility to Pulmonary Infections and Asthma Following RSV Exposure Study (INSPIRE), a birth cohort of term, healthy infants followed longitudinally from infancy through early childhood for the outcomes of wheezing illnesses and asthma.12 Over 1900 infants were enrolled over a 2-year period (June 2012–March 2014) from pediatric practices located in Middle Tennessee or self-referral through research announcements. Inclusion criteria for enrollment in the INSPIRE study included singleton birth, gestational age ≥37 weeks, and birth weight ≥2250 g (5 pounds). Exclusions included infants needing mechanical ventilation prior to enrollment, those with significant cardiopulmonary disease, bronchopulmonary dysplasia, cystic fibrosis, immunodeficiency (including maternal HIV), neurological disease, and those with any other significant health condition. Participants will continue to be followed to age 6–8 years, when asthma diagnosis will be ascertained.12 All parents provided informed consent, and the study was approved by the Vanderbilt University Medical Center, the Tennessee Department of Health, and University of Iowa Institutional Review Boards.
Baseline questionnaires were administered by trained study staff at the enrollment visit. The questionnaire included demographic characteristics, infant medical history, family history, secondhand smoke exposure, daycare attendance, growth trajectory, and other factors known to be associated with childhood asthma and allergy development. Annual follow-up visits were conducted year 1, year 2, and year 3, with longitudinal follow-up ongoing. The follow-up visits for years 1 and 3 were conducted in-person by research staff members, while the visit for year 2 was conducted by telephone survey. These visits included assessment of the outcomes of wheezing, including the International Study of Asthma and Allergy in Children (ISAAC) questionnaire13 and other allergic disease questionnaires in addition to biological sample collection (for in-person visits).12
Metabolite data collection
The Tennessee Newborn Screening Program of the Tennessee Department of Public Health provided the metabolic screening data that were linked to the INSPIRE birth cohort. All infants born in the State of Tennessee are screened for certain conditions, including phenylketonuria, hypothyroidism, galactosemia, and other metabolic/genetic defects that would result in intellectual disability or physical dysfunction as determined by the department.14 Thirty seven metabolites were measured on all subjects from dried blood spot specimens collected at birth as part of routine newborn screening by the Tennessee State Laboratory following standard procedures (https://www.tn.gov/content/dam/tn/health/documents/Tennessee_Newborn_Screening_Program_Information_Toolkit.pdf). These metabolites included: free carnitine, 21 acylcarnitines, 11 amino acids, 2 enzymes (biotinidase and galactose-1-phosphate uridyl transferase [GALT]), and 2 hormones (thyroid-stimulating hormone [TSH] and 17-hydoxyprogesterone [17-OHP]) (Supplemental Table S1 [online]). Uridyl transferase enzyme activity and total galactose (GALT) was measured by the quantitative enzymatic fluorometric method. Biotinidase activity was determined by the colorimetric method, a semiquantitative analysis of dried blood spots. TSH and 17-OHP were measured by the quantitative fluoroimmunoassay method. Amino acids and acylcarnitines were analyzed quantitatively by automated electrospray ionization tandem mass spectrometry. Metabolites were detected by their mass-to-charge ratio.
Thirty seven infants had more than one dried blood spot specimen collected. Blood spots were recollected for seven infants due to primary collection occurring outside of the acceptable time frame (>24 h from birth and <10 days from collection). For these seven infants, metabolite measurements from the second specimen were used in the analyses. For the remaining 30 infants who had >1 viable sample collected, the average value of each metabolite was calculated and used in the analyses.
Primary study outcome
The primary study outcome was wheezing ascertained at 1, 2, and 3 years of age. Wheezing was defined as the number of wheezing episodes the child had experienced in the past 12 months. This variable was defined using the ISAAC in 4 ordered categories, as no wheezing, 1–3 episodes, 4–12 episodes, or >12 episodes.13
Statistical analysis
Statistical analyses were conducted using the SAS 9.4 software (SAS Institute, Cary, NC). Each metabolite was natural log transformed to meet regression assumptions. Correlation between all pairs of carnitines (acyl and free) was assessed using the Spearman (non-parametric) rank correlation (Supplemental Table S2 [online]). To address the correlation among metabolites of similar chain length, metabolites were grouped into short-, medium-, and long-chain aggregate measures using methods described by Chace et al.15 Total carnitine (TC) was defined as the concentration of all acylcarnitines measured plus free carnitine (C0). The short-chain (SC) index was defined as the sum of the concentrations of C2, C3, C4, C5, and C5:1 divided by TC. Similarly, the medium-chain (MC) index was defined as the sum of the concentrations of C6, C8, C10, C10:1, and C10:2 divided by TC, and the long-chain (LC) index was comprised by sum of C14, C14:1, C16, C16:1, C18, C18:1, and C18:2 divided by TC. Total hydroxyl (total OH) included the sum of the LC hydroxyacylcarnitines (C14-OH, C16-OH, and C18:1-OH). Results are presented for both individual and grouped metabolites.
The association between newborn screening metabolite levels and the ordered wheezing outcome was assessed at 1, 2, and 3 years of age using separate ordinal logistic regression models (proportional odds model). We evaluated the proportional odds assumption by plotting the cumulative logits and visually inspecting whether their parallelism and regression assumption was valid for the independent covariates tested.16 Metabolites found to be significantly associated, after Bonferroni correction (p < 0.001), with number of wheezing episodes in the past 12 months for the 1-year, 2-year, and 3-year study outcomes in the univariate analysis were included in a multivariable logistic regression model including asthma risk factors and potential confounders (gender, ethnicity, race, delivery type, maternal asthma diagnosis, maternal smoking, other household smokers, primary insurance enrollment, and daycare attendance in first year of life) to assess the added value of the metabolite in predicting future wheezing. To assess the effect of metabolites on wheezing longitudinally over the course of the 3-year follow-up period, a proportional-odds generalized estimating equation model was fit using a robust sandwich variance estimator to account for correlated measures. This analysis was performed among individuals for whom all 3 years of follow-up data were available (n = 1280).
A secondary analysis was performed to compare metabolite levels at birth between the most extreme phenotypic groups at 1, 2, and 3 years of age. For this analysis, wheezing was dichotomized to include only those who never experienced a wheezing episode and those who experienced >4 wheezing episodes in the past 12 months. Univariate logistic regression was used to compute odds ratios (ORs) and the corresponding p values and 95% confidence intervals (CIs).
Results
Our cohort consisted of 1951 infants enrolled in the INSPIRE study and followed over a 3-year period (Table 1). The participant response rate was 90, 86, and 69% for years 1, 2, and 3 (Table 2). The percentage of participants reporting an absence of wheezing episodes over the 3-year period increased from 73.3 to 79.3%, while the percentage of participants reporting >12 wheezing episodes decreased from 1.8 to 0.8%, respectively.
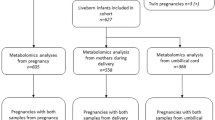
Newborn screening records were successfully linked to 1895 (97.1%) of the infants. Several metabolites were individually associated with the number of wheezing episodes in the past 12 months for the 1-year, 2-year, and 3-year study outcomes (Fig. 1, Supplemental Tables S3-S6 [online]), including C10:1 and C18:2 acylcarnitines, which remained significant after Bonferroni correction (p < 0.001). Increasing levels of C10:1 were associated with increasing number of wheezing episodes at 2 years (OR 2.11, 95% CI 1.41–3.17) and 3 years (OR 2.56, 95% CI 1.59–4.11) of age, while increasing levels of C18:2 were associated with increasing number of wheezing episodes at 1 year (OR 1.38, 95% CI 1.12–1.71) and 2 years of age (OR 1.47, 95% CI 1.17–1.84). The association between levels of C10:2 and number of wheezing episodes at years 1, 2, and 3 closely tracked those observed for C10:1, although the results were not significant after Bonferroni correction. Distributions of C10:1 and C18:2 with outcomes at years 1, 2, and 3 are depicted in Supplemental Figure S1 [online]. Summary measures of metabolites (SC, MC, LC, and total OH) were not significantly associated with the number of wheezing episodes.
The association between C10:1 and the number of wheezing episodes at 2 and 3 years of age remained significant after adjustment for asthma risk factors and potential confounders, including gender, ethnicity, race, delivery type, maternal asthma diagnosis, maternal smoking, other household smokers, primary insurance enrollment, and daycare attendance, in first year of life. Higher C18:2 levels were still associated with a greater number of wheezing episodes at 1 and 2 years of age, although this association was no longer statistically significant after adjusting for covariates (Table 3).
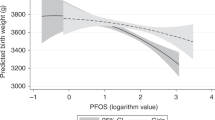
To assess the overall effect of newborn metabolites on wheezing over the course of the 3-year follow-up period, a longitudinal analysis was performed (Fig. 2). In this analysis, C10:1 levels at birth were strongly associated with an increase in the overall number of wheezing episodes combined across all 3 years (p = 0.0003), while C18:2 was moderately associated with wheezing (p = 0.02). However, these effects did not remain constant over time. The effect for C10:1 increased substantially over time, with its largest effect seen for wheezing at year 3. On the other hand, the association between C18:2 and wheezing was strongest in years 1 and 2 and significantly diminished at year 3.
A secondary analysis was performed to assess differences in metabolite levels at birth between the most extreme phenotypic wheezing groups (those who never experienced a wheezing episode and those who experienced >4 wheezing episodes in the past 12 months) at 1 year, 2 years, and 3 years of age (Supplemental Table S7 [online]). Decreasing levels of LC acylcarnitines were marginally associated with a decrease in the odds of experiencing >4 wheezing episodes in the past 12 months at 1 year. Many metabolites were marginally associated with an increase in the odds of experiencing >4 wheezing episodes in the past 12 months at 2 and 3 years of age. Analogous with the primary findings, C10:1 was significantly associated, after Bonferroni correction, with an increase in odds of experiencing >4 wheezing episodes in the past 12 months at year 2 (OR 4.30, 95% CI 2.08–8.90).
Discussion
Main findings
This study examined the association between targeted newborn screening metabolites and the risk of wheezing in childhood. Several metabolites were associated with the number of wheezing episodes in the past 12 months at 1, 2, and 3 years of age. This association was strongest among C10:1 and C18:2 acylcarnitines, where increasing levels at birth corresponded with increasing number of wheezing episodes in childhood. While the association between C18:2 and wheezing diminished after adjustment for asthma risk factors and potential confounders, C10:1 remained highly significant. Furthermore, C10:1 was also most strongly associated with wheezing in older children (age 3 years), suggesting that this metabolite could prove valuable in predicting asthma risk.
Interpretation
Asthma is a complex multifactorial disease characterized by altered lung function, airway hyper-responsiveness, airway narrowing, and inflammation.17, 18 Owing to its complexity, many pathways have been implicated in asthma pathogenesis, including pathways reflecting increased lipid metabolism and oxidative stress response. Lipid mediators and acylcarnitines (i.e., fatty acids) play a key role in the inflammatory responses in asthma.6 Low concentrations of fatty acids can influence the proliferation of T cells, while higher concentrations have been shown to induce apoptosis in a dose-dependent manner.19 The degree and length of the fatty acid also contributes to the level of apoptosis that occurs, with highly unsaturated fatty acids being most toxic even in low concentrations.19 Results from a recent study focusing on the role of oxidative stress in the modulation of asthma severity observed a high number of carbon double bonds (i.e., unsaturation) in the identified metabolites, suggesting that lipid peroxidation may be a driving force in asthma severity.11 We observed significant associations between increasing levels of two longer-length, unsaturated fatty acids and childhood wheezing. This is consistent with previous findings of positive associations between LC polyunsaturated fatty acid concentrations and asthma diagnosis in young adults.20
Evidence supporting the role of oxidative stress in asthma pathogenesis is strong. Reactive oxygen species (ROS) are produced as a result of normal metabolic processes and are essential in many physiological reactions.21 Increased exposure of airway cells and tissues to ROS as a result of environmental pollutants, infections, inflammatory reactions, or decreased levels of antioxidants can have deleterious effects. Damage to mitochondrial DNA, lipids, proteins, and carbohydrates as the result of increased ROS exposure may lead to impaired cellular functions and enhanced inflammatory reactions. Alterations in these pathways can lead to the chronic airway inflammation that characterizes asthma.21 Our findings support the concept that those with mild metabolic disturbances at birth will be more prone to mitochondrial dysfunction and development of chronic conditions, such as asthma, later in childhood when exposed to triggers in the environment or to other stressors.
We and others have previously shown that prenatal exposures, such as parental smoking, outdoor air pollution, and maternal stress, are consistently associated with childhood wheezing illness.22 The epigenome, a multitude of non-genetic chemical compounds that regulate genome structure and function,23, 24 is most susceptible to dysregulation in utero. The dynamic stages of fetal growth represent a period of vulnerability to epigenetic changes that can have major implications on the health of the child.25 We posit that the newborn screening metabolites identified through this analysis could serve as biomarkers of in utero mitochondrial dysfunction and epigenetic changes generated by prenatal exposures. Identification of specific metabolites and pathways involved in asthma pathogenesis could lead to potential therapeutic targets and strategies for targeted preventive interventions in pregnancy and early childhood to those who are most susceptible.
Strengths and Limitations
Newborn screening data represent a novel and unexplored resource for examining early life metabolic alterations in the etiology of childhood asthma. One limitation of current metabolomics studies of asthma is determining how the metabolites identified contribute to asthma etiology. For example, it is unclear whether metabolic differences indicate underlying metabolic and mitochondrial dysfunction that contributes to early childhood respiratory and allergy symptoms, and eventually the development of asthma, or if abnormal metabolite levels are simply a consequence of the condition itself. To our knowledge, this is the first study to examine mitochondrial and metabolic dysfunction, represented by metabolites from newborn screening, in the etiology of early childhood respiratory illness.
There are additional advantages to using newborn metabolic screening data. Because the State of Tennessee Department of Health requires newborn screening testing (as is the case with all US states), samples are collected and processed in a uniform manner for virtually every newborn born in the state. This allowed us to link nearly all INSPIRE cohort participants with metabolite data, limiting issues related to missing data and laboratory-related measurement bias.
While our findings add considerably to this field of research, we must acknowledge some limitations of our study. Our primary outcome, wheezing at 1, 2, and 3 years of age, was based on parental report, which could lend itself to bias. However, this variable was based on questions from an internationally standardized and validated questionnaire (ISAAC), increasing its reliability. Because longitudinal follow-up for the INSPIRE study is presently ongoing, information on asthma diagnosis has not yet been ascertained and thus could not be assessed in the present study. We intend to extend our present analysis to further assess the relationship between newborn screening metabolites and asthma diagnosis once 6–8-year follow-up has been completed. By utilizing a conservative Bonferroni method, we were able to control for multiple testing. However, as this method favors the detection of strong main effects, we may have missed weaker associations and those that are revealed via interactions.
The use of newborn screening data, while novel, offers limited metabolic profiling. Our future work will focus on integrating a broader range of untargeted metabolites with other “omic” strategies to identify the interactions and synergisms between biological pathways that will be necessary to fully characterize the complex etiology of asthma and reveal therapeutic targets for primary prevention.6, 11
Conclusion
This study leveraged newborn screening data to assess the relationship between newborn screening metabolites and the risk of wheezing in childhood, an early asthma phenotype, in a novel and exploratory approach. We identified metabolites that are available for every newborn that could be of value for identifying children at risk for asthma development. Before clinical translation can be executed, further integration of a broader range of metabolites and other “omic” data is necessary. Identification of specific metabolites and pathways involved in asthma pathogenesis is imperative to both the increased understanding of the underlying biology of asthma and to the development of clinical prediction models for targeted prevention in pregnancy and early childhood.
References
Akinbami L. J., et al. Trends in asthma prevalence, health care use, and mortality in the United States, 2001-2010. NCHS Data Brief 1–8 (2012).
National Institutes of Health. Guidelines for the Diagnosis and Management of Asthma: National Heart, Lung, and Blood Institute, National Institutes of Health. NIH Publication No. 07-4051 (National Institutes of Health, Bethesda, 2007).
Forno, E., Young, O. M., Kumar, R., Simhan, H. & Celedon, J. C. Maternal obesity in pregnancy, gestational weight gain, and risk of childhood asthma. Pediatrics 134, e535–e546 (2014).
Simons, E., To, T., Moineddin, R., Stieb, D. & Dell, S. D. Maternal second-hand smoke exposure in pregnancy is associated with childhood asthma development. J. Allergy Clin. Immunol. Pract. 2, 201–207 (2014).
Douros, K. et al. Prenatal maternal stress and the risk of asthma in children. Front. Pediatr. 5, 202 (2017).
Kelly, R. S. et al. Asthma metabolomics and the potential for integrative omics in research and the clinic. Chest 151, 262–277 (2017).
Beydon, N. et al. An official American Thoracic Society/European Respiratory Society statement: pulmonary function testing in preschool children. Am. J. Respir. Crit. Care Med. 175, 1304–1345 (2007).
Fleming, L., Tsartsali, L., Wilson, N., Regamey, N. & Bush, A. Sputum inflammatory phenotypes are not stable in children with asthma. Thorax 67, 675–681 (2012).
Johnson, C. H., Ivanisevic, J. & Siuzdak, G. Metabolomics: beyond biomarkers and towards mechanisms. Nat. Rev. Mol. Cell Biol. 17, 451–459 (2016).
Loureiro, C. C. et al. Urinary metabolomic changes as a predictive biomarker of asthma exacerbation. J. Allergy Clin. Immunol. 133, 261-263.e1–e25 (2014).
Fitzpatrick, A. M., Park, Y., Brown, L. A. & Jones, D. P. Children with severe asthma have unique oxidative stress-associated metabolomic profiles. J. Allergy Clin. Immunol. 133, 258-261.e1–e8 (2014).
Larkin, E. K. et al. Objectives, design and enrollment results from the Infant Susceptibility to Pulmonary Infections and Asthma Following RSV Exposure study (INSPIRE). BMC Pulm. Med. 15, 45 (2015).
Asher, I. ISAAC International Study of Asthma and Allergies in Childhood. Pediatr. Pulmonol. 42, 100 (2007).
Tennessee Newborn Screening Program Guide for Practitioners. State of Tennessee Department of Health. https://www.tn.gov/health/section/newborn-screening.
Chace, D. H. et al. Electrospray tandem mass spectrometry for analysis of acylcarnitines in dried postmortem blood specimens collected at autopsy from infants with unexplained cause of death. Clin. Chem. 47, 1166–1182 (2001).
Derr, B. Paper 446-2013: Ordinal Response Modeling with the LOGISTIC Procedure (SAS Institute Inc., Cary, NC, 2013).
Lambrecht, B. N. & Hammad, H. The immunology of asthma. Nat. Immunol. 16, 45–56 (2015).
Anderson, G. P. Endotyping asthma: new insights into key pathogenic mechanisms in a complex, heterogeneous disease. Lancet 372, 1107–1119 (2008).
de Jong, A. J., Kloppenburg, M., Toes, R. E. & Ioan-Facsinay, A. Fatty acids, lipid mediators, and T-cell function. Front. Immunol. 5, 483 (2014).
Woods, R. K., Raven, J. M., Walters, E. H., Abramson, M. J. & Thien, F. C. Fatty acid levels and risk of asthma in young adults. Thorax 59, 105–110 (2004).
Henricks, P. A. & Nijkamp, F. P. Reactive oxygen species as mediators in asthma. Pulm. Pharmacol. Ther. 14, 409–420 (2001).
Rosas-Salazar, C. & Hartert, T. V. Prenatal exposures and the development of childhood wheezing illnesses. Curr. Opin. Allergy Clin. Immunol. 17, 110–115 (2017).
Park, M., Keung, A. J. & Khalil, A. S. The epigenome: the next substrate for engineering. Genome Biol. 17, 183 (2016).
Epigenomics Fact Sheet. National Human Genome Research Institute, NIH, 2016. (Accessed 12 Oct 2017 at https://www.genome.gov/27532724/epigenomics-fact-sheet/)
Perera, F. & Herbstman, J. Prenatal environmental exposures, epigenetics, and disease. Reprod. Toxicol. 31, 363–373 (2011).
Acknowledgements
Thanks to the staff at the TN DOH and newborn metabolic screening program laboratory. This research is supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R21 HD-087864) and K24 AI 077930. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Donovan, B.M., Ryckman, K.K., Breheny, P.J. et al. Association of newborn screening metabolites with risk of wheezing in childhood. Pediatr Res 84, 619–624 (2018). https://doi.org/10.1038/s41390-018-0070-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0070-4
This article is cited by
-
Newborn screen metabolic panels reflect the impact of common disorders of pregnancy
Pediatric Research (2022)
-
Newborn metabolic vulnerability profile identifies preterm infants at risk for mortality and morbidity
Pediatric Research (2021)
-
Predicting childhood asthma development: are early life metabolite levels the philosopher’s stone to unlock the puzzle?
Pediatric Research (2018)